Allergy.
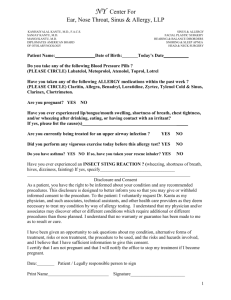
advertisement

Washington State NAPNAP 2013 Spring Conference Food Allergy Cases March 11, 2013 David R. Naimi, DO Clinical Assistant Professor of Pediatrics University of Washington School of Medicine Northwest Asthma & Allergy Center Introduction • Undergraduate – Go Dawgs! • Medical School – (Pomona, CA) • Pediatric Residency – Case Western - Rainbow Babies & Children’s • Allergy/Immunology Fellowship – CHOP & U Penn Seattle Redmond Red Ridge Issaquah Renton Everett Mt. Vernon Yakima Richland Learning Objectives • Understand the clinical manifestations of food allergic disorders • Appreciate the utility of tests used to diagnose food allergy • Understand when to refer to an allergist and how to follow patients with food allergy • Appreciate and respond to the educational needs of patients diagnosed with food allergy in regard to avoidance and treatment Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction Food Allergy Definitions • Adverse food reactions – any untoward reaction to food or food additive – Food allergy/hypersensitivity – adverse food reaction due to an immunologic mechanism • Example: Peanut allergy – Food intolerance – adverse reaction due to a physiologic or non-immunologic mechanism • Lactose intolerance • Caffeine Differences between IgE & Non-IgE food reactions IgE mediated allergy Symptoms Timing of symptoms Examples Non-IgE mediated Skin, respiratory tract, GI GI tract and/or skin, other tract, Cardiovascular Rapid (seconds to minutes). Rarely past 2hrs. Reproducible. Peanut anaphylaxis Subacute, chronic (>2hrs to days) -Celiac disease -Milk-protein induced proctocolitis -FPIES (Food Protein Induced Enterocolitis Syndrome) Mixed IgE/non-IgE: Eosinophilic Esophagitis & Atopic Dermatitis Spectrum of Immune mediated Food Allergy IgE-Mediated Mixed Non-IgE-Mediated Skin - Urticaria - Atopic Dermatitis - Angioedema Respiratory (isolated symptoms rare) - Asthma Rhinitis - Dermatitis herpetiformis Histamine related symptoms??? Gastrointestinal - GI “Anaphylaxis” - Oral Allergy syndrome Systemic - Eosinophilic gastrointestinal disorders(EoE) -Anaphylaxis -Food-associated or exercise-induced anaphylaxis - Celiac disease - Infant gastrointestinal disorders Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction The infant with “mucousy” or blood streaked stools • 2mo exclusively breastfed infant • Mucousy stools w/occasional streaks of blood noted recently • Clinical history NOT consistent w/constipation. • Normal growth & feeding pattern. • Normal exam (no rectal fissures). Questions to ask yourself • Diagnoses? Food protein induced proctocolitis. Major cause of colitis <12mo. >50% of infants usually exclusively breastfed • IgE or non-IgE mediated? Non-IgE • Risk of anaphylaxis? No • What is the most common cause? Cow’s Milk, often Soy • Skin or blood testing needed? No • What to advise parent? Mother to trial off of Cow’s milk/dairy +/- Soy • Is this going to improve? Yes. Usually resolves by 9-12mo What if this patient were bottle fed? • Change to hydrolyzed formula (Alimentum, Neutramigen, etc…) • Consider elemental formula (Elecare, Neocate) but NOT likely needed • Consider Soy formula (however, high likelihood of problems with soy) – Consider soy as an alternative nutrient AFTER age 6mo per European Society for Pediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) Recommendations Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction 12yo with oral itching with almond, fresh fruits & veggies • Began 1-2 yrs ago • Occurs w/fresh apple, pitted fruits, melons, & fresh carrot • Same symptoms w/almond • No problems w/cooked fruits & veggies • No other symptoms (no hives, respiratory symptoms, etc). Oral Allergy Syndrome (aka Pollen Food syndrome) • Oral itching w/certain foods (mild lip angioedema possible) – Contact reaction in oropharyngeal mucosa • IgE mediated • • • • – Onset <5min Raw fruits/veggies and some nuts Heat Labile proteins (cooked foods well-tolerated) Affects ~50% of adults w/allergic rhinitis Rarely causes serious symptoms (<1% risk of anaphylaxis) – possible increased risk w/tree nut & peanut Oral Allergy Syndrome (aka Pollen Food syndrome) • Cross-reactive allergens – BIRCH: apple, peach, apricot, cherry, and plum, pear, almond, hazelnut, carrot, celery, parsley, caraway, fennel, coriander, aniseed, – GRASS: Melon, Tomato, Orange, Lettuce, peanut – *RAGWEED: cantaloupe, honeydew, watermelon, zucchini, cucumber, banana *There is NO RAGWEED in the Pacific NW How to alleviate oral allergy syndrome • • • • • Cook/heat food (20sec in microwave) Avoid ripe fruits Peel & wash PO antihistamine few hrs before ingestion Allergy immunotherapy (allergy shots) Food Allergens Type Class I Class II Description Water soluble glycoproteins Plant-derived Examples Wheat, Egg, Milk, Peanut Apple, Carrot, Celery Characteristics Resistant to heat, acid, and proteases Highly heat labile. Cooking reduces allergenicity. Susceptible to digestion Sensitization GI tract Respiratory tract w/crossreactive pollens Clinical reaction Anaphylaxis, eczema Oral allergy syndrome Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction The infant w/eczema • 4mo infant w/eczema - present since he was “weeks” old – involving most areas of body. • Birth & developmental hx normal. Growing & feeding well w/out history of recurrent infections or chronic diarrhea. • Exclusively breastfed – mother asking if FOOD ALLERGIES are playing a role in eczema certain foods she ingests possibly flares his skin (? dairy) The infant w/eczema • Eczema only partially improved w/1% hydrocortisone regularly • Physical exam: – significant for scattered dry & minimally erythematous patches – few excoriations on cheeks, trunk, & extremities. What is the relationship between eczema and food allergy? They CAN be associated … extent of this association is controversial • Potential causes of eczema – Young children (<5yo) Food allergy +/- Env allergens – Older children & Adults Env allergens • Rate of sensitization to foods ranges from 30-80% (varies upon population represented) – However … ACTUAL rate of confirmed food allergy is LOWER The relationship between eczema and food allergy • Ingestion of food flare of patient's eczema (increased itching and redness). – IgE: min to hrs after ingestion – Non-IgE: hrs to days after ingestion • If the child eats a food regularly, then he/she may have persistent symptoms of eczema IgE Mediated Food Allergy • Allergies to various seeds (e.g. sesame) seem to be increasing. • Wheat, egg, and milk sensitization more commonly associated w/ eczema in children. WEMPSS = Wheat, Egg, Milk, Peanut/Treenut, Soy, Seafood (90% of food allergy) Most likely severity = peanut, treenut, seeds, seafood. Children Wheat Egg Milk Peanut Tree nuts Soy Finned fish Shellfish Adults Peanut Tree nuts Finned fish Shellfish Raw fruits/veggies (oral allergy syndrome) The modern diet “Exotic foods” – Increased reported allergic reactions • • • • Kiwi Mango Papaya Seeds (sesame, poppy, mustard) Too young for testing? • Foods – No ‘cut-off’ age for skin or blood testing to foods – If an infant/child has NEVER been exposed to a food (inutero, breastmilk, etc) then sensitization may not be present • Environmental allergens – <2yo: unlikely to be sensitized to allergens outside home – Testing to indoor allergens is still appropriate for <2yo – However, for environmental allergens: skin testing & blood testing (allergen specific IgE) can LAG behind clinical symptoms Testing: What would I do in this case? • Skin testing - Foods – Wheat, Egg, Milk, Peanut, Soy – Few other foods very common in mother’s diet (ie corn, seafood) – Fruits/veggies not likely common causes • Skin testing – Environmental allergens – Dust mites – Pets (if applicable) • If blood testing ordered (food specific IgE): would also obtain a total IgE What NOT to do when testing for food allergy • Skin/blood testing should NOT replace taking a hx • Do NOT blindly order “food allergy panels” (This is likely to yield clinically irrelevant results & FALSE food allergy dx) – Problem: some labs charge less for “panels.” A possible exception to the above statement … • Younger children w/recalcitrant eczema – Obtaining a history of food association may be difficult – One of the FEW times I consider “screening” for food allergy. More appropriate for children <5yo Skin Testing or Blood Testing? Food Allergy Testing: Identifying the presence of allergen specific IgE Skin Prick Testing Food Specific IgE (ie immunocap or radioallergosorbent tests) Cost effective More expensive Quick (results in 15min) Wait days for lab results Generally less painful More painful Affected by po antihistamines NOT affected by po antihistamines Difficult to perform if skin area is flared or if