pain3

Touch and Pain
Biological Foundations
Somatosensation
21 of 49
• Somatosensory receptors vary in complexity and stimuli that they respond to:
– Pacinian corpuscle detects sudden displacements or high-frequency vibrations on the skin
– Meissners corpuscles
• elaborate neuronal endings detect sudden displacement and low frequency vibrations on skin
Somatosensation
– free nerve endings detect pain, warmth and cold
– Ruffini endings detect stretch of skin
– Merkels disks detect indentation of skin
21 of 49
Somatosensation
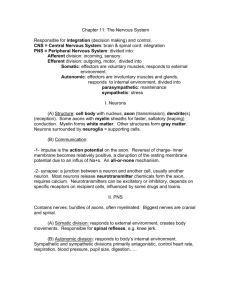
• Input to the spinal cord and the brain
– touch information from head enters CNS through cranial nerves
– below the head, information enters via 31 spinal nerves connecting to 31 dermatomes
22 of 49
Somatosensation
22 of 49
– sensory pathways to cortex remain separate
• Ex: two parallel strips respond to light touch, two others respond mostly to deep touch and movement of the joints and muscles
– somatosensory cortex receives input from the contralateral side of the body
Theories of Touch
• Von Frey’s specificity Theory
– Pressure: Meissner corpuscles
– Pain: free nerve endings
– Warmth: Ruffini endings
– Cold: Krause end bulbs
James W. Kalat Biological Psychology, 8th Edition
Figure 7.14
23 of 49
Figure 7.14 Dermatomes innervated by the 31 sensory spinal nerves. Areas I, II, and III of face are not innervated by the spinal nerves, but instead by three branches of the fifth cranial nerve. Although this figure shows distinct borders, the dermatomes actually overlap one another by about one-third to one-half of their width.
Touch
Most likely pathway to Somatosensory
Cortex receptors transduce environmental energy
Pacinian corpuscle: touch receptor elliptical shape large size
Touch
Fibers
A-beta: fast
A-delta: moderate (temp and pain)
C-fibers: slow conducting (temp and pain)
Touch: A Fibers
• A-beta fibers to spinal cord
– 2 ascending tracts
• Fasciculus grancilis (lower part of body)
• Fasciculus cureatus (upper body)
• Spinal cord to brain
– The spinal cord tract synapse and cross over in the medulla
– Information goes through the trigenimal nerve to the thalamus
– Relayed to the somatosensory cortex
Pain
• Transmission
– for moderate pain axons release glutamate
– stronger pain: axons release glutamate and substance P
• mice without substance P cannot detect severe injury
24 of 49
Pain
• Associations
– No association with one particular stimulation
– All pain has the potential to cause tissue damage
– Often have emotional reactions
– Pain centers
• No single center in the brain for pain
24 of 49
Pain
• Psychology of Pain
– Environmental factors
• Culture
• Previous experience
– Mental state influence
• Up to 35% of patients with pathological pain get relief from placebos
24 of 49
Pain
• Receptors
– A-delta fibers
• Short, sharper prickling pain
– C fiber endings
• Longer, buring, dull pain
24 of 49
Pain
• Neural pathway
– Fibers enter dorsal horn
– Terminate in laminae I and V of the spinal cord
– Ascend in the anterolateral system
– Fiber release Substance P
• Pain decreases
24 of 49
Pain
• Pain blocking
– Pain information can be blocked or transmitted
• Substantia gelatinosa (spinal cord)
• Laminae II and III (spinal cord)
24 of 49
Pain
• Involved brain areas
– Reticular formation
• Spinoreticular tract
• Arousal
– Limbic system
• Spinomescencephalic tract
• Emotional
– Thalamus
• Posterior nuclear group
– Dull, burning pain
• Ventrobasal complex
– Sharp, prickling pain
– Cortical area
• Cingulate gyrus
24 of 49
Pain
• Gate Control Theory
– Melzak and Wall (1965)
• Proposed that pain perception is controlled by a neural circuit
• Two fibers
– S fibers: small in diameter, increases activity of T-cell and perception of pain
– L fibers: large diameter, decreases activity of the T-cell and perception of pain
24 of 49
Pain
• Gate Control Theory
– Substantia gelantinos
– closes the “gate”
– Send inhibitory messages to T-cell
– Activated by L-fibers (A-fivers) to close gate
– Deactivated by S-fibers (C-fibers) to open gate
24 of 49
Pain
25 of 49
• Opioid mechanisms in brain reduce pain
– endorphins
• neurotransmitters met-enkephalin and leuenkephalin
• bind to opiate receptors
– endorphins are stimulated by pain, especially inescapable pain, sex, long-distance running and thrilling music
Pain
• Opioid mechanisms in brain reduce pain
– supports gate theory of pain that non-pain stimuli can reduce pain
• Endorphins released in the periaqueductal gray area results in blocking release of substance P, reducing pain
25 of 49
Figure 7.15
26 of 49
Figure 7.15 Synapses responsible for pain and its inhibition. The pain afferent neuron releases substance P as its neurotransmitter.
Another neuron releases enkephalin at presynaptic synapses; the enkephalin inhibits the release of substance P and therefore alleviates pain.
Chronic Pain
29 of 49
• Definition
– Situations in which pain persists long after the precipitating injury has healed
• Phantom Limb Pain: amputees
• Causalgia: bullet wounds
• Neuralgia: peripheral nerve infections
Chronic Pain
• Pain management
– Suppression
• Stimulations in two areas results in analgesia
– Periaqueductal gray in midbrain
– Nucleus raphe magnus: in medulla
• Opiates
– Stimulate periaqueductal grapy
– Inhibits a-delta and C-fibers
29 of 49
Chronic Pain
• Pain management
– Medications
• SSRIs in lower doses
• Dual action antidepressants in lower doses
– Elavil
– Acupuncture
• Works through endorphins
• Needles active L-fibers and “close the gate”
29 of 49
Painful Heat
• Body has special heat receptors that respond to burns or high heat above 43 degrees centigrade
– capsaicin stimulates heat receptors and causes neurons to release substance P, increasing pain
– but, capsaicin leaves you temporarily insensitive to pain because neurons are quickly depleted of substance P
27 of 49
Pain and Emotion
• Hurt is an emotion
– we can ignore serious injury at times, e.g., soldier in battle
– placebo, drug with no effect, can relieve pain anesthesia
– also, analgesic is more effective when you know it is being given
28 of 49
Pain and Emotion
29 of 49
• Cingulate cortex reacts to emotional aspect of pain, not the sensation
– painful stimulus to skin results in response
– no response to pin prick when person is told it will not hurt
– expectation of pain leads to response to moderately warm stimulus
– when damaged in rats, they will react to pain on foot but will not learn to avoid the place where it was received
Sensitization, Pain Control and
30 of 49
Itching
• Damaged tissue increases number of sodium gates in nearby receptors to magnify pain
– facilitates activity at capsaisin receptors, increasing pain
– anti-inflammatory drugs, e.g., ibuprofen, decrease pain by reducing the release of chemicals from damaged tissues
• Morphine for pain control
– very effective it reducing serious pain
– post-surgical use recommended
Sensitization, Pain Control and
31 of 49
Itching
• Itch
– caused by release of histamines when skin is irritated
– inhibitory relationship with pain, e.g., when novocaine wears off, you feel itch but face is still numb