Asymptomatic Urinary Tract Infection
advertisement

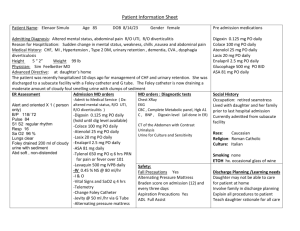
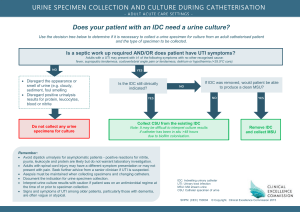
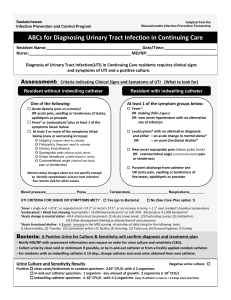
Asymptomatic Urinary Tract Infection Edward L. Goodman, MD October 13, 2003 A Common Problem: Prevalence of AB in Ambulatory Persons • • • • Young women: 1-2% Women >60 years: 6-10% Men >65 years: >5% Swedish city – At 72 years, 6% men, 16% women • VA outpatient men – 65-74 years old: 9% – 75-84 years old: 15.3% Nicolle. Inf Dis Clin NA, 1997; 11: 647 Elderly Institutionalized • Prevalence – Men: 15 – 35% – Women: 25 - 50% • Incidence Studies – NH with negative culture on admission • 11% men positive at one year • 23% women at one year – Another study: 10% acquire every 3 months Nicolle IDCNA 1997 So, it’s common- big deal! • We’ve got The Sanford Guide – – We can look it up conveniently Who needs a lecture? • For those of us who can’t read the small print – We’ve got Epocrates – Current house staff were all born with a Palm Pilot™ clutched in their palm! • What’s the big deal – just treat it! BUT • All antibiotic use ultimately leads to microbial resistance • Resistance results in increased morbidity, mortality, and cost of healthcare; and • Appropriate antimicrobial stewardship should prevent or slow the emergence of resistance among organisms (Clin Inf Dis 1997; 25:584-99.) • Antibiotics are used as “drugs of fear” (Kunin et al. Ann Int Med 1973;79:555) Antibiotic Misuse • Surveys reveal that: – 25 - 33% of hospitalized patients receive antibiotics (Arch Intern Med 1997;157:1689-1694) – 22 - 65% of antibiotic use in hospitalized patients is inappropriate (Infection Control 1985;6:226-230) Consequences of Misuse of Antibiotics • Contagious RESISTANCE – Nothing comparable for overuse of procedures, surgery, other drugs • Morbidity - drug toxicity • Mortality - MDR bacteria harder to treat • Cost Definitions: Asymptomatic Bacteriuria • “Gold standard” for bacteriuria = >=100,000 CFU/ml voided urine – Applied to Asymptomatic Bacteriuria – Almost always present in acute pyelonephritis – Kass, EH. Trans Assoc. Amer. Phys 69:56, 1956 Definitions: Symptomatic Bacteriuria • Acute cystitis in women: >= 100 CFU/ml – 95% sensitivity; 85% specificity* • Acute pyelonephritis: > 100,000/ml** • (The standard 0.001 ml loop cannot detect <1000 organisms/ml) • *Stamm WE. NEJM 3229:1328, 1982 • **Kass 1956 Infectious Disease Society Consensus Definition • Cystitis: >=10³ cfu/ml – Sensitivity 80%; Specificity 90% • Pyelonephritis: >=10,000 cfu/ml • Can be identified in routine micro labs using 0.001 ml loop • Rubin et al. Clinical Infectious Disease, 1992 Symptoms • Acute: irritation, obstruction or inflammation – correlate with significant bacteriuria • Chronic: incontinence, hesitancy, hematuria – do not correlate with bacteriuria in elderly • In demented: non-specific symptoms such as altered mentation are fairly sensitive for systemic infection Colonization vs. Infection • Bacteriuria is almost always associated with a host response – Pyuria – Cytokinuria • HENCE, THE TERM COLONIZATION OF URINE IS OBSOLETE. It is infection, asymptomatic or symptomatic Why So Many Urine Cultures? • Annually 10,400 urine cultures are submitted to the PHD Microbiology Laboratory – Exceeded only by 14,000 blood cultures • At least one third from catheterized patients – Often cath specimens are mislabeled as voided – It is an effort to obtain a clean catch urine from a hospitalized patient – Catheter urine is so convenient to culture! • Nursing preferences play a major role HCW’s Attitudes and Perceptions • HCW interpret bacteriuria as symptomatic in presence of nonspecific symptoms • Urine cultures are thus ordered for nonspecific changes in patient’s status – part of the “panculture” mentality • Difficulty in eliciting information about symptoms in frail elderly Attitudes and Perceptions –2 • Physician’s uncertainty