dermatographic. Limited by space. Not affected by active dermatitis nor dermatographia Generally avoid in pregnancy (despite its relative safety) Preferred during pregnancy Generally more helpful for determining the absence of sensitization (>95% negative predictive value) Generally more helpful for determining the likelihood of a clinical reaction (positive predictive value) High sensitivity (90%) esp fresh foods Sensitivity varies among different foods Moderate specificity (50-95%: depending on food & patient’s clinical history) Moderate specificity Skin testing: Epicutaneous Skin testing - Interpretation Measurements of wheal & flare, use histamine/saline controls Prick test: >3mm wheal w/10mm flare Read @ 15 min Oral antihistamines, not steroids, produce false (-) tests and alter the results of skin testing “Other” antihistamines = Ranitidine, Famotidine, Tricyclic antidepressants Results of testing in this case • Egg & Milk IgE quite elevated – Egg = 7 kU/L (normal <0.35) – Milk = 10 kU/L (normal <0.35) • Food specific IgE negative (<0.35 kU/L) for all other allergens • Total IgE minimally elevated Sampson HA. Food and Drug Reactions and Anaphylaxis: Utility of food-specific IgE concentrations in predicting symptomatic food allergy. J Allergy Clin Immunol 2001; 107(5): 891-896. Diagnostic Decision Points for Food Specific IgE Food Cow’s Milk Egg White Peanut Tree nut Fish Serum IgE (kU/L) ~95% Fail ~50% Fail 15 2 5 (if less than 2yo) 7 2 2 (if less than 2yo) 14 2 (Hx +) 5 (Hx -) 15 --20 --- Sampson HA. J Allergy Clin Immunol 2001; 107(5): 891-896. What do you do w/the results? • Demonstration of sensitization (via skin or blood test) to a food does NOT mean that the patient has clinical reactivity to that food (+) Test ≠ Clinical Relevance Food Allergy Diagnoses • Clinical reactivity can be confirmed by oral food challenges OR food elimination diets. • Double-blind, placebo-controlled food challenge (DBPCFC) – “gold standard” … but not practical. • Open food challenges performed more often in the allergy clinic – more practical. What next? • Maternal elimination of egg & milk from diet. Up to 2 wks is often enough time to determine improvement of eczema. • Refer to allergist, especially before introduction of solid foods – AVOID unnecessary food avoidance! This could cause increased sensitization too food. “Will my baby grow out of his allergies?” Natural history of Food Allergy Food When to expect resolution of IgE mediated allergy Wheat Resolves in 80% of patients by school age Egg Majority will outgrow by school age (~65%) Milk Majority will outgrow by school age (~80%) Peanut/ Tree nut Peanut: resolves in 20-25%, Tree nut: resolves in ~9%. Peanut: 7-10% recurrence of allergy may occur if a food challenge is passed & patient doesn’t eat the food regularly after this. Soy Generally outgrown more quickly than Egg or Milk. Often (+) if have concurrent peanut allergy [both are legumes]. Fish/Shellfish Less likely to resolve. Adult onset is more common. Limited data. Food allergies to most foods, other than fish/shellfish & peanut/treenuts, are usually outgrown Following a child w/food allergy • Food allergic children should be monitored regularly by a pediatrician & allergist. • Serial testing (skin test and/or serum IgE) usually done yearly (depending on type of food & age of patient). • If clinical history & lab testing is reassuring, then an oral food challenge can be performed in controlled setting to ensure resolution of food allergy. Following a child w/food allergy • Elevated initial food allergen specific IgE is assoc w/lower rate of resolution • Resolution of Atopic Derm may be a useful marker for onset of tolerance • Negative tests (skin or blood test) DO NOT guarantee loss of allergy. • IgE antibodies to a specific food can PERSIST even after clinical reactivity to that food has cleared. – Therefore, oral food challenges (often done by allergists in the office) can be helpful. CLINICAL HISTORY Skin Testing Food specific IgE Food Allergy Diagnoses Standard of Care for Food Allergy • Every food allergic reaction has possibility of developing into life-threatening reaction • • may depend upon how much of the food is eaten Long-standing principle = complete avoidance of even minute exposures and ready access to self-injectable epinephrine. Recent data has challenged the long-standing idea of strict avoidance, instead, attempting