Toxicology Anion & osmolar gap (Toxic alcohols)
advertisement

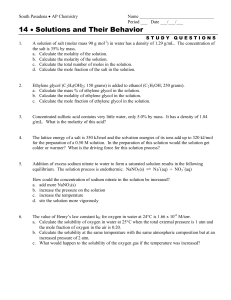
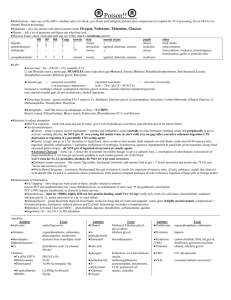
Toxicology Anion Gap, Osmolar Gap & Toxic Alcohols Christine Kennedy Pediatric Emergency Fellow Oct 15, 2009 Objectives 1) 2) 3) Review the causes of an anion gap Review the causes of an osmolar gap Review the “toxic alcohols” Methanol 2) Ethylene Glycol 3) Isopropyl Alcohol 1) 4) Discuss the evidence for Fomepizole Anion Gap AG = Na - (Cl + HCO3). Is it this simple? AG = Measured cations - measured anions Na is the primary measured cation Cl & HCO3 are the primary measured anions What are the other cations & anions?? Normal plasma AG is 7-13 meq/L lab dependant Interpret with caution Anion Gap Anion Gap Anion Gap AG= Unmeasured anions-unmeasured cations An increase in the AG can be induced by: a fall in unmeasured cations a Hypocalcemia, hypomagnesemia, hypokalemia rise in unmeasured anions hyperalbuminemia due to volume contraction the accumulation of an organic anions in metabolic acidosis Anion Gap Primarily determined by the negative charges on the plasma proteins (albumin) As a result, the expected normal values for the AG must be adjusted downward in patients with hypoalbuminemia AG falls by 2.5 meq/L for every 10 g/L reduction in the plasma albumin concentration Anion Gap-The DDx we all learned in medical school Methanol Uremia DKA, SKA, AKA Paraldehyde Isoniazid/Iron Lactate Ethylene glycol Salicylates Anion Gap-DDx Now, this is an okay mnemonic…although Tintinalli isn’t a fan of it If you use it, be aware that… There are other things to include in your Differential It doesn’t really tell you what causes the anion gap What causes the AG? Methanol ----> formate Uremia--->Chronic renal failure (GFR<20=impaired excretion of acids) DKA, SKA, AKA---> Acetaldehyde acetylCoA B-hydroxybutyrate, acetoacetate P Isoniazide--->lactic acidosis 2o to seizure activity Iron---> lactic acidosis (uncoupling of oxidative phosphorylation) Lactate Ethylene glycol ----> glyoxylate, glycolate, oxalate Salicylates ----> ketones, lactate Anion Gap Other causes of AG (due to lactate) Metformin Phenformin Propylene Glycol Carbon Monoxide Hydrogen sulfide Cyanide Methemoglobinemia Anion Gap-DDx Methanol/Metformin/Methemoglobinemia Uremia DKA, SKA, AKA Paraldehyde/Phenformin/Propylene glycol Isoniazid/Iron Lactate…… Ethylene glycol Salicylates Osmolar Gap Osmolar gap Measured serum osmolality-calculated osmolarity should be <10 mmol/L Plasma osmolarity Determined by the concentration of the different solutes in the plasma Posm = 2[Na] + [Glc] + [BUN] + 1.25[ethanol] Na multiplied by 2 to account for accompanying anions Osmolar Gap…which method to use??? Osmolarity Formulas Calgary 1.86Na + BUN + glucose + 9 Why 1.86? 93% is in Na+ & Cl- (ionized forms) and 7% is in the nonionized forms (NaCl) Why +9? Intercept for multiple regression line NB: EtOH is not automatically added! Edmonton 2Na + BUN + glc Serum is only 93% water: 1.86/0.93 = 2 DDx of elevated Osm Gap With anion gap metabolic acidosis Methanol ingestion End-stage renal disease (GFR <10)* Diabetic ketoacidosis** Alcoholic ketoacidosis** Paraldehyde ingestion Lactic acidosis** Ethylene glycol ingestion Formaldehyde ingestion DDx of elevated Osm Gap Without metabolic acidosis Ethylene glycol and Methanol* EtOH** Isopropanol ingestion---> acetone Diethyl ether ingestion Mannitol Severe hyperproteinemia Severe hyperlipidemia Ethanol and the Osmolar Gap Case 1 Intoxicated male