Slides - Healthcare Analytics Summit
advertisement
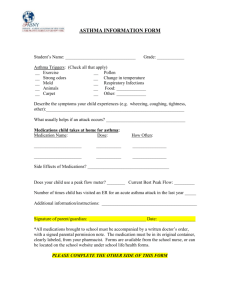
The Imperative of Linking Clinical and Financial Data to Improve Outcomes Charles G. Macias M.D., M.P.H. Chief Clinical Systems Integration Officer, Texas Children’s Hospital Learning objectives Assess the effectiveness of an organization’s quality gaps to ensure organizational readiness, drive efficiency and leverage opportunities to improve quality. Illustrate how a blend of clinical and financial data informed by analytics from an enterprise data warehouse can improve outcomes. Describe how an EDW and care process implementation can encourage a culture of quality and safety, providing physicians with the necessary tools to integrate financial relevance into the practice of delivering high-quality healthcare. Discuss how strategy for integration of science, data and predictive analytics and operational improvement through improvement science can transform a system towards the triple aim. Jenny Jones and the Challenges of a Fragmented System Within six months, Jenny had visited: One PCP Two Hospitals Three ERs Leading to: Six different Asthma Action Plans with conflicting discharge instructions Quality Defined 1 Institute of Medicine domains: Safe Effective Efficient Timely Patient centered Equitable 2 The degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge. – Lohr, K.N., & Schroeder, S.A. (1990). A strategy for quality assurance in Medicare. New England Journal of Medicine, 322 (10):707-712. 3 Importance of minimizing unintended variation in health care delivery The Healthcare Value Equation In an environment where cost is marginally increasing, healthcare must markedly improve quality. Adoption of EMRs and clinical systems should help push the quality agenda but alone may not be enough to deliver data intelligence. Quality Value = Cost 4 In Second Look, Few Savings from Digital Health Records New York Times: January 10, 2013 2005 RAND report forecasts $81 billion annual U.S. savings. “Seven years later the empirical data on the technology’s impact on health care efficiency and safety are mixed, and annual health care expenditures in the United States have grown by $800 billion.” Disappointing performance of health IT to date largely attributed to: Sluggish adoption of health IT systems, coupled with the choice of systems that are neither interoperable nor easy to use; The failure of health care providers and institutions to reengineer care processes to reap the full benefits of health IT. EHRs, Red Tape Eroding Physician Job Satisfaction Most physicians express frustration with the failure to provide efficiency. 20% want to return to paper 5 Variation in Care Describing variation in care in three pediatric diseases: gastroenteritis, asthma, simple febrile seizure Pediatric Health Information System database (for data from 21 member hospitals) Two quality-of-care metrics measured for each disease process Wide variations in practice Increased costs were NOT associated with lower admission rates or 3-day ED revisit rates Implications? Optimal care may be delivered at a lower cost than today’s care! Kharbanda AB, Hall M, Shah SS, Freedman SB, Mistry RD, Macias CG, Bonsu B, Dayan PS, Alessandrini EA, Neuman MI. Variation in resource utilization across a national sample of pediatric emergency departments. J Pediatr. 2013 6 Consumer Care/Cost Uncertainty Consumers: Trust their physicians Hope for the best Struggle to understand cost and care Don’t often know what they are getting Don’t always get great outcomes Value is what they want 7 Challenge of Healthcare Physicians are: Driven by science and key values Overwhelmed with medical literature Not well trained to turn that experience into high quality patient outcomes Transparency of local data is part of the solution! 8 Poll Question #1 In your organization, what percentage of patient visits are your physicians talking about cost and care tradeoffs at the bedside? a) 0-19% b) 20-39% c) 40-59% d) 60-79% e) 80-100% f) Unsure or not applicable 9 Physicians and Care Cost Patient values and preferences Evidence Clinical Expertise Resource issues Source: SAEM. Evidence Based Medicine Online Course 2005 Physician preferences Once taboo, physicians should take cost into consideration: No Money No Mission No Expansion And so providers must….. Understand what creates improvements Understand the story that their data tells. 