Path Chapter_4 [4-20
advertisement

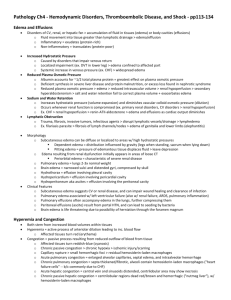
Lisa Stevens, D.O. Part 1 60% of lean body weight is water Two thirds of the body's water is intracellular Remainder is in extracellular compartments About 5% of total body water is in blood plasma Movement of water and low molecular weight solutes (salts) Between the intravascular and interstitial spaces Controlled primarily by opposing effect of: Vascular hydrostatic pressure Plasma colloid osmotic pressure Increased interstitial fluid Increased capillary pressure Diminished colloid osmotic pressure Fluid accumulation Movement of water into tissues (or body cavities) exceeds drainage Abnormal increase in interstitial fluid within tissues Edema Fluid collections in the different body cavities Hydrothorax Hydropericardium Hydroperitoneum (ascites) Anasarca Severe and generalized edema Widespread subcutaneous tissue swelling Transudate Edema caused by: Increased hydrostatic pressure Reduced plasma protein Typically a protein-poor fluid Heart failure, renal failure, hepatic failure, and certain forms of malnutrition Inflammatory edema Protein-rich exudate Result of increased vascular permeability Lymphedema Impaired lymphatic drainage Typically localized Causes Chronic inflammation with fibrosis Invasive malignant tumors Physical disruption Radiation damage Certain infectious agents Parasitic filariasis Lymphatic obstruction • Extensive inguinal lymphatic and lymph node fibrosis • Edema of the external genitalia and lower limbs • Massive = elephantiasis Severe edema of the upper extremity Complicate surgical removal and/or irradiation Breast and associated axillary lymph nodes • Breast cancer Morphology Edema is easily recognized grossly Microscopic examination Clearing and separation of the extracellular matrix Subtle cell swelling Most commonly seen: Subcutaneous tissues, lungs, and brain Subcutaneous edema Diffuse or more conspicuous in regions with high hydrostatic pressures Distribution is influenced by gravity Dependent edema • Legs when standing, the sacrum when recumbent Subcutaneous edema Pitting edema Finger pressure over substantially edematous subcutaneous tissue Displaces the interstitial fluid and leaves a depression Edema secondary to renal dysfunction Affect all parts of the body Manifests in tissues with loose connective tissue matrix (eyelids) Periorbital edema • Characteristic finding in severe renal disease Soft tissue edema Important because it signals underlying cardiac or renal disease Impairs wound healing or the clearance of infection Pulmonary edema Lungs are often two to three times their normal weight Sectioning yields frothy, blood-tinged fluid Mixture of air, edema, and extravasated red cells Common clinical problem Most frequently seen with left ventricular failure Pulmonary edema Lungs are often two to three times their normal weight Sectioning yields frothy, blood-tinged fluid Mixture of air, edema, and extravasated red cells Common clinical problem Most frequently seen with left ventricular failure Brain edema Localized or generalized Depending on the nature and extent of the pathologic process or injury Generalized edema Brain is grossly swollen with narrowed sulci Distended gyri show evidence of compression against the unyielding skull Brain edema Life-threatening Severe edema Brain substance can herniate (extrude) • Foramen magnum Brain stem vascular supply can be compressed Either condition can injure the medullary centers • Cause death Stem from locally increased blood volumes Hyperemia Active process Arteriolar dilation Sites of inflammation Skeletal muscle during exercise Hyperemia Leads to increased blood flow Affected tissues turn red (erythema) Engorgement of vessels with oxygenated blood Congestion Passive process Reduced outflow of blood from a tissue Systemic Cardiac failure Congestion Local Isolated venous obstruction Dusky reddish-blue color (cyanosis) Red cell stasis Accumulation of deoxygenated hemoglobin Long-standing chronic passive congestion Lack of blood flow causes chronic hypoxia Results in ischemic tissue injury and scarring Capillary rupture Cause small hemorrhagic foci Subsequent catabolism of extravasated red cells • Leave residual telltale clusters of hemosiderin-laden macrophages Morphology Cut surfaces Discolored due to the presence of high levels of poorly oxygenated blood Microscopic examination Acute pulmonary congestion • Engorged alveolar capillaries • Alveolar septal edema • Focal intra-alveolar hemorrhage Morphology Microscopic examination Chronic pulmonary