to incorporate small amounts of the food into the diet. Effect of Cooking & Digestion on Food Proteins M I M I L 1 K M I L L K K Processing K L 2 Children with milk (and egg) allergy MAY often tolerate baked-milk or baked-egg products M I BAKED GOODS Changing the Paradigm: from Strict Avoidance to a Limited Diet • 70% of children with egg allergy tolerate in baked goods • 75% of children with milk allergy tolerate in baked goods • Regular ingestion of these proteins is associated w/decreasing skin test size & milk/egg specific IgE • ? may result in development of tolerance What about future vaccines? Egg Allergy & Vaccines: Vaccines that contain “significant” amounts of Egg protein: • Influenza • Yellow Fever MMR IS OK!!! Egg allergy & Influenza Vaccination • Studies involve TIV, not intranasal LAIV (TIV = Trivalent Influenza Vaccine. LAIV = Live Attenuated Influenza Vaccine … “FluMist”) • Vaccine administered by provider familiar w/potential manifestations of egg allergy • Administer in setting w/emergency equip available • Observe x 30min or more • Centers for Disease Control and Prevention (CDC). Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP)--United States, 2012-13 influenza season. MMWR Morb Mortal Wkly Rep. 2012 Aug 17;61(32):613-8. • Greenhawt MJ, et al. Safe administration of the seasonal trivalent influenza vaccine to children with severe egg allergy. Ann Allergy Asthma Immunol. 2012 Dec;109(6):426-30. What should you tell the mother about the introduction of future foods for her infant? • Previous recommendations for delaying intro of solid foods for purpose of preventing allergic disease in “HIGH RISK” infants is NOT EFFECTIVE • Previous AAP recommendations = delay introduction of certain highly allergenic foods in high risk children: – cow's milk until age ……………………. 12mo – eggs until age …………………………... 24mo – peanuts, tree nuts, fish, and shellfish … 36mo What should you tell the mother about the introduction of future foods for her infant? • New recommendations: – insufficient evidence to recommend any specific practices concerning intro of foods after 4-6 mo for prevention of allergic disease in *“high risk” infants. – Breastfeeding is best for ≥4mo. If NOT breastfed, hydrolyzed formulas MIGHT be helpful in “high risk” infants to delay or prevent atopy. – DO NOT delay introduction of solid foods for “high risk” infants. This practice might increase the risk of allergy. *”High risk” definition: having at least one 1st degree relative (parent or sibling) w/documented allergic condition (mod/severe atopic dermatitis, food allergy, asthma). Greer et al. Pediatrics 2008; 121:183. What should you tell the mother about the introduction of future foods for her infant? • General guidelines for introducing solid foods to an infant's diet are also appropriate for infants at “high risk” for allergic disease. • Some reasons to REFER to an allergist: - Breastfed infant develops atopic dermatitis before solid foods are introduced or has an allergic reaction during/after breastfeeding. - Infant develops allergy to a food or shows signs of allergic disease. Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction Sarah & the Cashew cookie • Age 17 • Ate a “cashew” cookie and developed anaphylaxis treated in the emergency department • History indicates she regularly tolerates cashews, pistachio, almonds, walnuts, pecan and peanuts Which is the next most appropriate course of action? A) Advise to avoid all tree nuts B) Advise to avoid cashew C) Perform allergy tests to cashew D) Determine the ingredients of the cookie Sarah & the Cashew cookie • Age 17 • Ate a “cashew” cookie and developed anaphylaxis treated in the emergency department • History indicates she regularly tolerates cashews, pistachio, almonds, walnuts, pecan and peanuts Which is the next most appropriate course of action? A) Advise to avoid all tree nuts B) Advise to avoid cashew C) Perform allergy tests to cashew D) Determine the ingredients of the cookie Diagnosis Requires Careful History • The cookie package indicated that macadamia nuts were an ingredient • Sarah had been eating cashews but infrequently (once/twice) ate macadamia nuts • Allergy tests (+) to macadamia & negative to cashew • Instructions could include: – avoidance of all tree nut products or … – continue ingestion of tolerated nuts when certain that macadamia is not included General questions