11 No Innovation About Texas Children’s Hospital Statistics Number of Beds 469 Annual Inpatient Admissions 21,744 Annual Outpatient Visits 1.44 million Emergency Room Visits 82,049 Inpatient Surgeries 8,655 Outpatient Surgeries 14,439 A data management strategy to improve outcomes IMPROVED OUTCOMES from high quality of care Patient centric outcomes and institutional outcomes achieved DEPLOYMENT SYSTEM Operations Evidence Based Guidelines and Order sets, Clinical Decision Support, patient and provider materials CLINICAL CONTENT SYSTEM Science and evidence ANALYTIC SYSTEM Data analytics and collaborative data SOURCE SYSTEMS (e.g. EMR, Financial, Costing, Patient Satisfaction) Advanced Quality Improvement course, QI curriculum, Care process teams Informatics, Electronic Data Warehousing Creating a foundation for EB practice IMPROVED OUTCOMES from high quality of care Evidence Based Guidelines and Order sets, Clinical Decision Support, patient and provider materials DEPLOYMENT SYSTEM Operations CLINICAL CONTENT SYSTEM Science and evidence ANALYTIC SYSTEM Data analytics and collaborative data SOURCE SYSTEMS (e.g. EMR, Financial, Costing, Patient Satisfaction) Evidence-Based Guidelines: EBOC Acute Chest Syndrome Acute Gastroenteritis Acute Heart Failure Acute Hematogenous Osteomyelitis Acute Ischemic Stroke Acute Otitis Media Central Line-Associated Bloodstream Infections Closed Head Injury Community-Acquired Pneumonia Cystic Fibrosis – Nutrition/GI >12 y/o Appendicitis Autism Assessment and Diagnosis Arterial Thrombosis C-spine Assessment Asthma Intraosseus Line Placement Bronchiolitis IV Lock Therapy Cancer Center Procedural Management Postpartum Hemorrhage Cardiac Thrombosis Deep Vein Thrombosis Diabetic Ketoacidosis Fever and Neutropenia in Children with Cancer Fever Without Localizing Signs (FWLS) 0-60 Days Fever Without Localizaing Signs (FWLS) 2-36 Months Housewide Procedural Sedation Hyperbilirubinemia Neonatal Thrombosis Nutrition/Feeding in the Post-Cardiac Neonate Rapid Sequence Intubation Skin and Soft Tissue Infection Status Epilepticus Tracheostomy Management Urinary Tract Infection Poll Question #2 In ambulatory settings, what is the best estimate for the percentage of questions for which evidence exists to answer clinical questions that affect the decision to treat? a) 5% b) 10% c) 15% d) 25% e) 50% f) Unsure or not applicable 16 Creating a foundation for data use IMPROVED OUTCOMES from high quality of care DEPLOYMENT SYSTEM Operations CLINICAL CONTENT SYSTEM Science and evidence ANALYTIC SYSTEM Data analytics and collaborative data SOURCE SYSTEMS (e.g. EMR, Financial, Costing, Patient Satisfaction) Informatics, Electronic Data Warehousing TCH’s EDW Architecture Metadata: EDW Atlas Security and Auditing Common, Linkable Vocabulary; Late binding FINANCIAL SOURCES (e.g. EPSi,) Financial Source Marts ADMINISTRATIVE SOURCES (e.g. API Time Tracking) Administrative Source Marts • • • • • • • • EMR Source Marts EMR SOURCE (e.g. Epic) Clinical Asthma Appendectomy Deliveries Pneumonia Diabetes Surgery Neonatal dz Transplant DEPARTMENTAL SOURCES (e.g. Sunquest Labs) Departmental Source Marts Operations • Labor productivity • Radiology • Practice Mgmt • Financials • Patient Satisfaction • + others Patient Source Marts PATIENT SATISFACTION SOURCES (e.g. NRC Picker, HR Source Mart Human Resources (e.g. PeopleSoft) Creating a foundation for QI deployment IMPROVED OUTCOMES from high quality of care Advanced Quality Improvement course, QI curriculum, Care process teams DEPLOYMENT SYSTEM Operations CLINICAL CONTENT SYSTEM Science and evidence ANALYTIC SYSTEM Data analytics and collaborative data Avenues for Dissemination QUALITY LEADERS National Programs and Partnerships ADVANCED INTERMEDIATE Classroom (e.g. AQI Program, Six Sigma Green Belt) •Project Required Online and Classroom (IHI Educational Resources, PEDI 101, EQIPP, Fellows College) •Project Required BEGINNER Online and Classroom (e.g. Nursing IMPACT (QI Basic). OJO Educational Resources, Lean Awareness Training) NEW Classroom and Department (e.g. New Employee Orientation, e-Learning, Unit/Department-based training) Changes that result in process improvement Improvement Ideas Adapted from: The Improvement Guide: A Practical Approach to Enhancing Organizational Performance, 2nd Ed. Gerald J. Langley, Ronald D. Moen, Kevin M. Nolan, Thomas W. Nolan, Clifford L. Norman, and Lloyd P. Provost; Jossey-Bass 2009 Pareto 80/20 Principle in Healthcare Amount of Variation TCH’s Care Process Analysis Asthma Size of Clinical Process Improvement Opportunity: Large processes with significant variation Bubble Size = Case Count Driving clinical care improvement: linking science, data management, operations Clinical Program Guidelines centered on evidence-based care MD Lead #5 Care Process MD Lead #4 Care Process MD Lead #3 Care Process MD Lead MD Lead #2 Care Process Operation s Lead Domain MD Lead #1 Care Process Clinical Director Data Manager Outcomes Analyst BI Developer Data Architect Permanent, integrated teams composed of clinicians, technologists, analysts and quality improvement personnel drive adoption of evidence-based medicine and achieve and sustain superior outcomes. Application Service Owner Balanced scorecard-expanded visualizations 3. 1. Care Process Defined 2. Current Literature Research 5. Group Creates Final Scorecard 4. Individual Ratings Aggregate Ratings Severity Adjusted Variation Data Drives Waste Reduction: Alternative Approaches 1.96 std Mean # of Cases 1 box = 100 cases in a year Excellent Outcomes # of Cases Poor Outcomes Excellent Outcomes Poor Outcomes Option 1: Focus on Outliers – the prescriptive approach Strategy eliminate the unfavorable tail of the curve (“quality assurance”) Result Ithe impact is minimal 27 Alternative Approaches to Waste Reduction Mean # of Cases 1 box = 100 cases in a year Excellent Outcomes # of Cases Poor Outcomes Excellent Outcomes Poor Outcomes Option 2: Focus On Inliers – improving quality outcomes across the majority Strategy Evidence and analytics applied through EBP clinical standards targets inlier variation Result Shifting more cases towards excellent outcomes has much more significant impact 28 Improving Cost Structure Through Waste Reduction Ordering Waste Workflow Waste Defect Waste Ordering of tests that are neither diagnostic nor contributory Variation in Emergency Care wait time ADEs, transfusion reactions, pressure ulcers, HAIs, VTE, falls, wrong surgery 29 Care Redesign Methodology CXR utilization in patients with known asthma, steroids in bronchiolitis Quicker steroid delivery for status asthmaticus, goal directed therapy for septic shock Evidence Supports Evidence equivocal Hypertonic saline and bronchodilators in select patients with bronchiolitis Evidence against 30 Asthma: Care Process Team Cohort, Percentage of Chest X-rays Ordered* (Oct. 2010 - Ap r. 2013) 80% 70% Percentage 60% 51% 50% 40% 35% 30% 20% Feedba ck of ra tes to hospita lists a nd Emergency Center clinicia ns Order set revisions 10% Apr. 13 Mar. 13 Feb. 13 Jan. 13 Dec. 12 Nov. 12 Oct. 12 Sep. 12 Aug. 12 Jul. 12 Jun. 12 May. 12 Apr. 12 Mar. 12 Feb. 12 Jan. 12 Dec. 11 Nov. 11 Oct. 11 Sep. 11 Aug. 11 Jul. 11 Jun. 11 May. 11 Apr. 11 Mar. 11 Feb. 11 Jan. 11 Dec. 10 Nov. 10 Oct. 10 0% Month yea r * Inpa tient, Emergency Center (EC) a nd observa tion pa tients (Ca re Process Tea m cohort), P-Cha rt ba sed upon EDW da ta extra ction of 5/14/2013 (M& W). 31 Improving Cost Structure Through Waste Reduction Ordering Waste Workflow Waste Defect Waste Ordering of tests that are neither diagnostic nor contributory Variation in Emergency Care wait time ADEs, transfusion reactions, pressure ulcers, HAIs, VTE, falls, wrong surgery 32 Flow chart of a patient with acute gastroenteritis through the TCH Emergency Department: Existing process BEGIN Patient discharged home1 4 Does patient have vomiting &/ or diarrhea Patient presents to Emergency Dept (ED). 