Prototype drug - Nursing Pharmacology
advertisement

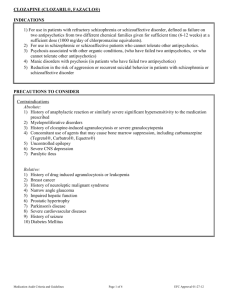
OVERVIEW: Neuro System Tri-Cyclic Antidepressant Antidepressant / Anxiolytic MAOIs lorazepam (Ativan) diazepam (Valium) Benzodiazepines GABAA zolpidem (Ambien) Antagonist Phenytoin-Like Drugs phenytoin (Dilantin) valproic acid (Depakote) Succinimides ethosuximide (Zarontin) Barbiturates phenobarbital (Luminal) Phenothiazines Non-Phenothiazines Opioids Salicylates NSAIDs Non-Opioid morphine (Infumorph) Atypical Antipsychotics aspirin (ASA) ibuprofen (Motrin) acetaminophen (Tylenol) Central Acting tramadol (Ultram) Anti-Migraine ergotamine (Cafergot) Sumatriptan (Imitrex) escitalopram (Lexapro) Opioid Antagonists naloxone (Narcan) chlorpromazine (Thorazine) halperidol (Haldol) risperidone (Risperdal) Psychoses • Severe mental and behavioral disorders characterized by: • Delusions • Hallucinations • Illusions • Paranoia Acute episode – occur over hours or days • Chronic episode – develop over months or years Factors Attributed to Development of Psychoses • Genetic • Neurological • Environmental Schizophrenia • • • • • • • • Abnormal thoughts and thought processes Disordered communication Withdrawal from other people and outside environment Severe depression High risk for suicide Most common psychotic disorder Manifests in men aged 15 to 24 years Manifests in women in aged 25 to 34 years Symptoms of Schizophrenia • Variety of symptoms that may change over time • • • • • • Hallucinations, delusions, or paranoia Strange and irrational behavior, actions Rapid alteration between extreme hyperactivity and stupor Attitude of indifference; detachment Deterioration of hygiene, job, academic performance Withdrawal from social and interpersonal relationships • Characterized by positive and negative symptoms • Positive: add on to normal behavior • Negative: subtract from normal behavior • Diagnosis of positive and negative symptoms important for selection of appropriate drug Causes of Schizophrenia • Cause yet to be determined • Genetic • Neurotransmitter imbalance • Symptoms seem to be associated with dopamine type 2 receptor in brain • Antipsychotic drugs enter dopaminergic synapses and compete with dopamine Conditions That May Mimic the Behaviors of Schizophrenia • • • • Drug use Brain neoplasm Infections Hemorrhage Selection of Antipsycotics • No single drug of choice • Selection of drug type depends on • Clinician experience • Side effects • Patient needs Categories of Antipsychotic Drugs • Conventional antipsychotic • Phenothiazines and phenothiazine-like drugs • Atypical antipsychotic • Nonphenothiazines Patient Drug Compliance • Goal is to reduce psychotic symptoms so patients have ability to self-care • Drugs do not cure mental illness • Patients must continue drug regimen to remain in remission • Relapse rate for those who discontinue medication is 60% to 80% Role of the Nurse • • • • • Monitor client’s condition Give client drug education Obtain health history (long-term physical problems) Obtain drug history (use of illegal drugs, alcohol, etc.) Obtain baseline assessment (liver and kidney function, vision, mental status) • Monitor for extrapyramidal symptoms, and report to the physician immediately Conventional (Typical) Antipsychotics • • • • • Monitor for decrease of psychotic symptoms, side effects Monitor for anticholinergic side effects Monitor for alcohol, illegal-drug, caffeine, and nicotine use Monitor for cardiovascular changes Monitor for seizures and patient’s environment Conventional (Typical) Antipsychotics (continued) • • • • • Monitor for decrease of psychotic symptoms, side effects Monitor for anticholinergic side effects Monitor for alcohol, illegal-drug, caffeine, and nicotine use Monitor for cardiovascular changes Monitor for seizures and patient’s environment Atypical Antipsychotic • • • • • Monitor RBC and WBC and hematologic side effects Observe for side effects and anticholinergic side effects Monitor for decrease of psychotic symptoms Monitor for alcohol, illegal-drug use, caffeine, nicotine use Monitor elderly closely Extrapyramidal Symptoms (EPS) • Tremor, muscle rigidity, stooped posture (pseudoparkinsonism) • Muscle spasms of face, tongue, neck or back (acute dystonias) • Inability to rest and relax; pacing (akathisia) • Lip