congestion • Septa are thickened and fibrotic • Alveoli often contain numerous hemosiderin-laden macrophages Heart failure cells Morphology Acute hepatic congestion Central vein and sinusoids are distended Centrilobular hepatocytes can be frankly ischemic Chronic passive hepatic congestion Centrilobular regions are grossly red-brown • Areas are accentuated against uncongested parenchyma • Nutmeg liver Morphology Microscopic examination Centrilobular hemorrhage Hemosiderin-laden macrophages Degeneration of hepatocytes Extravasation of blood into the extravascular space Increased tendency to hemorrhage (usually with insignificant injury) Occurs in a variety of clinical disorders Collectively called hemorrhagic diatheses Distinct patterns of tissue hemorrhage Hemorrhage may be external Contained within a tissue Hematoma Petechiae Minute 1- to 2-mm hemorrhages into skin, mucous membranes, or serosal surfaces Most commonly associated: Locally increased intravascular pressure Low platelet counts (thrombocytopenia) Defective platelet function (as in uremia) Purpura Slightly larger (≥3 mm) hemorrhages Associated with many of the same disorders that cause petechiae Secondary to trauma, vascular inflammation (vasculitis), or increased vascular fragility (amyloidosis) Ecchymoses Larger (>1 to 2 cm) subcutaneous hematomas (bruises) Red cells in these lesions are degraded and phagocytized by macrophages Hemoglobin (red-blue color) • Enzymatically converted into bilirubin (blue-green color) Hemosiderin (gold-brown color), accounting for the characteristic color changes in a bruise Large accumulation of blood in a body cavity Hemothorax Hemopericardium Hemoperitoneum Hemarthrosis (in joints) Normal hemostasis Consequence of tightly regulated processes Maintain blood in a fluid state in normal vessels Permit the rapid formation of a hemostatic clot at the site of a vascular injury Thrombosis Pathologic counterpart of hemostasis Involves blood clot (thrombus) formation Both hemostasis and thrombosis involve three components: Vascular wall (particularly the endothelium) Platelets Coagulation cascade Endothelial cells Key players in the regulation of homeostasis Exhibit antiplatelet, anticoagulant, and fibrinolytic properties After injury or activation Acquire numerous procoagulant activities Activated by infectious agents, hemodynamic forces, plasma mediators, and cytokines Antiplatelet effects Intact endothelium prevents platelets from engaging the highly thrombogenic subendothelial ECM Nonactivated platelets Do not adhere to endothelial cells • Even if platelets are activated, prostacyclin (PGI2) and nitric oxide produced by the endothelial cells impede platelet adhesion Antiplatelet effects Endothelial cells Also elaborate adenosine diphosphatase • Degrades adenosine diphosphate (ADP) • Further inhibits platelet aggregation Anticoagulant effects Mediated by endothelial membrane-associated heparin-like molecules Thrombomodulin • Binds to thrombin • Converts it from a procoagulant into an anticoagulant Via its ability to activate protein C, which inhibits clotting by inactivating factors Va and VIIIa Anticoagulant effects Mediated by endothelial membrane-associated heparin-like molecules Tissue factor pathway inhibitor • Cell surface protein • Directly inhibits tissue factor-factor VIIa and factor Xa activities Anticoagulant effects Heparin-like molecules Act indirectly Cofactors that enhance the inactivation of thrombin and several other coagulation factors • Through the use of plasma protein antithrombin III Fibrinolytic effects Endothelial cells synthesize tissue-type plasminogen activator (t-PA) Protease that cleaves plasminogen to form plasmin • Plasmin cleaves fibrin to degrade thrombi Platelet effects Endothelial injury allows platelets to contact the underlying extracellular matrix Subsequent adhesion occurs through interactions with von Willebrand factor (vWF) Product of normal endothelial cells and an essential cofactor for platelet binding to matrix elements Procoagulant effects Response to cytokines (TNF or IL-1) or bacterial endotoxin Endothelial cells synthesize tissue factor • Major activator of the extrinsic clotting cascade • Activated endothelial cells Augment the catalytic function of activated coagulation factors IXa and Xa Antifibrinolytic effects Endothelial cells secrete inhibitors of plasminogen activator (PAIs) Limit fibrinolysis and tend to favor thrombosis Intact, nonactivated endothelial cells inhibit platelet adhesion and blood clotting Endothelial injury or activation Results in a procoagulant