about significance and management of positive urine culture • Liability concerns – A positive culture left untreated looks “bad” in the chart • Walker et al. CMAJ 2000; 163 (3): 273 Refrain: Prevalence of AB in Ambulatory Persons • • • • Young women: 1-2% Women >60 years: 6-10% Men >65 years: >5% Swedish city – At 72 years, 6% men, 16% women • VA outpatient men – 65-74 years old: 9% – 75-84 years old: 15.3% Nicolle, Inf Dis Clin NA, 1997 Refrain II: Elderly Institutionalized • Prevalence – Men: 15 – 35% – Women: 25 - 50% • Incidence Studies – NH with negative culture on admission • 11% men positive at one year • 23% % women at one year – Another study: 10% acquire every 3 months Nicolle 1997 Does Rx for AB Help? • All data is from elderly in long term care facilities • Early studies (Platt, NEJM 1982;307:637) suggested AB associated with three fold higher mortality – Therapy had no protective effect – AB seems to be a marker of debility • More recent comparative studies confirm no benefit from Rx and no higher mortality in non Rx Nicolle et al. NEJM Male veterans, 1983;309:1420 Average age 82 2 yrs: no difference in incidence of sx UTI, prevalence or mortality Nicolle et al. Am J Med 1987; 83:27 Women, NH, average age 83 1 yr: monthly prev. 31% down; incid. of sx UTI and mortality no diff; more ADR and MDR Abrutyn et al. Ann Intern Med 1994; 120: 827 Women, geriatric apartment, average 81 8 yr: mortality similar Ouslander et al. Ann Intern Med 1996; 122: 749 Incontinent NH both sexes No decrease in freq or volume of incontinence Case Presentation • 91 year old woman admitted from NH with fever, altered mental state and drainage from recent hip incision, no urinary sx • Urine culture from cath inserted in ER: >100,000 Pseudomonas aeruginosa • Diagnosis: “Urosepsis” – BUT Case continued • Blood and hip aspirate cultures: MRSA • No response to anti-pseudomonas Rx: still confused • Woke up with Vancomycin • Diagnoses: – Infected total hip with secondary bacteremia – MRSA – Asymptomatic bacteriuria - Pseudomonas Fever and UTI in Elderly Institutionalized • Prospective study – Jan 1, 1989 through Dec 31, 1990 – Two LTCF in Canada • Demographics – M:F 3:1 – Majority >65 years – Catheters 5.7% to 9.3% Nicolle, AJM 1996; 100:71. Fever and UTI in Elderly Institutionalized • Entry Criteria – Fever • Urine cultures, UA at enrollment and Q4 weeks • Monitored serum antibody – Major Outer Membrane Protein (MOMP) of E coli for all enterobacteriaceae – IgG to other organisms Fever and UTI in Elderly Institutionalized: Definitions • Fever >38 (100.4) • Sx UTI for non cath required at least 3: • • • • • Fever or chills* New or increased lower tract irritation New flank or suprapubic pain or tender Change in character of urine Worsening mental status* – *our case Definitions continued • Indwelling catheter: two symptoms – – – – Fever or chills New flank or suprapubic pain/tender Change in character of urine Worsening mental status • Bacteriuria – Non cath >= 100,000/ml of one or two bugs – Condom cath >=100,000 of <3 bugs – Cath: any number Febrile Morbidity in long term care patients • Prevalence of bacteriuria - 50% – <10% were catheterized • Positive Predictive Value of bacteriuria for clinical UTI – 11% • PPV of bacteriuria for serologic UTI – 12% • <10% of episodes of unexplained fever were attributable to UTI • Nicolle, AJM 1996; 100:71. To Summarize • Bacteriuria very common in uncatheterized long term care patients • Poor correlation of bacteriuria with symptoms attributable to urinary tract • Bacteriuria rarely explains fever in absence of localizing symptoms • Most treatment for AB is inappropriate Should AB ever be treated? • Pregnant women – AB Prevalence: 4-7% – Optimal time to screen is 16th week – Symptomatic infection develops in 20-40% of those with AB (1-3% of all pregnancies) – Premature labor in 20-50% with symptomatic UTI – Successful Rx of AB reduces rate