3 Patient transferred to inpatient bed2 Evaluate per clinical symptoms Fellow/ Attending does pretransfer check PCA checks vital signs Patient registers Triage nurse does the following: · Vitals What is the patient’s level of dehydration? Patient waiting Key: ___ solid arrow indicates “yes” _ _ broken arrow indicates “no” 1 2 3 4 4 Outcome: Outcome: Outcome: Outcome: Outcome: Time in ED Time to inpatient bed Length of stay (LOS) Revisit from ED discharge Revisit from inpatient discharge Nurse-Nurse checkout occurs Nurse discharges patient Bed approved Patient evaluated by triage nurse PCA checks vital signs ED secretary requests bed Mild or Moderate dehydration Severe dehydration MD does discharge orders MD does admission orders Is the patient vomiting? Put patient in ED room Decision to discharge patient Triage nurse does the following: · Give Zofran · Provide gatorade/pedialyte Decision to admit patient Triage nurse does the following: · Nothing or give patient gatorade/ pedialyte Is the patient ok for discharge? Follow TCH AGE clinical algorithm Patient waiting Patient put in ED room Patient evaluated by nurse Patient evaluated by Medical student Patient evaluated by ED resident Patient evaluated by ED fellow Process map before EBG Patient evaluated by ED attending Modified: 7/21/2009 Flow chart of a patient with acute gastroenteritis through the TCH Emergency Deparment BEGIN 4 Does patient have vomiting &/ or diarrhea Patient presents to Emergency Dept (ED). Patient discharged home1 3 Patient transferred to inpatient bed2 Evaluate per clinical symptoms Fellow/ Attending does pretransfer check PCA checks vital signs Patient registers Key: ___ solid arrow indicates “yes” _ _ broken arrow indicates “no” Triage nurse does the following: · Vitals · Assess dehydration (Gorelick score)** ** New process 1 Outcome: Time in ED 2 Outcome: Time to inpatient bed 3 Outcome: Length of stay (LOS) 4 Outcome: Revisit from ED discharge 4 Outcome: Revisit from inpatient discharge What is the patient’s level of dehydration? Patient waiting Patient evaluated by triage nurse Nurse-Nurse checkout occurs Nurse discharges patient Collect ORT tracking sheet PCA checks vital signs ED secretary requests bed Mild or Moderate dehydration Severe dehydration MD does discharge orders MD does admission orders Is the patient vomiting? Put patient in ED room Follow TCH AGE clinical algorithm Decision to discharge patient Triage nurse does the following: · Give Zofran · Provide patient education on ORT · Initiate ORT · Give ORT tracking sheet** Patient waiting Patient put in ED room Decision to admit patient Triage nurse does the following: · Provide patient education on ORT · Initiate ORT · Give ORT tracking sheet** Patient evaluated by nurse Bedside nurse does the following: · Assesses dehydration (Gorelick score)** · Monitors progress on ORT tracking sheet** · Reemphasizes patient education on ORT Patient evaluated by Medical student Bed approved Is the patient ok for discharge? Patient evaluated by ED resident Patient evaluated by ED fellow ED Fellow does the following: · Assesses dehydration (Gorelick score)** · Monitors progress on ORT tracking sheet** · Reemphasizes patient education on ORT · Determines patient disposition Patient evaluated by ED attending Process map after EBG Modified: 5/9/2009 35 Improving Cost Structure Through Waste Reduction Ordering Waste Workflow Waste Defect Waste Ordering of tests that are neither diagnostic nor contributory Variation in Emergency Care wait time ADEs, transfusion reactions, pressure ulcers, HAIs, VTE, falls, wrong surgery 36 Clinical Decision Support to Minimize Errors Streamlining and Improving Processes and Operations to Minimize Errors 37 Value = EC: Early administration of Dexamethasone Expanding evidence based practice -Provider and staff inservicing -Clinical decision support -Bridging a continuum for home care: second dose 10% decrease in TID Inpatient: prolonged LOS • • 35% reduction in LOS No change in 7 or 30 day readmission rate No change in days of school/days of work missed • • Direct variable cost ($60/hr) I-MR Chart of CT - 1st q3h to d/c by Phase Baseline Individual V alue 200 Improv ement Improv 1 ement 2 1 150 100 0 LC L=-16.1 1 13 25 37 49 85 97 109 121 Improv ement Improv 1 ement 2 1 M oving Range 61 73 O bser vation Baseline 200 Evidence based approach to early medication weaning U C L=70.9 _ X=27.4 5 50 1 150 100 U C L=53.4 __ M R=16.4 LC L=0 50 0 1 13 25 37 49 61 73 O bser vation 85 97 109 121 The continuum: improved patient experience and outcomes Improved time to first beta agonist (ED or inpatient arrival) • Increase chronic severity assessment Improve accuracy Increase appropriate controller prescriptions Clinical decision support • • • Increase influenza vaccination rate Increase number of culturally sensitive education encounters Increase number of social work/ legal support encounters • AAP use went from 20% to 44% in first