Community-acquired acute pneumonia: B
advertisement
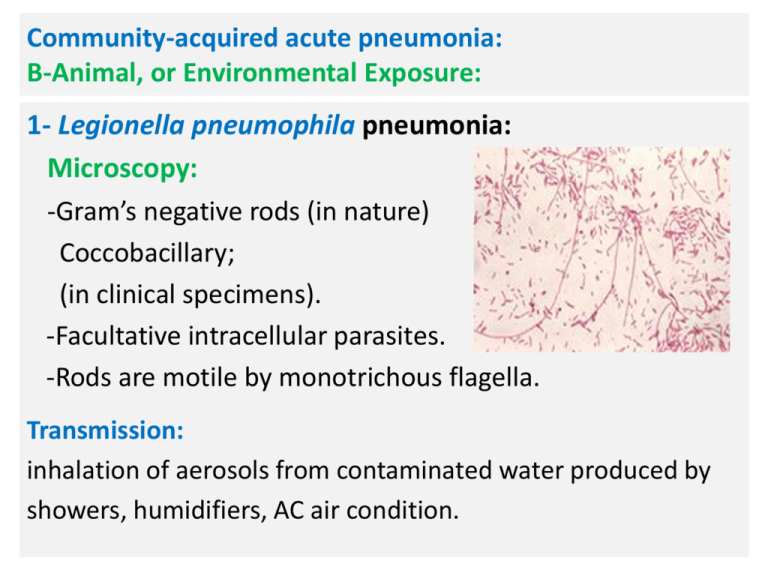
Community-acquired acute pneumonia: B-Animal, or Environmental Exposure: 1- Legionella pneumophila pneumonia: Microscopy: -Gram’s negative rods (in nature) Coccobacillary; (in clinical specimens). -Facultative intracellular parasites. -Rods are motile by monotrichous flagella. Transmission: inhalation of aerosols from contaminated water produced by showers, humidifiers, AC air condition. N Pathogenesis: -Infection of resident alveolar macrophage. -Inhibits phagosome-lysosome fusion. -Formation of phagosome enveloped by endoplasmic reticulum; formation of replicative rod form; Autophage. -TNF-α, and INF-γ Production; monocytic infiltration of air spaces. -Alveolitis (Consolidation) and micro-abscess formation. -Bronchi are not affected. N Laboratory diagnosis: -Staining of specimens by Gram’s stain and Gimesa stain. -Grown on buffered charcoal yeast extract agar. (Enriched media: L-cysteine, iron, α-ketoglutarate). -Rapid identification: 1-Immunofluorescent microscopy 2-PCR. Treatment: 1-Macrolides: Azithromycin 2-Fluoroquinolones: Levofloxacin. N 2-Pneumonic tularemia: (granulomatous infection): : Francisella tularensis infection: Microscopy and Cultural characteristics: -Gram’s negative pleomorphic Coccobacillus with lipidrich capsule. -Facultative intracellular parasite. -Obligate aerobic bacteria. N - Grown on buffered charcoal yeast extract agar. (Enriched media: L-cysteine, iron, α-ketoglutarate). Transmission: 1-Inhalation of infectious aerosols. 2-Blood sucking arthropods bite; vector (ticks, mites) from animals (rabbit, birds). Pathogenesis and clinical presentation: -Infection of alveolar macrophage; granuloma of lung: Pneumonic tularemia. N Pathogenesis and clinical presentation: N -Infection of skin macrophage; ulcerative papule; transmitted to regional lymph nodes; lymphadenitis: Ulceroglandular tularemia ;(the most common presentation). -Hematogenous dissemination to lung from other sites. (infection of APC of liver, spleen, bone marrow). N Treatment of Tularemia: 1- Aminoglycosides: Gentamicin or Streptomycin. 2-Ciprofloxacin and doxycycline. 3-Pneumonic Plague: Yersinia pestis infection: Microscopy, virulence, and cultural characteristics: - Gram’s negative coccobacillus. - In sputum: Gram’s negative bipolar-stained bacilli. -Encapsulated: F1, V, and W antigen; Antiphagocytic Ag. -Lipopolysaccharide (LPS) endotoxin. -Plasminogen activator: degrades fibrin. N Transmission: 1-Person-to-person: inhalation of droplets. 2-Vector-borne: insect bite(Fleas) from rodents (Rat). Pathogenesis and clinical presentation: -Infective dose:100-500 cells. -Incubation: 2-8 days. -Primary: Bubonic plague: Swollen tender regional lymph node; bubo: lymphadenitis (Hemorrhagic necrosis). -Septicemic plague: DIC, Purpura and ecchymoses; Black). -Pneumonic plague: (Bronchopneumonia): A-Primary: Inhalation of droplets. B-Secondary: Hematogenous spread. Transmission of Yersinia pestis (Plague): N N Treatment of Plague: -Pneumonic plague should be treated within 24 hours of appearance of symptoms, (mortality rate: 100%). -Aminoglycosides: Streptomycin, gentamicin. -Fluoroquinolones and doxycycline. 