to ask a patient w/suspected food allergy • • • • • • History, History, History! What food? How much? What was the reaction? Timing of symptoms? Reproducible? Any ingestions after reaction? – Can develop allergy … (esp seafood) Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction Stephanie vs the Bagel • • • • 14 years old, has asthma Sesame allergy (known) Ate a bagel with no visible sesame Has no hives, develops repetitive coughing, hoarse throat, trouble swallowing, vomiting What treatment is most appropriate? A) Antihistamine B) Injected epinephrine C) Asthma inhaler D) Heimlich maneuver Anaphylaxis May Occur Without Hives What treatment is most appropriate? A) Antihistamine B) Injected epinephrine C) Asthma inhaler D) Heimlich maneuver Treatment of Food Allergy • Avoid offending food! If in doubt, don’t eat it! • Read food labels! • Early use of epinephrine!! • Written plan for emergencies. • Wear Medic-alert bracelet. • Ensure nutritional needs are being met. Food-induced Anaphylaxis • • • • Frequency: ~150-200 deaths/ year Food allergy #1 cause of anaphylaxis in ER Rapid onset, up to 30% biphasic Risk factors for fatal, food-induced anaphylaxis – – – – Major risk factor: delayed use of epinephrine High risk groups: teenagers/young adults High risk co-morbidity: asthma Confusing physical symptom: urticaria may be absent in up to 10% of cases Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction 15yo w/fatigue, h/a, occasional abd pain and loose stools • Questionable cause • Workup & labs normal thus far • “Dairy” and “wheat” might be the cause, but unclear • If this is food related, seems delayed (>2-3hrs) and not immediate So … is this most likely an “Intolerance” or “Allergy” ? … my neighbor recommended a food allergy/sensitivity panel … • Obtained blood test at local “allergy lab.” • (+) to various foods: grains, dairy, egg, blueberry, etc… • Blood test report = IgG testing IgG to foods • Proposed to identify nonIgE-mediated hypersensitivity to foods: IBS, migraine headaches, myalgia, fatigue, etc • Assays may measure total IgG, IgG subclasses (i.e. IgG4), or IgG/IgE combined testing. www.usbiotek.com IgG to Foods: Availability • Large scale screening for hundreds of food items by ELISA-type and RAST-type assays • USA & several European countries, ‘mainstream’ allergy diagnostic labs now offer IgG assays to foods • Direct-to-consumer advertising for panels of IgG • Direct marketing by some companies to PCPs • May not be covered by a patient’s medical insurance What I tell my patients • Food intolerance vs True allergy • Food intolerance is a TRUE entity, but there is NOT an accurate way to actually “test” for this • IgG testing is controversial and is/should be used for research purposes. What I tell my patients (cont..) • IgG is elevated to many foods in healthy individuals & is often (+) to what is common in our diet: (Wheat/Gluten, Dairy, and Egg). – Patients who note improvement w/avoidance of IgG (+) foods often DRASTICALLY change their dietary habits • If food intolerance/sensitivity is suspected: – Best way to diagnose this is avoidance of above foods/food groups for a certain duration (few/several weeks) followed by re-introduction – Consultation with dietitian if continued avoidance of foods is done (2004) - UK (2005) - UK (2006) - USA (2007) - China (2007) - China Zar et al 25 IBS (2005) – UK (13 IBS-D, 10 IBS-C, 2 alternating) IgG4 6mo elimination IgG4 antibodies to milk, eggs, wheat, beef, pork and lamb were elevated. Significant improvement reported in pain severity (pB/0.001), pain frequency (p/0.034), bloating severity (p/0.001), satisfaction with bowel habits (p/0.004) and effect of IBS on life in general (p/0.008) at 3mo & 6mo. Rectal compliance was significantly increased (p/0.011) at 6mo. Critiques To be discussed (2004) - UK Considerable overlap observed in IgG titers for certain foods between IBS and controls. IBS pts: elevated IgG4 abs to ave of 8 foods. Controls: 5 foods. No correlation seen between pattern of elevated IgG4 ab titers & patients’ symptoms. (2005) - UK No placebo group. Probiotics were also given. Potential for placebo effect was huge. Authors discuss the detection of serum IgG antigen-ab complexes, so what was actually measured is not clear. (2006) - USA (Chinese). No Placebo diet group. (2007) - China No significant correlation between symptom severity and elevated serum food