cycle to 52% in second • ACT use went from 0% to 30% in first cycle to 41% in second • Severity classification went from 10% to 35% in first cycle to 54% in second Registry Financial Score Card 42 Asthma Care Outcomes Dashboard Financial conversations $5,000 $4,500 $4,000 $3,500 $3,000 $2,500 $2,000 $1,500 $1,000 $500 $0 -$500 -$1,000 -$1,500 -$2,000 -$2,500 -$3,000 -$3,500 -$4,000 -$4,500 -$5,000 Margin y = 106.48x - 855.25 2011 Q1 2011 Q2 2011 Q3 2011 Q4 2012 Q1 2012 Q2 2012 Q3 47 2012 Q4 2013 Q1 2013 Q2 2013 Q3 2013 Q4 2014 Q1 2014 Q2 y = 291.62x - 3062.5 Examples Demonstrating ROI Improved clinical care Decreases in LOS Decrease in readmission rates Decreased unnecessary test utilization Millions in savings across several disease processes Reducing waste by systematizing reporting EDW reports cost 70% less to build Clinical operations tools allow global views for increased operational efficiency 48 Organizational direction for data Improved outcomes for our patients and our enterprise Organizational evolution over time Decision support Data analytics Data reporting -EMR clinical reports -Financial reports -Shortening event to reporting time -Transforming data and translating to action -Integrating best evidence into delivery system infrastructures -EMR based recommendations and alerts -Integrated plans of care across continuums Predictive analytics --Linking likelihood of outcomes to care decisions driven with realtime data -Predicting financial outcomes and linking to clinical decisions for populations of patients -Linking outcomes across infrastructures Predictive analytics: High risk asthma Targets: reduce ED visits, hospitalization, albuterol overuse, ICS non adherence Critical data source: TCHP, TDSHS data SHORT ACTING BETA AGONISTS Targets: reduce ED visits/ unscheduled PCP visits Critical data source: TCH ED, PCP Age 1-5 , 4 of 5 below 1 hospitalization = 1 point >= 2 hospitalizations = 4 points Government insurance (Medicaid or CHIP): Q2 under health insurance information Financial barrier to meds :Answered Yes to Q4 under health insurance information Previous asthma hospitalization: Yes to Q2 under past history of asthma care Chronic Severity= Mild persistent Acute Severity= Mild NUMBER PRESCRIBING PROVIDERS Age 6+ 6 to 9 SABA = 1 point ≥ 10 SABA = 2 points EC UTILIZATION 1-2 ER = 1 point > 2 ER = 2 points HOSPITALIZATION >= 3 different prescribing providers in 12 months one of above criteria met, add 1 point PRIMARY CARE VISITS Last PCP visit > 6 months + one of above criteria met = add 1 point INHALED CORTICOSTERIOD >= 6 ICS low dose canister equivalent refills, subtract 1 point Lieu TA et al Am J Respir Crit Care Med. 1998 Apr;157(4 Pt 1):1173-80 Farber HJ, et al. Ann Allergy Asthma Immunol. 2004 Mar;92(3):319-28. Farber HJ. J Asthma. 1998;35(1):95-9 Spitzer WO, et al. N Engl J Med 1992 Feb 20;326(8):501-6 Suissa S, et al. Thorax. 2002 Oct;57(10):880-4. All 3 of the following Government insurance (Medicaid or CHIP): Q2 under health insurance information Chronic Severity= Mild persistent Acute Severity= Mild Or All 3 of the following Government insurance (Medicaid or CHIP): Q2 under health insurance information Exercise induced asthma: Answered yes to exercise page 3 of TEDAS. Acute Severity= Mild Care Process Teams Diabetes Pregnancy Asthma Transplant Pneumonia Appendicitis Newborn Hospital Acquired Conditions Sepsis and septic shock Obesity Transitions of care Survey explorer Additionally, completed a gap strategy for 38 “registries” Content System Using and innovating best practices Assuring an excellent patient experience Evidence Integrated practice via guidelines, order sets and measures Measurement System QI education and culture change Improved Population Health Deployment strategy— Care Process Teams Data/predictive analytics: measuring through meaningful metrics Deployment System Knowledge management for population health Analytic Insights Questions & Answers A Session Feedback Survey 1. On a scale of 1-5, how satisfied were you overall with the Penny Wheeler, MD / Allina session? 2. What feedback or suggestions do you have for Penny Wheeler, MD / Allina session? 3. On a scale of 1-5, how satisfied were you overall with the Charles Macias / TCH session? 4. What feedback or suggestions do you have for the Charles Macias / TCH session? 54