phenotype that enhances thrombus formation Disc-shaped Anucleate cell fragments Shed from megakaryocytes in the bone marrow into the blood stream Play a critical role in normal hemostasis Forming the hemostatic plug that initially seals vascular defects Providing a surface that recruits and concentrates activated coagulation factors Function depends on several glycoprotein receptors Contractile cytoskeleton Two types of cytoplasmic granules α-Granules • Adhesion molecule P-selectin on their membranes • Contain fibrinogen, fibronectin, factors V and VIII, platelet factor 4, platelet-derived growth factor (PDGF), and transforming growth factor-β (TGF-β) Function depends on several glycoprotein receptors Two types of cytoplasmic granules Dense (or δ) granules • Contain ADP and ATP, ionized calcium, histamine, serotonin, and epinephrine Following vascular injury… Platelets encounter ECM constituents Collagen and the adhesive glycoprotein vWF On contact with these proteins, platelets undergo: Adhesion and shape change Secretion (release reaction) Aggregation Mediated largely via interactions with vWF Acts as a bridge between platelet surface receptors (glycoprotein Ib) and exposed collagen vWF-GpIb associations Necessary to overcome the high shear forces of flowing blood Mediated largely via interactions with vWF Genetic deficiencies of vWF or its receptor result in bleeding disorders • Von Willebrand Disease • Bernard-Soulier syndrome Occurs soon after adhesion Various agonists can bind platelet surface receptors Initiate an intracellular protein phosphorylation cascade Leads to degranulation Various agonists can bind platelet surface receptors Release of the contents of dense-bodies Important Calcium is required in the coagulation cascade ADP is a potent activator of platelet aggregation • Causes additional ADP release Amplifies aggregation process Platelet activation Appearance of negatively charged phospholipids (particularly phosphatidylserine) on their surfaces Bind calcium and serve as critical nucleation sites for the assembly of complexes containing the various coagulation factors Follows adhesion and granule release Vasoconstrictor thromboxane A2 Important platelet-derived stimulus Amplifies platelet aggregation Formation of the primary hemostatic plug Initial wave of aggregation is reversible Concurrent activation of the coagulation cascade Generates thrombin Stabilizes the platelet plug via two mechanisms: Thrombin binds to a protease-activated receptor on the platelet membrane • In concert with ADP and TxA2 causes further platelet aggregation Stabilizes the platelet plug via two mechanisms: Thrombin binds to a protease-activated receptor on the platelet membrane Platelet contraction • Event that is dependent on the platelet cytoskeleton • Creates an irreversibly fused mass of platelets • Constitutes the definitive secondary hemostatic plug Thrombin converts fibrinogen to fibrin in the vicinity of the platelet plug • Cements the platelets in place Noncleaved fibrinogen Important component of platelet aggregation Platelet activation by ADP Triggers a conformational change in the platelet GpIIb-IIIa receptors Induces binding to fibrinogen Large protein that forms bridging interactions between platelets that promote platelet aggregation Lisa Stevens, D.O. Part 2 Third arm of the hemostatic process Amplifying series of enzymatic conversions Each step proteolytically cleaves an inactive proenzyme into an activated enzyme Culminates in thrombin formation Thrombin is the most important coagulation factor Can act at numerous stages in the process Conclusion of the proteolytic cascade Thrombin converts the soluble plasma protein fibrinogen into fibrin monomers that polymerize into an insoluble gel Fibrin gel encases platelets and other circulating cells in the definitive secondary hemostatic plug Fibrin polymers are covalently cross-linked and stabilized by factor XIIIa (which itself is activated by thrombin) Assess the function of the two arms of the coagulation pathway Two standard assays Prothrombin time (PT) Partial thromboplastin time (PTT) The PT assay Assesses the function of the proteins in the extrinsic pathway Factors VII, X, II, V, and fibrinogen Accomplished by adding tissue factor and phospholipids to citrated plasma (sodium citrate chelates calcium and prevents spontaneous clotting) Coagulation is initiated by the addition of exogenous calcium and the time for a fibrin clot to form is recorded Partial thromboplastin time (PTT) Screens for the function of the proteins in the intrinsic pathway