Burning Issues with UTIs
advertisement
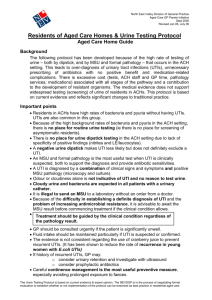
Burning Issues with UTIs Meghan Brett, MD Division of ID Hospital Epidemiologist Medical Director, Antimicrobial Stewardship Objectives • Distinguish between asymptomatic bacteriuria (ASB) and different types of active UTIs (complicated vs. uncomplicated) • Describe in which patients ASB should be treated • Learn how to diagnose a catheter-associated UTIs (CAUTIs) • Describe how to determine empiric treatment and how long uncomplicated UTIs should be treated • Know how to access and use various antibiograms and other resources What’s the Burden of UTIs? • 50% of women will have a UTI in their lifetime – Up to 25% may have a second UTI within 6 months • Visits related to UTI – – – – 3 million ED visits in 2010 Most common primary diagnosis for U.S. women visiting EDs 100,000 hospitalizations in U.S. 0.9% of all ambulatory visits • Half of all UTIs were among patients age 18 to 44 years • Pts visiting the ED have higher acuity than those pts presenting to primary care – 400,000 (13%) were for pyelo (13 visits/10,000 people) – In general population: 1 case/28 cases of cystitis Who is Most Affected by UTIs? • Annual Incidence of UTIs – – – – – – – – Young, sexually active women: 2 – 4% Women > 70 yrs: 5 – 10% Women > 80 yrs: 50% Institutionalized Women: 40% Adult men (childhood through middle age): < 1% Men > 65 yrs: 1 – 3% Men > 80 yrs: 10% Institutionalized Men: 25% • CAUTIs: ~1 million/year What Are Take Home Points? • Assemble the whole clinical picture (i.e., limiting reflexive Rx of positive Urine Cx) • Determine the syndrome • Distinguish between complicated vs. uncomplicated UTIs • Choose appropriate empiric antibiotics based on likely bacterial etiologies and their resistance • Adjust antibiotics based on culture results • Decide about length of therapy Questions (1st Set) • How do you define asymptomatic bacteriuria ASB? • How do you differentiate between asymptomatic bacteriuria and UTI? • Which groups need to be treated for ASB? • What criteria do you use to define uncomplicated vs. complicated UTIs? • Why does distinguishing uncomplicated vs. complicated help? • What kinds of questions would you ask to distinguish between uncomplicated and complicated? Asymptomatic Bacteriuria • Asx women: 2 consecutive voided urine specimens with isolation of same bacterial strain in quantitative counts ≥ 105 cfu/mL • Men: single, clean-catch voided specimen with 1 bacterial species isolated in quantitative counts ≥ 105 cfu/mL • Women or men: single catheterized specimen with 1 bacterial species isolated in quantitative count ≥ 102 cfu/mL Infectious Diseases Society of America (IDSA), ASB guidelines 2005 ASB • Evidence that screening and treatment does not lead to improved clinical outcomes • More likely, unnecessary antibiotics may cause harm – Adverse effects – C difficile infection – Antibiotic resistance – Wasted expense UTI Signs/Sx Clinical Presentation – Distinguishing ASB vx. UTI • Lower tract signs – Dysuria – Frequent urination – Urgent urination • DDX: – STIs – Vaginitis – Exposure to chemical or allergic irritants Clinical Presentation – Distinguishing ASB vx. UTI • Upper tract: – Fevers, chills – Nausea – Flank pain – Often also with dysuria/frequency/urgency Which Groups Require Rx for ASB? • Definitive: – Pregnant Women – Anyone undergoing TURP or Urologic procedures during which mucosal bleeding is anticipated • Maybe: – Renal transplant patients – Neutropenic patients Infectious Diseases Society of America (IDSA), ASB guidelines 2005 Uncomplicated vs. Complicated • Uncomplicated – premenopausal women – No structural or functional abnormalities in urinary tract – Not pregnant • Complicated – – – – – Structural abnormalities (e.g., nephrolithiasis) Functional abnormalities (e.g., ureteral reflux) Compromised hosts (e.g., pregnant, diabetic) UTIs in boys/men: until structural/functional ruled out IDSA, Uncomplicated UTI Guidelines 2011 Dielubanza EJ. ID Clin N Am 2014. Why Distinguish Between Uncomplicated vs. Complicated? • Guidelines for uncomplicated but none for complicated UTIs • More important than upper tract/lower tract • Complicated – May need further evaluation (diagnostics, urology consult) – Increased morbidity and mortality – May encounter more drug resistance (IV ABX) – Duration of therapy will likely be longer • Assess