smacking; wormlike movements of the tongue; uncontrolled chewing and grimacing (tardive dyskinesias) Neuroleptic Malignant Syndrome (NMS) • Client suffers a toxic reaction to therapeutic doses of antipsychotic drug • Client exhibits • • • • • • Elevated temperature Unstable blood pressure Profuse sweating Dyspnea Muscle rigidity Incontinence Phenothiazines • Prototype drug: chlorpromazine HCI (Thorazine) • Mechanism of action: blocks positive symptoms of schizophrenia • Primary use: for severe mental illness • Adverse effects: acute dystonia, akathisia, Parkinsonism, tardive dyskinesia, anticholinergic effects, sedation, hypotension, sexual dysfunction, and neuroleptic malignant syndrome Prototype Drug: Chlorpromazine hydrochloride Nonphenothiazines haloperidol (Haldol) Mechanism of action: blocking of the dopamine type 2 receptor Primary use: severe mental illness Adverse effects: identical to that of phenothiazines • Prototype drug: • • • Prototype Drug: Haloperidol Atypical Antipsychotics risperidone (Risperdal) Mechanism of action: block dopamine type 2 receptors, serotonin and alpha-adrenergic receptors Primary use: severe mental illness; treats both positive and negative symptoms Adverse effects: fewer than those of phenothiazines and nonphenothiazines, but obesity and its risk factors need to be monitored • Prototype drug: • • • Atypical Antipsychotics (continued) • Dopamine System Stabilizers • Newest antipsychotic class • Aripiprazole (Abilify) controls both positive and negative symptoms • Serious side effects compared to other antipsychotic drugs is low Prototype Drug: Risperidone Conventional (Typical) Antipsychotic Agents • Phenothiazines • Action blocks positive symptoms • Mellaril, Compazine, Permitil • Nonphenothiazines • Action same as that of phenothiazines • Taractan, Loxitane, Navane Atypical Antipsychotics • Treats both the positive and negative symptoms • Less dramatic side effects, but still significant • Examples: Seroquel, Risperdal, Zyprexa Nursing Process Focus: Patients Receiving Atypical Antipsychotic Therapy NCLEX-RN Review Question 1 The patient states that he has not taken his antipsychotic drug for the past 2 weeks because it was causing sexual dysfunction. The name antipsychotic explains that continuing the medication as prescribed is important because: 1. 2. 3. 4. Hypertensive crisis may occur with abrupt withdrawal. Muscle twitching may occur. Parkinson-like symptoms will occur. Symptoms of psychosis are likely to return. NCLEX-RN Review Question 1 – Answer 1. 2. 3. 4. Hypertensive crisis may occur with abrupt withdrawal. Muscle twitching may occur. Parkinson-like symptoms will occur. Symptoms of psychosis are likely to return. NCLEX-RN Review Question 1 – Rationale Rationale: Symptoms of psychosis are likely to return and manifest as agitation, distrust, and frustration. NCLEX-RN Review Question 2 Prior to discharge, the nurse provides teaching related to side effects of phenothiazines to the patient, family, or caregiver. Which of the following should be included? 1. 2. 3. 4. The patient may experience withdrawal and slowed activity. Severe muscle spasms may occur early in therapy. Tardive dyskinesia is likely early in therapy. Medications should be taken as prescribed to prevent side effects. NCLEX-RN Review Question 2 – Answer 1. 2. 3. 4. The patient may experience withdrawal and slowed activity. Severe muscle spasms may occur early in therapy. Tardive dyskinesia is likely early in therapy. Medications should be taken as prescribed to prevent side effects. NCLEX-RN Review Question 2 – Rationale Rationale: Acute dystonias occur early in the course of therapy. These are severe muscle spasms, particularly of the back, neck, tongue, and face. NCLEX-RN Review Question 3 A 20-year-old man is admitted to the in-patient psychiatric unit for treatment of acute schizophrenia and is started on risperidone (Risperdal). Therapeutic outcomes of this drug will include: 1. 2. 3. 4. Restful sleep, elevated mood, and coping abilities Decreased delusional thinking and lessened auditory/visual hallucinations Orthostatic hypotension, reflex tachycardia, and sedation Relief of anxiety and improved sleep and dietary habits NCLEX-RN Review Question 3 – Answer 1. 2. 3. 