Factors XII, XI, IX, VIII, X, V, II, and fibrinogen Clotting is initiated through the addition of negative charged particles (ground glass) • Activates factor XII (Hageman factor), phospholipids, and calcium, and the time to fibrin clot formation is recorded Thrombin Exerts a wide variety of proinflammatery effects Most effects of thrombin occur through its activation of a family of protease activated receptors (PARs) Belong to the seven-transmembrane G proteincoupled receptor family PARs are expressed on endothelium, monocytes, dendritic cells, T lymphocytes, and other cell types Coagulation cascade must be restricted to the site of vascular injury Prevent runaway clotting of the entire vascular tree Three categories of endogenous anticoagulants Antithrombins (antithrombin III) Inhibit the activity of thrombin and other serine proteases, including factors IXa, Xa, XIa, and XIIa Antithrombin III is activated by binding to heparin-like molecules on endothelial cells • Clinical usefulness of administering heparin to minimize thrombosis Three categories of endogenous anticoagulants Proteins C and S Vitamin K-dependent proteins Act in a complex that proteolytically inactivates factors Va and VIIIa TFPI is a protein produced by endothelium Inactivates tissue factor-factor VIIa complexes Fine-tune the coagulation/anticoagulation balance Releasing plasminogen activator inhibitor (PAI) Blocks fibrinolysis by inhibiting t-PA binding to fibrin Confers an overall procoagulant effect Production is increased by thrombin as well as certain cytokines Three primary abnormalities that lead to thrombus formation (called Virchow's triad): Endothelial injury Stasis or turbulent blood flow Hypercoagulability of the blood Particularly important for thrombus formation in the heart or the arterial circulation Normally high flow rates might otherwise impede clotting by preventing platelet adhesion and washing out activated coagulation factors Endothelial cell injury Thrombus formation within cardiac chambers (i.e. after endocardial injury due to myocardial infarction) Over ulcerated plaques in atherosclerotic arteries Sites of traumatic or inflammatory vascular injury (vasculitis) Endothelium Does not need to be denuded or physically disrupted to contribute to the development of thrombosis Any perturbation in the dynamic balance of the prothombotic and antithrombotic activities of endothelium can influence local clotting events Endothelial dysfunction Induced by a wide variety of insults Hypertension Turbulent blood flow Bacterial endotoxins Radiation injury Metabolic abnormalities • Homocystinemia or hypercholesterolemia Toxins absorbed from cigarette smoke Turbulence Contributes to arterial and cardiac thrombosis by causing endothelial injury or dysfunction Forming countercurrents and local pockets of stasis Stasis is a major contributor in the development of venous thrombi Normal blood flow is laminar Platelets (and other blood cellular elements) Flow centrally in the vessel lumen • Separated from endothelium by a slower moving layer of plasma Stasis and turbulence therefore: Promote endothelial activation Enhancing pro-coagulant activity Disrupt laminar flow Bring platelets into contact with the endothelium Prevent washout and dilution of activated clotting factors Fresh flowing blood Inflow of clotting factor inhibitors AKA thrombophilia Less frequent contributor to thrombotic states Any alteration of the coagulation pathways that predisposes to thrombosis Divided into primary (genetic) Secondary (acquired) disorders Inherited causes Most common Point mutations in the factor V gene Prothrombin gene Elevated levels of homocysteine Contribute to arterial and venous thrombosis Prothrombotic effects of homocysteine Due to thioester linkages Between proteins homocysteine metabolites and a variety of Rare inherited causes of primary hypercoagulability Deficiencies of anticoagulants Antithrombin III, protein C, or protein S Clinical presentation • Begins in adolescence or early adulthood • Venous thrombosis • Recurrent thromboembolism Acquired thrombophilic states Heparin-induced thrombocytopenia (HIT) syndrome Occurs following the administration of unfractionated heparin • May induce the appearance of antibodies Recognize complexes of heparin and platelet factor 4 on the surface of platelets Heparin-induced thrombocytopenia (HIT) syndrome Occurs following the administration of unfractionated heparin • Complexes of heparin-like molecules and platelet factor 4-like proteins on endothelial cells • Binding of these antibodies to