Na 140, BUN 5, Glc 5, EtOH 75 Osmolality 385 Osmolarity = ____ Osm gap = ____ Ethanol and the Osmolar Gap Case 1 Intoxicated male Na 140, BUN 5, Glc 5, EtOH 75 Osmolality 385 Osmolarity 2(140) + 5 + 5 + 75 = 365 Osm gap = 20 So how does EtOH affect the osm gap? Ethanol and the Osmolar Gap Several Studies have noted the increase in osmolar gap with rising EtOH in a non 1:1 relationship Many different EtOH conversion factors have been developed Britten 1972: 1.74 Glasser 1973: 1.1 Pappas 1985: 1.12 Geller 1986: 1.20 Galvan 1992: 1.14 Synder 1992: 1.20 Hoffman 1993: 1.09 Ethanol and the Osmolar Gap Purssell. Ann Emerg Med 2001; 38: 653659. Derived a formula to account for the relationship between ethanol and then osmolar gap Prospectively validated Best formula = EtOH (mmol/L) X 1.25 Explanation for EtoH X 1.25 Ethanol has a “non-ideal” osmotic behaviour because molecules form physiochemical bonds with other molecules Results in an effect on osmolarity that is non-uniform Data from Calgary lab O-Gap (absence of toxic Alc) This supports the 1.25 EtOH conversion 200 180 O-GAP, mosmoL 160 140 120 100 80 60 40 20 0 0 50 100 Ethanol m m ol/L 150 200 Case 1 Intoxicated male Using 1:1 EtOH Osmolality = 385 Osmolarity = 2(140) + 5 + 5 + 75 = 365 Osm gap = 20 Redo this with EtOH X 1.25 = 94 Osmolarity = 2(140) + 5 + 5 + 94 = 384 Osm gap = 1 Case 2 35 year male Took a swig of a mug that had antifreeze Na 140, Cl 106, BUN 5, Glc 5, EtOH 25, HCO3 24 Osmolality 321 Normal anion gap (10) Osmolarity = ___ Osmolar gap = ___ Case 2 Osmolarity=2(140) + 5 + 5 + 1.25(25)=321 Osmolar gap = 321 – 321 = 0 What is the normal osmolar gap? Normal Osmolar gap Hard to define because it depends on Lab method of osmolality determination Osmolarity formula used Lab error of Na, BUN, Glc, EtOH EtOH conversion factor used Few studies documenting what normal osmolar gaps are in the population Normal Osmolar gap Traditionally normal osmolar gap is <10 In case #2 the osm gap was 0 Can osmolar gaps be used to rule out toxic alcohol ingestions? Is there a cut off where toxic alcohols should be routinely measured? Normal Osmolar Gap Hoffman. J Toxicol Clin Toxicol. 1993 Mean Osm gap= -2 SD 6.1 -14 -8 -2 +4 +10 Can you still miss toxic levels? -14 0 Baseline -14 Osm gap 0 Methanol level 14!!! When should toxic alcohols be measured? AMA guidelines Calgary Osm gap >10: measure methanol and ethylene glycol Edmonton Osm gap >2: measure ethylene glycol Osm gap >5: measure methanol When should toxic alcohols be measured? AMA guidelines Where do the 5 & 2 come from? “Classically” EG & methanol ingestions needed treatment at levels of 20 mg/dL in nonacidotic patients This translates to EG level of 3.2 mmol/L Methanol level of 6.24mmol/L Analyzed all published case reports of MeOH poisoning to determine the applicability of the 20mg/dL (6.24mmol/L) threshold for treatment 329 articles analyzed (2433 patients) 70 articles met inclusion criteria (173 pts) Only 22 pts presented for care within 6 hours of ingestion All but 1 patient was treated with an ADH inhibitor A clear acidosis developed only with a methanol level of >126mg/dL (39.4mmol/L) There were cases of acidosis after only a few hours of ingestion Conclusions There are no useful data available to create treatment recommendations for the MeOH exposed pt who presents early, prior to development of toxicity This is a time-dependent disease (which is not accounted for in the “classic” treatment recommendations) So….what is the utility of osm