of symptomatic UTI by 80-90% – Patterson TF, Andriole VT. Inf Dis Clin NA 1997;11:593-608 When to Rx AB – cont’d • Prior to renal transplant • Prior to invasive urinary procedures – TURP, biopsy prostate – not insertion of catheter (except if valvular heart disease and infected urine) • Unclear before insertion of non urinary prosthesis: heart valve, total hip or knee Case Presentation 2 • 39 woman, 250 pounds, three previous THR. No urinary sx. • Pre op: “dirty” voided UC: 30k E coli and Klebsiella • Three days of Cefamandole and Tobra starting at time of surgery • 6 weeks later, E coli in hip – Different biotypes and MIC’s Case 2 - continued • She sued the surgeon alleging negligence for replacing hip in setting of positive urine culture • Defense expert testified – the two organisms were unrelated – the literature didn’t support any increased risk of SSI from asymptomatic UTI* *Review of literature on urine cultures prior to hip surgery • Lawrence, Kroenke. Arch Int Med 1988; 148:1370-1373 – Chart review 200 consecutive knee procedures • Excluded insertion of prostheses – Criteria for abnormal UA established – 10% UA’s indicated, 90% not – SSI: 1/166 with normal UA; 0/23 with WBC • Overall infection rate 0.5% (95% CI: 0-2.3%) Literature - continued • Health Technology Assessment 1997; 1:4347 – No controlled trials on value of routine preop urine testing – Routine preop urine abnormal 1%-34.1% • Leads to change in management in only 0.1%-2.8%! – No good evidence that preop abnormal UA is associated with any postop complication Case - continued • Plaintiff’s expert stated “An E coli is an E coli is an E coli. Don’t bother me with genetics.” • SHE WON THE CASE! Catheter Associated UTI • • • • • Short term catheter <30 days Long term catheter >30 days Prevention of bacteriuria Prevention of complications of bacteriuria Avoidance of urethral catheters Warren Inf Dis Clin NA 1997; 11: 609-622 How Significant is Pyuria in Foley Urine? • Definition – Standard: 5 WBC/hpf – Hemocytometer: 10 WBC/µl • Does not correlate with catheter related symptomatic infection. • SHOULD NOT BE USED AS REASON TO OBTAIN FOLEY URINE CULTURE • Tambyah, Maki. Arch Int Med 2000; 160: 673 Short Term Catheter • 15-25% of acute care patients have catheter – Mean/median duration between 2 and 4 days – At 3% to 10% incidence/day, 10% to 30% will develop catheter associated bacteriuria (CAB) during their hospital stay –Warren Inf Dis Clin NA 1997; 11: 609-622 Risk Factors for CAB Platt. Am J Epid 1986; 124: 977 • • • • • • • • • Duration of catheter Absence of urinometer Colonization of drainage back/back flow Diabetes No receipt of antibiotics Female For other than surgery or output measures Abnormal serum creatinine Errors in catheter care Complications of Short Term Catheter • Most episodes of AB are asymptomatic • Fever or UTI sx in up to 30% – <5% associated with bacteremia – Attributable mortality <15% of bacteremic • Given large number of short term catheters nationwide, up to 15% of nosocomial bacteremias are from UTI PHD 2001 Survey Data courtesy of Sharon Williamson, MT(ASCP) and Bobby Moore, MT (ASCP) PHD Microbiology Lab • Review Micro Lab Computer for – All patients with positive urinary catheter culture and – Positive blood cultures drawn same day • Exclude urine positive for Staph aureus and Candida since – Literature states these are more likely causes of the bacteriuria rather than the consequence Cases with same isolate in BC/UC • Total 19 cases – 14 E coli – 2 Proteus mirabilis • 1 had three other urinary isolates as well – 2 Klebsiella pneumoniae – 1 Morganella morganii Cases with different isolates • 55 total cases – Skin flora in blood: 40 • Seven had 2 + BC for CNS – likely pathogens • 33 had single + BC – unclear significance – Definite pathogens in blood: 16 – Combined definite and likely: 23 cases Likelihood of Positive Foley Culture As Cause of “urosepsis” • 