platelets Results in their activation, aggregation, and consumption Prothrombotic state, even in the face of heparin administration and low platelet counts AKA lupus anticoagulant syndrome Clinical manifestations Recurrent thromboses, repeated miscarriages, cardiac valve vegetations, and thrombocytopenia Pulmonary embolism, pulmonary hypertension, stroke, bowel infarction, or renovascular hypertension Fetal loss Autoantibodies induce a hypercoagulable state Cause endothelial injury Directly activates platelets and complement Primary and secondary forms Secondary antiphospholipid syndrome Individuals with a well-defined autoimmune disease Systemic lupus erythematosus Primary and secondary forms Primary antiphospholipid syndrome Exhibit only the manifestations of a hypercoagulable state Lack evidence of other autoimmune disorders Association with certain drugs or infections Can develop anywhere in the cardiovascular system Size and shape of thrombi Depend on the site of origin and the cause Arterial or cardiac thrombi Begin at sites of turbulence or endothelial injury Venous thrombi Occur at sites of stasis Focally attached to the underlying vascular surface Arterial thrombi Grow retrograde from the point of attachment Venous thrombi Extend in the direction of blood flow Gross and microscopic laminations Lines of Zahn Represent pale platelet and fibrin deposits alternating with darker red cell-rich layers Signify that a thrombus has formed in flowing blood Presence can therefore distinguish antemortem thrombosis from the bland nonlaminated clots that occur postmortem Thrombi occurring in heart chambers or in the aortic lumen Mural thrombi Abnormal myocardial contraction • Arrhythmias, dilated cardiomyopathy, or myocardial infarction • Endomyocardial injury (myocarditis or catheter trauma) Arterial thrombi Frequently occlusive Most common sites Coronary, cerebral, and femoral arteries Friable meshwork of platelets, fibrin, red cells, and degenerating leukocytes Superimposed on a ruptured atherosclerotic plaque Venous thrombosis (phlebothrombosis) Invariably occlusive Thrombus forming a long cast of the lumen Thrombi form in the sluggish venous circulation Contain more enmeshed red cells Red, or stasis, thrombi Veins of the lower extremities are most commonly involved (90% of cases) Postmortem clots Mistaken for antemortem venous thrombi Gelatinous with a dark red dependent portion Red cells have settled by gravity Yellow "chicken fat" upper portion Usually not attached to the underlying wall Red thrombi Firmer Focally attached Gross and/or microscopic lines of Zahn Vegetations Thrombi on heart valves Blood-borne bacteria or fungi Adhere to previously damaged valves (rheumatic heart disease) Directly cause valve damage Infective endocarditis Vegetations Sterile vegetations Nonbacterial thrombotic endocarditis Sterile, verrucous endocarditis Libman-Sacks endocarditis Survival of the initial thrombosis Ensuing days to weeks thrombi undergo some combination of the following four events: Propagation • Thrombi accumulate additional platelets and fibrin Embolization • Thrombi dislodge and travel to other sites in the vasculature Dissolution • Result of fibrinolysis Leads to shrinkage and total disappearance of recent thrombi Organization and recanalization • Older thrombi become organized by the ingrowth of endothelial cells, smooth muscle cells, and fibroblasts Deep venous thrombosis (DVT) Larger leg veins-at or above the knee Thrombi more often embolize to the lungs Give rise to pulmonary infarction Venous obstructions from DVTs can be rapidly offset by collateral channels DVTs are asymptomatic in approximately 50% of affected individuals Recognized only in retrospect after embolization Obstetric complications to advanced malignancy Sudden or insidious onset of widespread fibrin thrombi in the microcirculation Not grossly visible Diffuse circulatory insufficiency, particularly in the brain, lungs, heart, and kidneys Widespread microvascular thrombosis results in platelet and coagulation protein consumption Fibrinolytic mechanisms are activated Initially thrombotic disorder Evolve into a bleeding catastrophe Embolus Detached intravascular solid, liquid, or gaseous mass Carried by the blood to a site distant from its point of origin Thromboembolism Rare forms of emboli Fat droplets, nitrogen bubbles, atherosclerotic debris (cholesterol emboli), tumor fragments, bone marrow, or foreign bodies Unless otherwise specified, emboli should be considered thrombotic in origin Occlusions—embolic 95% from deep leg veins