Staphylococcus aureus - York College of Pennsylvania
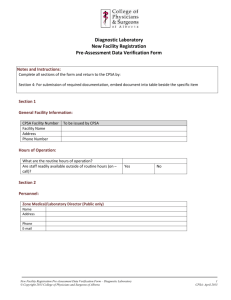
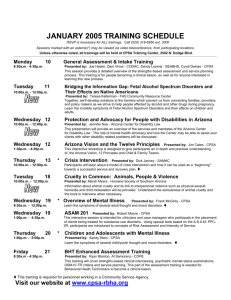
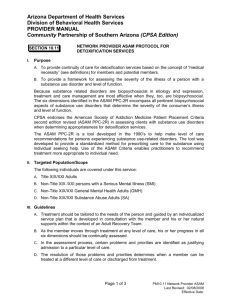
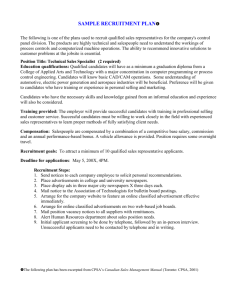
advertisement

Factors influencing Staphylococcus aureus Nasal Carriage Rate and Antibiotic Resistance Prevalence among College Students: 2007-2012 Joshua E. Fabie* & Carolyn F. Mathur Department of Biological Sciences, York College of Pennsylvania 17403 Methods Cultured in Staphylococcus enrichment broth Nasal samples collected Abstract n=57* A Percent Positive 30 16S ribosomal DNA extraction and amplification for sequencing Individual positive colonies grown in slants B C n=105 n=173 25 n=157* n=109 n=41 20 15 % coag % β-lac * n=27 n=23 10 n=55 * n=75 n=71 n=43 5 0 Male Female HC NHC G NG Figure 1. The prevalence of CPSA (2007 to 2012) and β-lactamase positive CPSA (2008-2012) nasal samples are isolated by gender (Male vs. Female); healthcare exposure (HC vs. NHC); and gym participation (G vs. NG). Prevalence was compared with a Fisher’s exact two-tailed test. A) Prevalence of CPSA was greater in males than females (p = 0.0148*), while there was no difference between genders when measuring β-lactamase in the isolates (p = 0.3558). B) When comparing healthcare exposure, there was no difference for CPSA (p = 0.5615), but the prevalence of β-lactamase was higher in the HC samples compared to NHC (p = 0.0051*). C) Differences were not relevant between G and NG samples for the CPSA or β-lactamase tests (p = 0.2376 and p = 0.0743). n= 35 Spring Figure 2. Comparison of the prevalence of CPSA and β-lactamase positive % β-lac CPSA by season. No % Coag difference was determined between spring and fall for CPSA or β-lactamase (p = 0.5009 and p = 0.5650). n= 72 n= 63 Fall n= 142 0 Objectives 5 10 15 20 Percent Positive 50 25 30 n= 55 45 Percent Coagulase Positive • To determine the prevalence of CPSA and β-lactamase in nasal samples collected biannually from college students from 2007 through 2012 • To determine if gender, healthcare exposure, or gym participation relates to prevalence rates of CPSA and β-lactamase in the aforementioned samples • To determine if the prevalence of CPSA and β-lactamase in the above samples varies annually or seasonally (fall vs. spring) β-lactamase testing 35 Introduction • Staphylococcus aureus (SA) is an established facultative anaerobic Gram positive coccal bacterium due to a combination of high carriage rates and its immunoevasive strategies. • Coagulase production is a known virulence factor; the enzyme protease converts fibrinogen to fibrin providing resistance from phagocytosis (Wan et al 2013). • The blaZ gene allows for production of β-lactamase which affords SA resistance to antibiotics containing a β-lactam ring (Pitkälä et al 2007). • A new SA strain, Community-acquired coagulase positive SA (CA-CPSA), is infecting young, healthy individuals, and it is infiltrating hospitals replacing less aggressive nosocomial SA strands (D'Agata et al 2009). • CA-CPSA most often subsists on the soft mucosal membranes of the nose and is capable of spreading rapidly in areas where carriers gather (Munckhof et al 2009). Mannitol salt agar streak plates Results uwsscience.wordpress.com/tag/mrsa/ Potentially pathogenic Staphylococcus aureus (Sa) is important in clinical medicine due to its ability to persist within the human respiratory tract and on the skin under certain conditions. In order to understand more about this interaction, an ongoing study of the nasal carriage rates of Sa and antibiotic resistance prevalence in college students has been underway since 2007. This report is an update covering data from 2007 through 2012. Nasal swabs were cultured in staphylococcus enrichment broth, and further tested for positive, yellow growth on mannitol-salt agar, and for the presence of coagulase (CPSa if positive) and β- lactamase( in CPSa samples only). Overall, 214/881 (24%) of samples taken were coagulase -positive Sa (CPSa), which agrees the prevalence reported in other studies and