4. Restful sleep, elevated mood, and coping abilities Decreased delusional thinking and lessened auditory/visual hallucinations Orthostatic hypotension, reflex tachycardia, and sedation Relief of anxiety and improved sleep and dietary habits NCLEX-RN Review Question 3 – Rationale Rationale: Antipsychotic drugs such as risperiodne (Risperdal) treat the positive and negative effects of the underlying mental disorder.A decrease in delusional thinking, lessened hallucinations, and overall improvement in mental thought processes should be noted. Improvement in sleep patterns, anxiety, and nutrition may be noted as secondary effects of treatment of the underlying thought disorder. Orthostatic hypotension, reflex tachycardia, or sedation are potential adverse effects. NCLEX-RN Review Question 5 Which of the following data collected by the nurse during the history and physical is a contraindication for a patient to receive fluphenazine (Permitil, Prolixin)? 1. 2. 3. 4. Diabetes mellitus Age older than 70 Bone marrow depression Hypertension NCLEX-RN Review Question 5 – Answer 1. 2. 3. 4. Diabetes mellitus Age older than 70 Bone marrow depression Hypertension NCLEX-RN Review Question 5 – Rationale Rationale: Fluphenazine (Prolixin) is a phenothiazine drug. Use is contraindicated in patients with CNS depression, bone marrow depression, and alcohol withdrawal. NCLEX-RN Review Question 6 A female, age 39, has been on haloperidol (Haldol) for 3 months for severe psychosis. The nurse is monitoring the patient for the development of acute dystonias with haloperidol, and will monitor for: 1. 2. 3. 4. Dry mouth, constipation, and blurred vision Pacing, squirming, or difficulty with gait such as bradykinesia Severe spasms of the muscles of the tongue, face, neck, or back Tremors, wormlike tongue movements, and involuntary lip puckering NCLEX-RN Review Question 6 – Answer 1. 2. 3. 4. Dry mouth, constipation, and blurred vision Pacing, squirming, or difficulty with gait such as bradykinesia Severe spasms of the muscles of the tongue, face, neck, or back Tremors, wormlike tongue movements, and involuntary lip puckering NCLEX-RN Review Question 6 – Rationale Rationale: Acute dystonias are characterized by acute spasms of the face, tongue, neck, or back. Dry mouth, constipation, and blurred vision are adverse effects related to anticholinergic activity. Pacing and squirming are signs of akathisia, and bradykinesia and tremors are symptoms of pseudoparkinsonism. Involuntary lip-puckering and wormlike movements of the tongue are symptomatic of tardive dyskinesias. Drug Therapy for Psychoses • Assessment • • • • Monitor client’s condition Obtain health assessment Ascertain past mental illness Obtain information on smoking and use of illegal drugs, alcohol, and caffeine • Ascertain current medications and dietary habits • Obtain baseline blood and urine samples • Assess family’s knowledge of psychoses and medication regimen Drug Therapy for Psychoses (continued) • Planning • Goal is to remain compliant with medication regimen and free of symptoms • Implementation • Encourage compliance with medication regimen • Provide additional education Drug Therapy for Psychoses (continued) • Evaluation • Client to remain free of symptoms related to psychoses • Client to verbalize importance of taking prescribed medications Nursing Process Focus: Patients Receiving Conventional Antipsychotic Therapy Nursing Process Focus: Patients Receiving Conventional Antipsychotic Therapy Nursing Process Focus: Patients Receiving Conventional Antipsychotic Therapy Nursing Process Focus: Patients Receiving Conventional Antipsychotic Therapy Nursing Process Focus: Patients Receiving Conventional Antipsychotic Therapy Nursing Process Focus: Patients Receiving Conventional Antipsychotic Therapy Nursing Process Focus: Patients Receiving Conventional Antipsychotic Therapy Nursing Process Focus: Patients Receiving Atypical Antipsychotic Therapy Nursing Process Focus: Patients Receiving Atypical Antipsychotic Therapy Nursing Process Focus: Patients Receiving Atypical Antipsychotic Therapy Nursing Process Focus: Patients Receiving Atypical Antipsychotic Therapy Nursing Process Focus: Patients Receiving Atypical Antipsychotic Therapy Nursing Process Focus: Patients Receiving Atypical Antipsychotic Therapy Nursing Process Focus: Patients Receiving Atypical Antipsychotic Therapy