4-Inhalation anthrax: Woolsorter’s disease: Bacillus anthracis infection: -Caused by Gram’s positive aerobic spore-forming bacilli. -Transmission: inhalation of spores. -Not a true pneumonia. -Alveolar macrophage transfer the spore to mediastinal and peribronchial lymph nodes. N Clinical presentation of inhalation anthrax: -Hemorrhagic Mediastinal lymphadenitis. -In 50% of inhalation cases; Anthrax meningitis ; extensive hemorrhage of the leptomeninges; Dark-red “Cardinal’s cap” appearance on autopsy. Treatment: -Only if multiple intravenous antibiotics and passive vaccine administered prophylactically after spore exposure. 2- Hospital-acquired Pneumonia(Nosocomial): Pneumonia acquired during or after hospitalization. It occurs at least 72 hour after admission. Who are at Risk? -Patients on mechanical ventilation ( ICU). -Immunocompromised patients. -Other factors: malnutrition, heart and lung diseases. Causative agents: (Micro-aspiration of Oropharyngeal flora of hospitalized patients): MRSA, Pseudomonas, Enterobacter, Klebsella, Serratia, Acinetobacter (person-to person) and VRE. Chronic and Subacute Pneumonias: Chronic granulomatous pneumonia: 1-Bacterial granulomatous pneumonia: Mycobacterium tuberculosis: -Acid-fast bacilli (Mycolic acid rich waxy capsule). -Non-motile aerobic rods resists drying. -Cultured on Lowenstein-Jensen agar. -Stained by Z.N stain. N Pathogenesis and Clinical presentation: Primary Tuberculosis 90% Latent dormant tuberculosis 10% Progressive active infection Living- bacteria, granuloma Living bacteria &granuloma 25% arrested granuloma Fibrosis or Calcification. Enlarged Tracheobronchial lymph nodes . AIDS, Old, Children 75% Breaks down granuloma Apical lung cavities Tuberculous pneumonia -Caseous material discharged; necrosis -Cavity creation. LymphoHemo Meningitis Osteomyelitis Diagnosis of Tuberculosis: Clinical test:1-Tuberculin skin test. (DTH:48-72 hours). Mantoux test: (PPD: Purified Protein Derivative) Results: Intermediate reaction=5-9mm. Positive reaction=greater than 9mm. 2-Radiology. Laboratory tests: 1-Z.N stain (Low sensitivity). 2-Culture. 3-PCR (highest sensitivity). N 2-Fungal granulomatous pneumonia: (Endemic in America): Transmission: Direct contact with birds and bats. A-Coccidioidomycosis. C-Blastomycosis. B-Histoplasmosis. D-Paracoccidioidomycosis. Coccidioidomycosis: Caused by dimorphic fungi :Coccidioides immitis. Infective stage: Arthrospores generated by septate hyphae. Diagnostic stage: Spherule filled with many endospores. Fungal Pneumonia in AIDS patients: 1-Pneumocystis Pneumonia: (The most common infection). -Caused by Pneumocystis jiroveci (P.carinii). -Yeast lacking ergosterol in cell membrane. -Can not be treated by Amphotericin. -Encysted forms infects alveoli; exudate; blocks gas exchange. -Treatment: Sulfamethoxazole and trimethoprim. Cysts of Pneumocystis carinii ; Sliver stain. N 2-Cryptococcosis: (The second common cause of Fungal pneumonia in AIDS pat.). -Causative agents: Cryptococcus neoformans. -Yeast transmitted to man from birds (pigeon). -Capsulated microbe. -Meningitis in Immunocompromised host. -Treatment: Fluconazole or amphotericin B. The Budding capsulated yeast Cryptococcus neoformans as shown in India ink wet mount .