gap? Osmolar gaps are not 100% reliable to exclude treatable toxic alcohol ingestions Low suspicion-----check osmolar gap High suspicion----check toxic alcohol levels regardless of osmolar gap Toxic Alcohols “Toxic” Generally reserved for any alcohol other than ethanol A few mouthfuls can kill: Average adult mouthful: 0.42cc/kg Lethal dose of methanol: 1.2cc/kg Lethal dose of ethylene glycol: 1.4-1.6cc/kg How does EtOH affect methanol & ethylene glycol metabolism EtOH competes for the enzyme alcohol dehydrogenase Minimizes the metabolism of methanol and ethylene glycol to their toxic metabolites Takes longer to form an AG in methanol or ethylene glycol ingestion if there is concurrent EtOH ingestion Case 3 21 year male presents at 7 am Drank 1 glass of antifreeze at 3 am, “was tired of life” Had been drinking EtOH earlier in the night Vomited immediately after ingestion Now he wants to live so came to ED O/E T 37.2, HR 129, RR 18, BP 138/96 Neuro: inebriated CVS, resp, abdo all unremarkable Case 3 What investigations would you like? Labs Na 141, K 3.6, Cl 107, CO2 21 BUN 10, Cr 190, glc 6, pH 7.35 Osmolality 329 EtOH 8.3 mmol/L Ethylene Glycol, methanol, isopropanolpending Is there a benefit of testing the urine? Case 3 What would you like to do for this patient? Case 3 Ethylene Glycol-7 mmol/L Methanol-undetectable Isopropyl Alcohol-undetectable Does this change your treatment plan? How about if the EG level was 9mmol/L? Case 4 17 male and his 13 year old girlfriend present to ACH ED at 3am Male is obviously intoxicated, slurring his words and swearing at the triage nurse Presenting complaint…. “my girlfriend can’t see” Couple came from a party Heavy drinking and marijuana consumption at the party Case 4 Girl Very sedated, vomited at triage Vitals: T37.8, HR 112, BP 115/70, RR 28 O/E: Eye exam: mydriasis, but uncooperative CVS normal, resp normal, abdo tender diffusely Labs??? Case 4 Labs on girl Glc 5 Na 142, K 4.0, Cl 105, CO2 15 CBG 7.25/30/55/15/-10 lactate 4 BUN 8, Cr 55 Osmolality 320 EtOH 19mmol/L Case 4 Guy Obnoxious, ongoing slurring and swearing Vitals: T37.9, HR 110, RR 18, BP 120/80 O/E Diaphoretic H&N normal CVS, Resp, GI normal Labs??? Case 4 Labs Glc 4.5 Na 138, K 4.0, Cl 105, CO2 21 CBG 7.35/35/55/21/-4 lactate 2 BUN 7, Cr 70 Osmolality 395 EtOH 85mmol/L U/A: +ketones Case 4 What’s the girl’s diagnosis? What do you want to do for her? What’s the guy’s diagnosis? What do you want to do for him? Case 4 Further history….girl showed up at the party at 7pm, clearly intoxicated Rumours that prior to the party she had experimented with windshield wiper fluid in order to “get drunk fast”, as did another girl At the party, she consumed 5 beer At 2 am she started to complain of blurred vision Methanol level 16mmol/L Case 4 Does this change what you want to do for her? Ethylene Glycol Coolant Peak levels in 1-4 hours Toxicity is a result of the metabolites Glycolic acid---->glyoxylic, oxalic acid Oxalic acid produces calcium oxalate crystalluria** Ethylene Glycol Metabolism Metabolic acidosis Ethylene Glycol Urine sediment under polarized light showing calcium oxalate monohydrate crystals Ethylene Glycol Calcium oxalate monohydrate and envelope-shaped calcium oxalate dihydrate crystals Stages of EG toxicity Phase 1 (1-12 hours post ingestion) Phase 2 (12-24 hours post ingestion) Cardiopulmonary phase (tachycardia, tachypnea, mild hypertension, CHF, ARDS, cardiomegaly, circulatory collapse) Phase 3 (24-72 hours post ingestion) CNS depression (inebriation, hallucinations, coma, seizures) Nephrotoxicity (CVA tenderness, oliguria, ATN) Phase 4 (6-12 days) Delayed CNS (Cranial neuropathies, motor deficits, cognitive deficits) Methanol Paint removers, solvents, varnishes, windshield washing fluid Well absorbed from the GI tract Peak levels 30-90 minutes after ingestion Presentation may be delayed 12-18 hours (longer if EtOH co-ingested) Toxicity is the result of the metabolites Formaldehyde & formate Cause optic papillitis and retinal edema---> blindness Inhibits mitochondrial respiration---> lactic acidosis Methanol Metabolism Methanol Metabolism Retinal & optic nerve damage Methanol Clinical presentation CNS depression Seizures Visual disturbances Abdominal pain Nausea Vomiting AG metabolic acidosis Osmolar gap EG & Methanol Tx Approach ADH blockage (Ethanol or Fomepizole) Alkalinize (If acidotic) Accelerate Elimination (Dialysis) Adjuncts Supportive treatment Seizures IV Calcium for symptomatic hypocalcemia GI decontamination EG/Methanol are very rapidly absorbed Activated charcoal does not absorb significant amounts of alcohol---no role Gastric aspiration via NG tube may be beneficial only within the first hour after ingestion, prior to symptoms ADH Inhibition Prevents conversion of parent alcohol to it’s toxic metabolites ADH inhibition doesn’t help once the toxic metabolites are formed 2 options EtOH 65X more affinity for ADH than EG 10-20X more affinity for ADH than methanol Fomepizole 500-1000 X more affinity for ADH than EtOH ADH Inhibition MOA N Engl J Med 1999;340:832-8 ADH Inhibition AACT practice guidelines Toxic alcohol concentration >3.2mmol/L (EG), >6.2mmol/L (methanol) OR Documented recent history of ingesting toxic amounts of EG/methanol with osm gap >10 OR Strong clinical suspicion of EG/methanol poisoning with at least 2 of: Arterial pH <7.3 Bicarb <20 mEq/L Osm gap >10 Urinary oxalate crystals EtOH Load Maintenance 7.6-10ml/kg of 10% solution IV in D5W over 30 min Average drinker: 1.39 mL/kg/h Chronic drinker: 1.95 mL/kg/h Non drinker: 0.83 mL/kg/h With dialysis: 3 mL/kg/h Monitor levels q1h Goal: 22-28 mmol/L EtOH level Continue until EG/methanol levels are undetectable T1/2 is increased with ethanol EG 11-18h, Methanol 30-52 h EtOH Complications of infusion Hypotension Respiratory depression (with supratherapeutic concentrations) Flushing Hypoglycemia Hyponatremia Pancreatitis Gastritis Inebriation Patients receiving IV ethanol require ICU monitoring Orally administered ethanol is effective, and may be considered when ICU is unavailable rural areas where there may be a significant delay in getting the patient to another hospital Fomepizole (4-methylpyrazole) Load Maintenance 10mg/kg IV q12h X 4 doses Then 15mg/kg q12h until EG/methanol levels <3.2mmol/L Don’t need to monitor levels & no ICU monitoring Expensive (~$1000 per 1.5g vial) 15mg/kg IV in 250 cc NS or D5W over 30 min Average 4 vials per patient Previous EtOH intake does not decrease efficacy T1/2 is increased EG 20h; methanol 54h Fomepizole-How good is it? Anecdotal case 42 year old male drank 1.5 L of antifreeze and presented 4.5 hours after ingestion. EG level 51mmol/L Loading dose of EtOH, then fomepizole Complete recovery without dialysis CJEM 2002 Fomepizole-How good is it? Retrospective case series Fomepizole in the treatment of uncomplicated EG poisoning. Lancet 1999. Treatment of acute methanol poisoning with fomepizole. Intensive Care Med 2001. Fomepizole-How good is it? Multi-center prospective clinical trials