with our previous reports. Forty-six percent of CPSa carriers were also positive for βlactamase, indicating high levels antibiotic resistance among these individuals. Males had a higher prevalence of CPSa compared to females, (p=0.0148, Fisher exact two-tailed test). CPSa carriers who had regular contact with a health-care environment had higher β-lactamase prevalence compared to non-health care individuals (p = 0.0051). However, the actual CPSa carriage rate did not differ in these 2 groups (p = 0.5614). In addition, no differences were found comparing gym and non-gym users for CPSa (p = 0.2376) and β-lactamase activity (p = 0.0743). No seasonal (spring vs. fall) differences in CPSa prevalence (p=0.5650) or β-lactamase activity (p = 0.5650) were detected. Coagulase testing 40 35 30 n= 103 n= 93 n= 124 n= 57 n= 102 25 n= 80 n= 89 n= 90 n= 37 n= 57 S. aureus 1000x Conclusion • Overall nasal carriage of CPSA was 24.3%, which is slightly less than the carriage rates of 25 to 30% reported by the CDC (2013). Out of the CPSA samples, 45.8% were β-lactamase positive, which is high compared to similar studies (Talan et al 2011). This could be because carriage rates peak in young adult populations and progressively decline with increasing age (Munckhof et al 2009). • The higher prevalence of nasal CPSA for males (31.5%) over females (22.4%) was paralleled in other studies; Munckhof et. al. (2009) found carriage rates of 24.6% for females and 34.8% for males. However, further research is necessary to determine the mechanism for gender differences in carriage in young populations (Kupfer et al. 2010). • The prevalence of CPSA resistant to β-lactam antibiotics was higher in students exposed to health care settings (p = 0.0051). Although there was no difference in the CPSA levels alone, students involved in health care may have a higher risk of exposure to resistant strains of Sa. • Sequencing were not obtained due to ineffective extraction most likely due to complications caused by G+ cell wall. Literature Cited Centers for Disease Control and Prevention. (2013). Definition of MRSA. Retrieved February 12, 2013 from http://www.cdc.gov/mrsa/definition/index.html D'Agata, Erica M. C.; Webb, Glenn F.; Horn, Mary Ann; Moellering Jr., Robert C., & Shigui Ruan. 2009. Modeling the Invasion of Community-Acquired MethicillinResistant Staphylococcus aureus into Hospitals. Clinical Infectious Diseases. 48(3), 274-284. Kupfer, M., Jatzwauk, L., Monecke, S., Möbius, J., & Weusten, A. 2010. MRSA in a large German University Hospital: Male gender is a significant risk factor for MRSA acquisition. GMS Krankenhaushygiene Interdisziplinär, 5(1), 1-8. Munckhof, W. J., Nimmo, G. R., Schooneveldt, J. M ., Schlebusch, S. S., Stephens, A. J., Williams, G. G., & Giffard, P. P. 2009. Nasal carriage of Staphylococcus aureus, including community-associated methicillin-resistant strains, in Queensland adults. Clinical Microbiology & Infection, 15(2), 149-155. Pitkälä, L. Salmikivi, P. Bredbacka, A.-L. Myllyniemi1, & M. T. Koskinen. 2007. Comparison of Tests for Detection of β-Lactamase-Producing Staphylococci. Journal of Clinical Microbiology. 2031-2033. Talan, D. A., Krishnadasan, A., Gorwitz, R. J., Fosheim, G. E., Limbago, B., Albrecht, V., & Moran, G. J. 2011. Comparison of staphylococcus aureus From Skin and Soft-Tissue Infections in US Emergency Department Patients, 2004 and 2008. Clinical Infectious Diseases, 53(2), 144-149. Wan, M., Lauderdale, T., & Chou, C. (2013). Characteristics and virulence factors of livestock associated ST9 methicillin-resistant Staphylococcus aureus with a novel recombinant staphylocoagulase type. Veterinary Microbiology, 162(2-4), 779-784. 20 Acknowledgments 15 10 5 0 Fall 07 Spring 08 Fall 08 Spring 09 Fall 09 Spring 10 Fall 10 Spring 11 Fall 11 Spring 12 Figure 3. Semester trends in prevalence of CPSA nasal samples from 2007 to 2012 Fall 12 I would like to thank C. Taylor, A. Newson, R. Cheng, S. Giordano, M. Branche, C. Cusick, and S. Miller for providing SA data since 2007 that contributes to the depth of my data set.