Indwelling central venous lines Right atrial thrombi 50,000 deaths/year in US Origin of emboli Leg or pelvic veins Large emboli Sudden death Lodging • Major branches of pulmonary arteries • Saddle emboli Acute cor pulmonale Small emboli Minimal symptoms Exception Inadequate bronchial circulation • Symptoms Causes of emboli Immobilized individuals Hypercoagulable state (primary vs. secondary) Heart failure Extent of pulmonary artery obstruction Size of occluded vessel Pathophysiologic response Clinical significance Number of emboli Status of the cardiovascular system Release of vasoactive factors Pathophysiologic consequences Respiratory compromise Hemodynamic compromise Adequate cardiovascular function Bronchial artery compensation Hemorrhage without infarction Infarction Inadequate circulation Rare in young Clinical course Cardiopulmonary resuscitation Electromechanical dissociation • Electrocardiogram has a rhythm • No pulses are palpated Survival (post-sizable pulmonary embolus) Mimics myocardial infarction Diagnosis Spiral CT Other diagnostic methods Ventilation perfusion scanning Pulmonary angiography Duplex ultrasonography • Deep vein thrombosis Prevention Major clinical problem Prophylactic therapy Early ambulation Stockings Anticoagulation Filter Treatment Thrombolysis Anticoagulation Gross examination Parenchyma 75% of all infarcts affect the lower lobes Greater than 50%--multiple lesions Wedge shaped Hemorrhagic Fibrinous pleural exudate Scar Embolus http://www.path.uiowa.edu/cgi-bin-pub/vs/fpx_gen.cgi?slide=714&viewer=java&lay=&jpg=493 Microscopic examination Ischemic necrosis Alveolar walls, bronchioles, and vessels Infected embolus Intense neutrophilic inflammatory reaction Septic infarct Microscopic fat globules-with or without associated hematopoietic marrow elements Fractures of long bones (which have fatty marrow) Soft tissue trauma and burns Common incidental findings after vigorous cardiopulmonary resuscitation No clinical consequence Gas bubbles within the circulation Coalesce to form frothy masses Obstruct vascular flow (causes distal ischemic injury) More than 100 cc of air Required to have a clinical effect in the pulmonary circulation Decompression sickness Sudden At decreases in atmospheric pressure risk: • Scuba and deep sea divers, underwater construction workers, and individuals in unpressurized aircraft in rapid ascent The bends Rapid formation of gas bubbles within skeletal muscles and supporting tissues in and about joints The chokes Gas bubbles in the vasculature Causes edema, hemorrhage, and focal atelectasis or emphysema, leading to a form of respiratory distress Caisson disease Chronic form of decompression sickness Named for the pressurized vessels used in the bridge construction Workers in these vessels suffered both acute and chronic forms of decompression sickness Persistence of gas emboli in the skeletal system Leads to multiple foci of ischemic necrosis More common sites • Femoral heads, tibia, and humeri Amniotic fluid embolism Ominous complication of labor and the immediate postpartum period Sudden severe dyspnea, cyanosis, and shock Followed by neurologic impairment ranging from headache to seizures and coma If the patient survives the initial crisis, pulmonary edema typically develops, along with (in half the patients) DIC, as a result of release of thrombogenic substances from the amniotic fluid Underlying cause Infusion of amniotic fluid or fetal tissue into the maternal circulation via a tear in the placental membranes or rupture of uterine veins Classic findings Presence of squamous cells shed from fetal skin, lanugo hair, fat from vernix caseosa, and mucin derived from the fetal respiratory or gastrointestinal tract in the maternal pulmonary microvasculature Final common pathway for several potentially lethal clinical events Severe hemorrhage, extensive trauma or burns, large myocardial infarction, massive pulmonary embolism, and microbial sepsis Clinical findings Systemic hypotension Due to reduced cardiac output or to reduced effective circulating blood volume Consequences Impaired tissue perfusion and cellular hypoxia Three general categories Cardiogenic shock Hypovolemic shock Septic shock Depend on the precipitating insult Hypovolemic and cardiogenic shock Patient presents with hypotension Weak, rapid pulse; tachypnea Cool, clammy, cyanotic skin Septic shock Skin may initially be warm and flushed because of peripheral vasodilation Cardiac, cerebral, and pulmonary changes secondary to shock worsen the problem Electrolyte disturbances and metabolic acidosis