conversion from uncomplicated to complicated (may indicated underlying issues) Questions to Distinguish Uncomplicated from Complicated • • • • • • • • • Pregnancy status History of kidney stones Structural/functional GU abnormalities Pelvic surgery DM Neurologic disorders Recent ABX use Recent hospitalization Recent GU instrumentation Questions (2nd Set) • What’s the best way to obtain a urine sample for diagnosing a UTI? • What are indications for having a Foley catheter? • What tests do you review on a urinalysis to make you consider a UTI? ASB? • How do you diagnose a CAUTI? Key Issue – Urine Sample Collection • Clean-catch, mid-stream = best • In/Out catheterization • DO NOT insert Foley catheters for sake of urine collection (unless otherwise indicated) Indications for Foley Catheters • Patients with hemodynamic instability (e.g., on pressors) who require urine output monitoring • Urinary obstruction/retention • Sacral or perineal wounds in patients with incontinence • Genitourinary surgery/Placed by a Urologist • Requires prolonged immobilization (unstable spine) • End of life care CDC (HICPAC) CAUTI Prevention Guidelines, 2009 http://www.cdc.gov/HAI/ca_uti/uti.html Review of UA for Evidence of Infection • Check squamous cells first… if > 20, likely a contaminated sample • Nitrites – Produced by many Gram-negatives – Requires hours for conversion of nitrate nitrite – Not by Gram-positives, candida species • WBCs – > 10 per high powered field • Leukocyte esterase – Enzyme found in neutrophils – If present, indicates neutrophil activity Caveats • Pyuria in ASB does not need to be treated • Urine samples that sit will have alterations in UA results – Samples analyzed within 2 hours or refrigerated to limit false positive and false negative results Questions (3rd Set) • How do you select an antibiotic for empiric treatment treatment? • When do you change from empiric to directed antibiotic therapy? • How long do you treat uncomplicated cystitis? Uncomplicated pyelonephritis? • How do you treat CAUTIs? For how long? • Do you test urine for cure? Why? Treatment of UTIs – What Bugs? • Enteric flora colonizing perineum and urethra • E. coli – – – – 80% of first infection in women, men, children 50% of nosocomial UTIs Most common for acute uncomplicated cystitis Many episodes of complicated UTIs and pyelo • Staphylococcus saprophyticus – 11% of UTIs (sexually active, younger women) • Remaining – GNRs (Klebiella, Proteus mirabilis) increasingly MDROs – Gram-positive cocci (entercoccus and GBS) What’s First Line Therapy (Empiric Treatment)? – Uncomplicated Only! • Antimicrobial Stewardship Clinical Pathway (with a focus on inpatients) Change from Empiric to Directed? • When you have culture results • Look at susceptibility interpretations • Determine what has good urine/kidney penetration • Lowest MIC ≠ Best ABX selection • Questions? Call Antimicrobial Stewardship! (on amion.com) How Long to Treat? • It depends! • Uncomplicated UTIs – Cystitis • Nitrofurantoin or Bactrim 3 days • 20% resistance in isolates is an indication not to use this for empiric coverage • Note: nitrofurantoin should not be used in patients with Creatinine clearance < 50 (does not reach bladder) – Pyelonephritis • FQ 5 – 7 days • Beta-lactams 10 – 14 days • Bactrim 14 days How Long to Treat CAUTIs? • 7 days of treatment for patients with CAUTI who have prompt resolution of symptoms • 10 – 14 days in patients with delayed response to treatment • 3 day regimen may be considered for women ≤ 65 yrs who develop CAUTI without upper tract sx after a catheter has been removed Test of Cure? • Nope (please don’t) Other Notes • Complicated including CAUTIs – Polymicrobial for longer-term (>30d) indwelling catheters – More drug resistant (ESBLs, P. aeruginosa, or enterococcus faecium) • S. aureus – what to do? Treatment of CAUTIs • Algorithm to be developed Greatest Overuse of Antibiotics It’s ASB patient’s positive urine cx Unintended Consequences of ABX • Drug reactions • C difficile infections • Selection for drug resistance • Stay tuned… impact to the microbiome Resources ASP – Inpt Antibiograms and Clinical Pathways • https://hospitals.health.unm.edu/intranet/Ind ex.cfm • https://hospitals.health.unm.edu/intranet/ant imicrobial/pathways.shtml Tricore – Outpatient Antibiograms • http://www.tricore.org/HealthcareProfessionals/Test-Information/Antibiograms