File

The Blood
Objectives
By the end of this lecture you should be able to
• Describe the composition of Blood
• Describe composition of Plasma and Types of Cells
Present [RBC, WBC, Platelets]
• List the normal Values for Hb, RBC, WBC, PLT
• Define Anemia, Polycythemia, Leukocytosis, Leukopenia,
Thrombocytosis, Thrombocytopenia
• List the different types of the blood Vessels(Arteries
,Arterioles – resistance, Capillaries, Veins)
• Define blood Pressure, Hyper tension, Hypo tension
• Define normal Heart rate
Blood
• Represents about 8% of total body weight
• Average volume
•
5 liters in women
•
5.5 liters in men
Composition of the blood
• Plasma: fluid part, 55% of total blood volume.
• Cellular elements: 45% of total blood volume.
• RBC or erythrocytes
-men 5.4 million/mm 3
-women 4.8 million /mm 3
• Hb concentration:
– men 16 g/dl
– women 14 g/dl
WBC or leukocytes 4000-11000/mm3
• Platelets or 150,000-400,000 /mm3
Blood Composition
Hematocrit or packed cell volume :
% of total blood volume occupied by RBCs.
Blood
• Consists of 3 types of specialized cellular elements suspended in plasma (liquid portion of blood)
– Erythrocytes
• Red blood cells ( contains hemoglobin)
• Important in O
2
– Leukocytes transport
• White blood cells
• Immune system’s mobile defense units
– Platelets
• Cell fragments
• Important in hemostasis(they prevent blood loose from damaged blood vessels).
DIFFERENT TYPES OF WBC &
THEIR FUNCTIONS
WBC
1. Neutrophil (60-70%)
FUNCTION
Phagocytosis (engulf bacteria)
2. Eosinophil (1-4%)
3. Basophil (0.5-1%)
Important in allergic reactions
Important in allergic reactions and have heparin
4. Lymphocytes (25-33%)
5. Monocyte (2-8%)
For immunity
Tissue macrophage
PLASMA
• Plasma is transport medium for inorganic and organic substances.
• Plasma Composition:
Water – 90%
Solids – 10 %
Electrolytes [1%]– mainly Na + , Cl , K + , HCO
3
Plasma protein [6-8%]
, Ca 2+
Organic Substances - Glucose, Amino acids, Lipids,
Vitamins
Waste products – urea, creatinine
Dissolved gases – O
2
Hormones and CO
2
Plasma
• Plasma proteins
– Compose 6% to 8% of plasma’s total weight
– 3 groups of plasma proteins
• Albumins
– Most abundant plasma proteins
• Globulins
– 3 subclasses
» Alpha (α)
» Beta (β)
» Gamma (γ)
• Fibrinogen
– Key factor in blood clotting
Most of the plasma protein are synthesized in liver.
Functions
Plasma
Constituent
Water (makes up
90% of plasma)
Electrolytes
Alpha and beta globulins
Transport medium, carries heat
Nutrients, wastes, gases, hormones
Membrane excitability; osmotic distribution of fluid between
ECF and ICF; buffer pH changes
Transported in blood; blood gas CO base balance
2 plays role in acid-
Plasma proteins In general, exert an osmotic effect important in distribution of ECF between vascular and interstitial compartments; buffer pH changes
Albumins Transport many substances; contribute most to colloid osmotic pressure
Transport many water-insoluble substances; clotting factors; inactive precursor molecules
Gamma globulins Antibodies
Fibrinogen Inactive precursor for the fibrin meshwork of a clot
CLINICAL APPLICATION
• Anemia – decrease in RBC & Hb
• Polycythemia – increase in RBC & Hb
• Leukocytosis – increase in WBC count (more than
11,000 /mm3
• Leukopenia – decrease in WBC count (less than 4000
/mm3
• Thrombocytosis – increase in platelet count
• Thrombocytopenia – decrease in platelet count
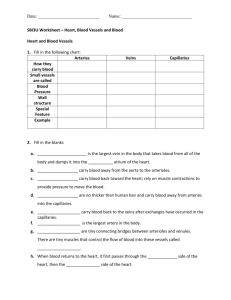
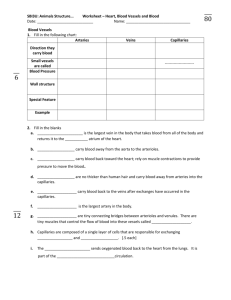
BLOOD VESSELS
Basic Organization of the Cardiovascular
System
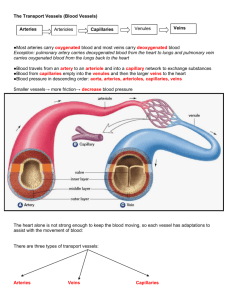
Vascular Tree
• Consists of
– Arteries
• Carry blood away from heart to tissues
– Arterioles
• Smaller branches of arteries
– Capillaries
• Smaller branches of arterioles
• Smallest of vessels across which all exchanges are made with surrounding cells
– Venules
• Formed when capillaries rejoin
• Return blood to heart
– Veins
• Formed when venules merge
• Return blood to heart
Arteries
• Specialized to
– Serve passageways for blood from heart to organs
• Due to large radius, arteries offer little resistance to blood flow
– Act as pressure reservoir to provide driving force for blood when heart is relaxing
– Has thick, highly elastic wall.
• Arterial connective tissue contains
– Collagen fibers
» Provide tensile strength
– Elastin fibers
» Provide elasticity to arterial walls
Arteries as a Pressure Reservoir
Blood Pressure
Blood pressure averages
120 mm Hg during systole ( systolic pressure )
80 mm Hg during diastole ( Diastolic pressure )
the difference between systolic & diastolic pressures is called the pulse pressure )
Hypertension: increase in Blood pressure
Hypotension: decrease in Blood pressure
Arterioles
• Major resistance vessels
• Arterioles are highly muscular (smooth muscle).
• Have no elastic fiber.
• Radius supplying individual organs can be adjusted independently to
– Distribute cardiac output among systemic organs, depending on body’s momentary needs
– Help regulate arterial blood pressure
Arterioles
• Mechanisms involved in adjusting arteriolar resistance
– Vasoconstriction
• Refers to narrowing of a vessel
– Vasodilation
• Refers to enlargement in circumference and radius of vessel
• Results from relaxation of smooth muscle layer
• Leads to decreased resistance and increased flow through that vessel
Arteriolar Vasoconstriction and Vasodilation
Capillaries
• Thin-walled, small-radius, extensively branched
• Sites of exchange between blood and surrounding tissue cells
• Narrow, water-filled gaps (pores) lie at junctions between cells
• Permit passage of water-soluble substances
• Lipid soluble substances readily pass through endothelial cells by dissolving in lipid bilayer barrier
• Size of pores varies from organ to organ
Capillaries
Veins
• Venous system transports blood back to heart
• Capillaries drain into venules
• Venules converge to form small veins that exit organs
• Smaller veins merge to form larger vessels
• Veins
– Veins are thin walled as compared to arteries
– Large radius offers little resistance to blood flow
– Also serve as blood reservoir
– serve as a BLOOD RESERVOIR (under resting conditions nearly two-thirds of all your blood in located in the veins), they are called ‘CAPACITANCE
VESSELS’.
Lymphatic System
• Extensive network of one-way vessels
• Provides accessory route by which fluid can be returned from interstitial to the blood
Percentage of blood volume in different parts of circulatory system
References
•
Human physiology by Lauralee Sherwood, seventh edition
•
Text book physiology by Guyton &Hall,11
th
edition
•
Text book of physiology by Linda .s contanzo,third edition
29