19/42 (45%) bacteremic episodes in this cohort of catheterized patients were attributable to urine isolate • 23/42 (55%) bacteremic episodes not related to urine isolate – would have been missed if therapy based on urine only! Conclusion • In an acute care hospital, cannot assume that a positive urine culture from catheterized patient is the cause of a febrile episode • Must always draw blood culture before initiating therapy • Keep an open mind about other sites for fever Long Term Catheters • Prevalence: more than 100,000 NH patients in USA • Incidence of bacteriuria still 3% to 10%/day • At 30 days, almost 100% prevalence! – 95% polymicrobial – Catheter bugs not the same as bladder bugs at least 25% of the time (biofilm theory) Complications of Long Term Catheters • Two thirds of febrile episodes in aged LTC attributed to UTI – Incidence: one febrile episode per 100 catheter days – MOST SELF LIMITED (<1 day) – Therapy not usually indicated Other Complications of LTC • Catheter obstruction – Related to biofilm production • Infection stones • Chronic renal inflammation – Chronic pyelo usually only with obstruction/stones • Urethritis/fistulae, epididymitis, prostatitis • Bladder cancer Prevention of CA Bacteriuria • Closed catheter system • Remove catheter when possible • Delay onset – Coated catheters largely ineffective – Systemic antibiotics work but ultimately • Adverse effects • Multidrug resistant isolates emerge Prevent Complications of CA Bacteriuria? • Search out and treat AB? – Prospective trial (Warren JAMA 1982;248:454) • no effect on preventing fever • Marked increase in resistance • DO NOT TREAT CAB except in – epidemics or clusters – High risk patients • Pregnancy, renal transplant, urologic surgery What about symptomatic UTI in catheterized patient? • Always look for non-UTI explanations as well – Blood cultures • Treat with specific therapy for 10-14 days assuming occult pyelonephritis – Change catheter and obtain new culture before Rx • Clinical and bacteriologic outcomes better • More reliable culture from newly inserted catheter with no biofilm – Raz. J Urol 2000;164:1254 What about Candiduria? • 10% of positive urine cultures in referral hospitals yield candida sp. • Symptomatic candiduria should be treated • What about catheter associated candiduria? – Short term eradication with 14 days fluconazole – No effect on candiduria two weeks after therapy – No effect on mortality Sobel. Clin Inf Dis 2000; 30:19 Recommendations for screening and treatment of AB Nicolle L.E. Infect Dis Clin N Am (2003): 367 • Screening and treatment beneficial – Pregnant women – Before traumatic genitourinary procedure • Screening and treatment may be beneficial – Renal transplant, first 6 month post-tranplant – Women with persistent cath-acquired bacteriuria after cath removal Screening and Treatment not beneficial Nicolle 2003 • • • • • • • • Healthy infants, children, adults Elderly in the community or long term care Women with diabetes HIV patients Patients with short or long term urinary catheters Patients with intermittent catheterization Patients with neurologic impairment of voiding Patients with chronic urologic devices Conclusions • Don’t seek out Asymptomatic Bacteriuria – Except in pregnant women, prior to renal transplant or invasive urologic procedures • Don’t assume that foley associated AB is cause of patient’s deterioration – Look for other causes even while you treat the UTI Conclusions 2 • Don’t bother with post treatment cultures • When Rx given for catheter associated UTI, change the catheter, obtain second culture and treat 10-14 days • Avoid use of drugs needed for treating other serious infections – Reduce risk of selection of resistance Thanks to the following persons for their assistance: • • • • • • Sharon Williamson, MT (ASCP) Bobby Moore, MT (ASCP) Tammy Chung, Pharm.D Carla Philmon, Pharm.D Teri Smith, Pharm.D Judith Marshall, R. Ph