antigen-specific IgG Abs. (2007) - China Zar et al 25 IBS (2005) – UK (13 IBS-D, 10 IBS-C, 2 alternating) Noantibodies placebo to diet group difficult to further IgG4 milk, eggs,(thus, wheat, beef, pork and lamb were ele IgG4 interpret these data, b/c potential for placebo effect). pain Significant improvement reported in pain severity (pB/0.001), 6mo elimination Data at 6mo only available on 15 patients. Patients frequency (p/0.034), bloating severity (p/0.001), satisfaction eliminated average of 8 foods (most common being with b habits (p/0.004) andin effect of IBS diet) on lifeincluding in generalmilk, (p/0.008) at 3m foods common a Western & 6mo. compliance significantly increased (p/0.011) a eggs,Rectal beef, pork, wheatwas & tomatoes Results of studies of IgG antibody elimination diets for migraine headaches Author Subjec ts Trial Results Alpay K, et al 30 migraine Double blinded randomized controlled cross-over trial 6wk elimination Average count of reactions with abnormally high titer was 24±11 against 266 foods. Compared to baseline, there was statistically significant reduction in # of headache days (from 10.54.4 to 7.53.7; P<0.001) and # of migraine attacks (from 9.04.4 to 6.23.8; P<0.001) in the elimination diet period. true diet (n = 84) sham diet (n = 83) Single blind two arm Randomized controlled trial. true diet vs sham diet 12wk elimination Elimination diet Small decrease in # of migraine like headaches over 12 wks, although this difference was not statistically significant (IRR 1.15 95% CI 0.94 to 1.41, p = 0.18). At 4 wks, use of the ELISA test with diet elimination advice significantly reduced # of migraine like headaches (IRR 1.23 95%CI 1.01 to 1.50, p = 0.04). Disability and impact on daily life of migraines were not significantly different between the true & sham diet groups. Statistically significant differences in the number of positives for IgG food allergens between patients with migraine and a controlled group. Elimination diets successfully control the migraine without the need of medications. Cephalalgia 2010 Turkey Mitchell N, et al Nutrition Journal 2011 UK Arroyave H, et al Revista Alergia Mex 2007 Mexico 56 migraine 56 controls Results of studies of IgG antibody elimination diets for migraine headaches Author Alpay K, et al Cephalalgia 2010 Turkey Mitchell N, et al Nutrition Journal 2011 UK Subjec ts 30 migraine Double blinded randomized controlled cross-over trial 6wk elimination true diet Single blind two arm (n = 84) sham diet Randomized controlled trial. (n = 83) true diet vs sham diet 12wk elimination 56 Arroyave H, et al migraine Revista Alergia Mex 56 2007 controls Mexico Trial Elimination diet Critiques Low number of patients Relatively short follow-up Potential carry-over effect of a cross-over design Recruited participants who self-reported their migraines (their headaches may not have been from migraines) Small decrease in # of migraine like headaches over 12 wks, although this difference was not statistically significant (due to diet adherence?) Disability and impact on daily life of migraines were not significantly different between the true & sham diet groups. No Placebo group Not blinded • Double blind, randomized, controlled, parallel design • 150 outpatients w/IBS randomized to receive, for 3mo, either a “true diet” excluding all foods to which they had raised IgG antibodies (ELISA) or a “sham diet” excluding the same number of foods but NOT those to which they had antibodies. • Primary outcome measures = change in IBS symptom severity & global rating scores. Secondary outcome measures = Noncolonic symptomatology, QOL, and anxiety/depression. Baseline demographic/clinical characteristics of the two groups, including the use of concomitant medication, were found to be similar with the exception of IBS symptom severity score which was slightly higher in the treatment group. 