Fomepizole for the treatment of ethylene glycol poisoning. Methylpyrazole for Toxic Alcohols Study Group. N Engl J Med. 1999 Fomepizole for the treatment of methanol poisoning. N Engl J Med. 2001 Fomepizole for the treatment of ethylene glycol poisoning. N Engl J Med. 1999 Enrolled 23 patients (19 met criteria for EG poisoning) 18 patients survived 1 death occurred in a pt with severe acidemia clinical course complicated by an MI Died of cardiogenic shock on the day of admission Fomepizole for the treatment of ethylene glycol poisoning. N Engl J Med. 1999 All 10 pts who had normal renal fcn at presentation showed no subsequent kidney injury EG levels as high as 71.9mmol/L pH levels as low as 7.16 Glycolic acid levels under 10.5mmol/L Pts needed median of 3.5 doses [range 1-7] Fomepizole for the treatment of methanol poisoning. N Engl J Med. 2001 11 patients 2 died Both pts comatose with signs of anoxic brain injury on admission pH 6.9 & 7.01 Formic acid levels 43 & 28 mmol/L Fomepizole for the treatment of methanol poisoning. N Engl J Med. 2001 9 survived pH’s as low as 6.9 Methanol levels as high as 191 mmol/L Visual deficits (only able to count fingers) Formic acid levels no higher than 21.7mmol/L All regained baseline visual acuity Pts needed median of 4 doses [range 1-10] When does Fomepizole win? Rural areas without adequate lab support Patients prone to hypoglycemia Liver failure Children Patients who are going to be admitted to the ward and dialysis is not imminent (i.e. those without acidosis or end-organ damage) Fomepizole-Adverse Effects? Adverse Drug Events Associated with the Antidotes for Methanol and EG poisoning: A Comparison of Ethanol and Fomepizole Cohort study of pts 13 years and older Hospitalized patients 1996-2005 Methanol or EG poisoning treated with fomepizole or ethanol Primary outcome At least one adverse drug event Adverse drug event rate per person-day of antidote tx Secondary outcomes Severe & serious adverse drug events Lepik et al. Annals of Emergency Medicine 2009; 53(4): 439-50 Adverse Drug Events Associated with the Antidotes for Methanol and EG poisoning: A Comparison of Ethanol and Fomepizole 223 charts reviewed, 172 analyzed Toxicologists identified at least 1 AE in 74/130 (57%) EtOH treated pts 5/42 (12%) Fomepizole treated pts CNS symptoms accounted for most AE 48% of all patients treated with EtOH 2% of all patients treated with Fomepizole Lepik et al. Annals of Emergency Medicine 2009; 53(4): 439-50 Adverse Drug Events Associated with the Antidotes for Methanol and EG poisoning: A Comparison of Ethanol and Fomepizole Severe AE (Poison Severity Score severity threshold) 26/130 (20%) of EtOH treated pts 2/42 (5%) of Fomepizole treated pts Coma, extreme agitation, cardiovascular Coma, cardiovascular Serious AE (WHO criteria) 11/130 (8%) EtOH treated pts Resp depression, hypotension 1/42 (2%) Fomepizole treated pts Hypotension, bradycardia Lepik et al. Annals of Emergency Medicine 2009; 53(4): 439-50 Adverse Drug Events Associated with the Antidotes for Methanol and EG poisoning: A Comparison of Ethanol and Fomepizole Median adverse drug event onset was within 3 hours of the start of the antidote Adverse drug event rates adverse drug events per treatment-day 0.93 EtOH 0.13 Fomepizole Lepik et al. Annals of Emergency Medicine 2009; 53(4): 439-50 Fomepizole-Any contraindications? Previous allergic reaction None reported Fomepizole-When to stop Previous guidelines* EG<3.2mmol/L Methanol < 6.2mmol/L NEJM 2009** Exact point