7-Bone & Bone Formation
advertisement

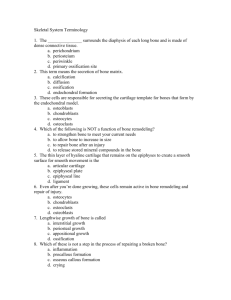
Written by : RAYAN S. ALBALLAA Histology team, Group A Bone & Bone Formation Edited by: Albara Marwa Histology team, Group A Components of Bones : 1. Bone Cells. 2. Calcified Matrix. 3. Periosteum (the outer covering). 4. Endosteum (the inner layer facing the Marrow Cavity). Types of Bone Cells : 1. Osteoprogenitor cells (Forming) 2. Osteoblasts cells (Immature cells) 3. Osteocytes (Mature cells) 4. Osteoclasts Osteoprogenitor Cells Arise from MESENCHYMAL STEM CELL. Differentiate into OSTEOBLASTS. Found in PERIOSTEUM & ENDOSTEUM. Osteoblasts : Derived from OSTEOPROGENITOR cells and can divide. Have CYTOPLASMIC PROCESSES which are extensions of the cytoplasm. Basophilic cells on the surface of the bone (in PERIOSTEUM & ENDOSTEUM). Protein secreting cells. Secrete the ORGANIC PART OF THE BONE MATRIX. Osteocytes : After the osteoblasts secrete the bone matrix, it becomes osteocyte in a small space called the LACUNA. Osteocytes are mature bone cells with flattened nucleus and cytoplasmic processes. Can not divide. Maintain Matrix. The lacunae (the plural of lacuna) are connected together by small canals called CANALICULI. Canaliculi contain the cytoplasmic processes of the osteocytes. GAP JUNCTIONS connect the processes of the osteocytes in the canaliculi. Osteoclasts : Multinucleated, motile, and acidophilic cells in the ENDOSTEUM. Originate by FUSION OF CELLS in the bone marrow. Secrete Enzymes that digest and remove bone matrix forming cavities and canals (to maintain the Ca++ level in blood). Have cytoplasmic processes called RUFFLED BORDER. Bone Matrix : Bone matrix consists of two components: 1. organic components : Type 1 collagen. Chondroitin sulfate. 2. inorganic components : Calcium & phosphorus forming HYDROXYAPATITE CRYSTALS. Bone Matrix : In H&E section, the decalcified bone matrix is acidophilic. It shows the collagen type 1 and the bone cells. The bundles of collagen in the matrix form parallel layers called bone LAMELLAE. Periosteum : It's the outer covering of a bone. It consists of two layers : 1/ outer fibrous layer of dense connective tissue attached to a bone by collagen fibers. 2/ inner cellular layer (Osteogenic layer) of osteoblasts and osteoprogenitor cells. Function : bone formation and repair. Endosteum : it's a layer of cells on the the internal surface of bone facing the marrow cavity. The cells are the osteoprogenitor cells, osteoblasts, and osteoclasts. Function : Bone formation and repair. Types of Bones : Bones exist in two forms : Compact bone : forms the outer part of all bones in the body. Cancellous (spongy) bone: forms the inner part of all bones and is more in the epiphysis (the ends of a long bone) than in the diaphysis (the shaft of a long bone). Compact Bone The matrix of a compact bone consists of REGULAR lamellae (layers) of calcified type 1 collagen. The lamellae form parallel cylinders called OSTEONS or HAVERSION SYSTEMS. Osteons are found deeply in the compact bone. Compact Bone The CONCENTRIC lamellae forming the osteons are called OSTEONAL LAMELLAE. Under the periosteum and endosteum, the lamellae do not form osteons and are called CIRCUMFERENTIAL LAMELLAE. Canals in a Compact Bone HARVERSIAN canal in the centre of each osteon contains osteoblasts, osteoclasts, and blood vessels. VOLKMAN'S canals contain blood vessels and connect the harversion canals of adjacent osteons. CANALICULI connect the lacunae with Haversion canals for nutrition of the osteocytes. Cancellous (Spongy) Bones The lamellae of spongy bone do not form osteons. The lamellae form INTERCONNECTED TRABECULAE. (Small pieces of bone). Cancellous (Spongy) Bones The lamellae in each Trabecula are parallel to each other. The Trabeculae are separated by bone marrow spaces lined by endosteum. In Trabeculae, the canaliculi connect lacunae to bone marrow for nutrition of osteocytes. OSSIFICATION = OSTEOGENESIS = BONE FORMATION Bone Is Formed by Two Methods : 1. INTRAMEMBRANOUS OSSIFICATION. 2. ENDOCHONDRAL OSSIFICATION (INTRACARTILAGENOUS OSSIFICATION). INTERMEMBRANOUS OSSIFICATION : In this type of ossification, bone is formed directly in a membrane of MESENCHYMAL cells without the formation of cartilage. (Ex: Flat bones of the skull) MESENCHYMAL cells differentiate into OSTEOPROGENITOR cells and OSTEOBLASTS which secrete bone matrix and form the PERIOSTEUM. Calcium salts are deposited in the matrix to form bone. OSTEOCLASTS remove part of the bone to form MARROW SPACES (Ex: Frontal bone, Maxilla) ENDOCHONDRAL OSSIFICATION : In this type of ossification, Hyaline Cartilage is formed first and then replaced by bone (Ex: Long bones) Steps of Endochondral Ossification 1. 2. 3. 4. 5. 6. MESENCHYMAL cells first form Hyaline cartilage. Blood vessels enter perichondrium which becomes periosteum and secretes BONE COLLAR on surface of cartilage. Cartilage in centre degenerates leaving Cavities. Blood vessels and Osteoblasts from periosteum enter the cavities to form THE PRIMARY OSSIFICATION CENTRE IN THE DIAPHYSIS. OSTEOBLASTS secrete bone matrix. OSTEOCLASTS in the ossification centre remove part of the new bone to form the bone marrow cavity. Epiphyseal Growth Plate of Cartilage After ossification, a piece of cartilage called EPIPHYSEAL GROWTH PLATE remains between the epiphysis and diaphysis. Ossification of the growth plate continues up to the age of 20 years. The growth plate increases the length of bone because its cartilage continues to grow. Ossification of Epiphyseal Plate Zones of ossification of epiphyseal plate : 1. Zone of cartilage reserve (resting). 2. Zone of proliferation of chondrocytes. 3. Zone of hypertrophy of chondrocytes. 4. Zone of calcification of cartilage. 5. Zone of ossification (formation of bone on the calcified cartilage matrix). 6. Zone of resorption by osteoclasts.