30% of patients found to be atopic. • Obtained IgG abs specific to 29 different food antigens. • Most patients found to be (+) to 6–7 foods (range 1– 19). • Sham diet eliminated same # of foods but not those particular foods in the True diet. • Adherence was lower in those on the true diet (24 patients withdrew from the study in the true diet group mainly b/c of difficulty in following the diet) Atkinson W, et al. Gut. 2004. Results: Atkinson W, et al. Gut. 2004 Discussion (Atkinson W, et al. Gut. 2004.) • Content of food elimination diets in true & sham groups were NOT similar. Dietary restrictions in one group are NOT controlled for by the other group. – Treatment group excluded significantly different foods to the control group, particularly those foods which appear to exacerbate symptoms of IBS. – ‘‘True diet’’: 84% avoided milk products, 49% avoided wheat (both foods are known to be common offenders in IBS). Total number of foods avoided by this group = 498. – ‘‘Sham diet’’: 1.3% avoided milk, 8% avoided wheat. Total number of foods avoided = 453. – These differences between the diets could explain the modest difference in outcome between the two diet groups. – More care needs to be taken to match diets not just for number of food types excluded but also for types of food. Discussion (Atkinson W, et al. Gut. 2004.) • Effectiveness of blinding is questionable. • Does the test add specificity? – Would patients w/IBS gain as much symptomatic improvement if recommended to exclude the top four foods (yeast, milk, whole egg, and wheat) compared with an IgG antibody test based diet? • 86.7% in treatment group avoided yeast. – ‘‘Yeast exclusion’’ diet is not a recognized diet in standard textbooks of diet & nutrition. This diet may sometimes entail exclusion of a VERY wide range of foods (i.e. bakery products, alcoholic beverages, commercial fruit juices, cereals, condiments, dairy produce, fungi, meat products, canned food, dried fruit, etc). Discussion (Atkinson W, et al. Gut. 2004.) “Despite the inconclusive results of this study, it has regrettably already been the subject of a press release and other publicity by the company that provided the IgG testing for this study, in order to promote IgG tests to the general public. On the company’s website, IgG testing is now described as ‘‘clinically proven’’ by the British Allergy Foundation on the basis of this study (The UK YorkTest website: www.yorktest.com). This blurring of the boundaries between what should be a disinterested scientific enquiry and the promotion of a commercial venture is regrettable.” ~Dr J O Hunter Addenbrookes Hospital Cambridge, UK Conclusions from the IBS studies IBS • May indeed be true, proven benefits from dietary change • Trials that appropriately blind interventions in irritable bowel syndrome are difficult to design and implement. • IgG to the food may reflect foods commonly consumed rather than those contributing to symptoms. • There may be other food specific immune effects, immune dysregulation, peptide effects or effects of dietary components on gut microflora composition, irrespective of IgG values. What we do know: IgG4 & the Development of Clinical Tolerance in OIT and SLIT Trials Keet CA, et al. The safety and efficacy of sublingual and oral immunotherapy for milk allergy. JACI. 2011 Nov 28. • 30 subjects with CM allergy. After therapy, 1 of 10 subjects in the SLIT group, 6 of 10 subjects in the SLIT/OITB group, and 8 of 10 subjects in the OITA group passed the 8-g challenge (P = .002, SLIT vs OIT). • By the end of therapy, titrated CM skin prick test results and CD63 and CD203c expression decreased and CM-specific IgG(4) levels increased in all groups, whereas CM-specific IgE and spontaneous histamine release values decreased in only the OIT group. What we do know: IgG4 & the Development of Clinical Tolerance in OIT and SLIT Trials Enrique E, et al. Sublingual immunotherapy for hazelnut food allergy: a randomized, double-blind, placebo-controlled study with a standardized hazelnut extract. JACI. 2005; 116:107–109. • SLIT w/hazelnut. 23 patients, half randomized to active treatment and half to placebo. 50% of those on active treatment were able to tolerate 20 g of hazelnut at the end of the trial and showed increases in hazelnut-specfic IgG4. Buchanan AD, et al. Egg oral immunotherapy in nonanaphylactic children with egg allergy. JACI. 2007; 119:199–205 • Egg oral immunotherapy in seven children with IgE-mediated egg allergy, all of whom improved during the course of the study. Two were able to reach a state of complete oral tolerance. Hen’s eggspecific IgG rose significantly in these subjects, IgE did not. What we also know: IgG is increased in healthy controls Stapel SO, et al. Testing for IgG4 against foods is not recommended as a diagnostic tool: EAACI task force report. Allergy. 