not defined States “undoubtedly safe to discontinue therapy when the EG level is <4.8mmol/L & methanol <9.4mmol/L Great review article Fomepizole for EG and Methanol Poisoning. N Engl J Med 2009; 360:221623. NaHCO3 Rationale EG metabolized to glycolate, glyoxalate & oxalate Methanol metabolized to formate Acidemia leads to protonation of these metabolites & makes them more likely to penetrate end-organ tissues Bicarb deprotonates them, making them less toxic Issues No clear evidence for how bicarb should be given NaHCO3 Recommendations UTD: 1-2 mEq/kg bolus for pH < 7.3, then infusion (133meq NaHCO3 in 1L D5W) to maintain pH >7.35 American Academy of Clinical Toxicology Practice Guidelines on the treatment of Ethylene Glycol Poisoning. J Toxicol Clin Toxicol 1999 American Academy of Clinical Toxicology Practice Guidelines on the treatment of Methanol Poisoning. J Toxicol Clin Toxicol 2002 Adjuncts Thiamine & Pyridoxine MOA: involved in the metabolism of glyoxylic acid to non-toxic substrates Theoretical benefit with some indirect evidence Cheap! So use them! Dose: Thiamine 100mg IV Pyridoxine 100 mg IV Adjuncts Folinic acid 50mg Folic acid 50mg IV IV q6h for methanol How about for EG? Perhaps a better question is….Does ethylene glycol metabolism produce formate? Which pathway is correct??? Ethylene Glycol--->Formate EVIDENCE AGAINST: NONE OF THE FOLLOWING MENTION FORMATE AS A POSSIBLE METABOLITE FROM ETHYLENE GLYCOL…. 1. Medical Toxicology. 3rd edition. R. Dart. 2. Clinical Toxicology. Ford, Ling, Delaney, Erickson. 3. Goldfrank’s Toxicologic Emergencies. 5th Edition. Ethylene Glycol--->Formate EVIDENCE FOR formate formation from the metabolism of ethylene glycol… Critical Care Toxicology: Diagnosis and Management of the Critically Poisoned Patient. Brent, Wallace, Burkhart, Phillips, Donovan. 2. Haddad and Winchester’s Clinical Management of Poisoning and Drug Overdoses. Shannon, Berron, Burns. 3. Emergency Toxicology 2nd Edition. Peter Viccellio. 4. Current Occupational and Environmental Medicine. Joseph La Dou. 5. Poison Management Manual. 4th Edition. D. Kent. G. Willis. K Lepik. 6. 6. W. Henderson and J. Brubacher. Methanol and Ethylene Glycol Poisoning: A case study and review of the current literature. CJEM. Vol 4. (2002) 1. Ethylene Glycol--->Formate Total of 9 resources 3 do not mention formate 6 mention formation of formate Of the 6, only 1 (#3) suggested treatment with folic acid. Yet the reference quoted suggested “other metabolites (including formate) are deemed to be negligible.” Hemodialysis Best method to rapidly remove parent alcohols and their toxic metabolites General recommendations Severe or refractory metabolic acidosis Deteriorating vital signs Onset of acute renal failure/visual symptoms EG >8.1mmol/L; Methanol > 15.6mmol/L* evidence for HD based on levels alone is almost nonexistent Hemodialysis Intensive Care Med (2005) 31: 189-195 Hemodialysis Intensive Care Med (2005) 31: 189-195 Hemodialysis Intensive Care Med (2005) 31: 189-195 Hemodialysis Special considerations Fomepizole is dialyzable European recommendation: continuous infusion 1mg/kg/h USA manufacturer recommends q4h administration Endpoints Serum pH normal Parent alcohol concentration <3.2mmol/L Resolution of the osmolar gap Back to the cases…. Case 3 21 year male drank antifreeze (&EtOH) AG 13, osm gap 21, pH 7.35, EtOH 8.3mmol/L, 190, Na 141, K 3.6, Cl 107, CO2 21 Ethylene Glycol: 7 mmol/L Methanol and Isopropanol-undetectable How would you treat him? Fomipazole or Ethanol NaHCO3 not needed at this time Dialysis not needed Adjuncts: Thiamine and Pyridoxine Cr Back to the cases…. Case 4 (girl) Very sedated, “can’t see”, T37.8, HR 112, BP 115/70, RR 28 CBG 7.25/30/55/15/-10, Na 142, K 4.0, Cl 105, CO2 15 EtOH 19mmol/L, methanol 16mmol/L, BUN 8, Cr 55 AG 22, Osm gap 1 Treatment? ADH blockage-will it help her given that she has AG already and no osm gap? Dialysis indications: Vision changes, MeOH>15mmol/L NaHCO3 Adjuncts: Folate Doesn’t the ethanol consumption protect her? Back to the cases…. Case 4 (guy) Inebriated, EtOH 85mmol/L CBG 7.35/35/55/21/-4 AG 12, Osm gap 2 U/A: +ketones Treatment??? No toxic alcohol exposure Treat as you would a drunk teenager Proposed Treatment Algorithm Intensive Care Med (2005) 31:189–195 Isopropyl Alcohol Disinfectant, solvent Typically comprises 70% “rubbing alcohol” When ingested, functions as a CNS depressant and inebriant Fatality is rare Does NOT cause an elevated anion gap acidosis retinal toxicity (as does methanol) renal failure (as does ethylene glycol) Isopropyl Alcohol Acetone Mild CNS depressant Responsible for marked ketosis Isopropyl Alcohol Lethal dose 250 mL of 70% solution Rapidly absorbed, peaks at 1-2 hours T1/2 = 2.5-8 hours (much slower when ADH inhibitors are present) Absorption and toxicity are possible following dermal exposure (in infants) Isopropyl Alcohol Clinical (Symptoms peak at 1 hour) Inebriation w/ disinhibition--->sedation---> stupor--->coma Nausea, vomiting, abdominal pain Fruity breath (acetone) The metabolite (acetone) causes much less sedation therefore expect clinical improvement with time Laboratory Serum isopropyl alcohol levels & acetone Elevated osmolar gap Urine & serum ketones Lytes, BUN, Cr, blood gas Treatment Supportive (ABC’s) Consider intubation if patient unable to protect airway Decontamination: no real role ADH inhibition: no indication Review of Objectives 1) 2) 3) Review the causes of an anion gap Review the causes of an osmolar gap Review the “toxic alcohols” Methanol 2) Ethylene Glycol 3) Isopropyl Alcohol 1) 4) Discuss the evidence for fomepizole Summary-Anion Gap AG = Na - (Cl + HCO3) Simple way to calculate AG=unmeasured anions-unmeasured cations When considering the DDx, can use MUDPILES, but need to consider what actually causes the AG In hypoalbuminemic patients, need to re-adjust the “accepted” AG Summary-Osmolar gap Posm = 2[Na] + [Glc] + [BUN] + 1.25[ethanol] Osmolar gap can not distinguish among ethanol, isopropyl alcohol, methanol or ethanol Osm gap increases only in the presence of the parent alcohols Osm gap is not sensitive enough to rule out small ingestions An unexlpained large osm gap (>25) is presumptive of a recent methanol, ethylene glycol or isopropyl alcohol exposure Summary-EG & Methanol Rapidly absorbed and toxic in small amounts A low/neg EG/methanol level and osm gap can be misleading in late presenters Expect normal AG in early presenters Significant met acidosis suggest toxic metabolites---only definitive treatment is dialysis ADH inhibitors are use to prevent further metabolization of the parent alcohol Fomepizole seems to be the recommendation! Summary-Isopropyl Alcohol Hallmark of isopropyl alcohol metabolism is marked ketonemia and ketonuria in the absence of metabolic acidosis Isopropyl alcohol is rapidly and completely absorbed following oral ingestion Clinical presentation similar to ethanol intoxication If ingested in isolation, no tx needed, but need to r/o ingestion of more toxic alcohol