2008; 63:793–6. • 13 healthy lab workers. IgG4 and IgE obtained to specific foods • Positive results for IgG4 against different foods found in all samples, and did not significantly coincide with positive IgE. • Increased IgG4 results were, in none of the subjects, related to clinical problems by intake of foods • “Positive IgG4 tests to foods therefore do not indicate the presence of food allergy, but are probably reflecting prolonged exposure to food components.” (+) IgG … then what? • Some companies construct a ‘rotary diet’ for the patient to follow at home, though most laboratories do not get involved in the practice of medicine in this way. • Such dietary prescriptions can be hard to follow & may cause nutritional deficiencies especially in children With ANY type of testing…. • Allergy tests (SPT, serum IgE, patch testing, etc) MUST be interpreted in the context of the patient's specific clinical history, and the diagnosis of an allergic disorder CANNOT be based solely on a laboratory result. • Food Allergy: Accurate diagnoses VERY important - to prevent unnecessary avoidance of foods & potentially harmful diets Portnoy JM. Mo Med. 2011 Testing in General: Can be a “Dangerous Weapon” • All Physicians must educate themselves & their patients about the clinical utility of ANY test. • The “Danger” = misdiagnoses, unnecessary specialist consults, wasted time and $$$. • Panels for food allergy may be seen by some patients & physicians as a substitute for a thorough history & physical exam • Nonselective use of large panels of allergens can lead to false positives and misinterpretation of the results, particularly in food allergy We need to utilize our testing wisely & responsibly It Can be Frustrating nightshadejournal.com yankeegunnuts.com Many patients w/suspected food intolerance/sensitivity are disappointed by the negative results of IgE testing … they often look elsewhere for testing that might be “more in line” with their expectations. Stapel et al. Allergy. 2008. What NOT to Say You don’t have a food allergy…Don’t do ANYTHING. That testing is hogwash. I have a food allergy… Look at these IgG test results! What should I do? www.onpublicspeaking.com A More Appropriate Response Ok … lets talk about your symptoms & why you think they’re food related … … then lets discuss what these IgG results mean & what we know about IgG testing … www.onpublicspeaking.com Final Thoughts • Have an open mind & healthy skepticism • IgG to foods needs further research. – Too early to encourage patients or insurers to spend $$ on panels that are suited for research, not clinical, applications – IgG4 could be a sign of clinical tolerance, normal response to food, or prolonged food exposure. – IgG4 elevated in IBS, migraines, and inflammation??? • IgG to foods is “NOT ready for prime time.” Stapel et al. Allergy. 2008. Teuber & Beyer. Curr Opin Allergy & Clin Imm. 2007 Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction 12yo with allergy to salmon • 2 ingestions • Both ingestions reaction = skin pruritis, few hives on abdomen resolved with benadryl • Parents do NOT have Epi Pen … “he only gets a few hives and it goes away with Benadryl…” Food Allergy Myth: Prior Episodes Predict Future Reactions • No predictable pattern • Severity depends upon: – Sensitivity of the individual – Dose of the allergen – Other factors (food matrix, exercise, concurrent medications, airway hyper-responsiveness, etc) • Must always be prepared for emergency Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction 3yo w/hives after peanut ingestion • Occurred immediately (within 15min) after ingesting ½ tsp of peanut butter. • One episode of emesis 20min after ingestion • No prior peanut or peanut butter ingestions • He has not had peanut since Results of testing • Your colleague sent off a PANEL of food allergy tests • Blood testing results: – Peanut: elevated (>50 kU/L) – Also (+) SOY & slightly to blueberry & carrot. • Why is soy (+)? Soy is also a legume • Why are Blueberry and Carrot elevated? Who knows … (carrot = pollen cross reactivity) Sicherer S. J Allergy Clin Immunol 2001; 108:881 Cross-reactivity Between Foods Mother asks: “how SEVERE is his peanut allergy?” Serum IgE LEVEL or skin prick test SIZE is NOT a predictor of severity but rather the likelihood of a reaction. Diagnostic Decision Points for Food Specific IgE Food Cow’s Milk Egg White Peanut Tree nut Fish Serum IgE (kU/L) ~95% Fail ~50% fail 15 2 5 (if less than 2yo) 7 2 2 (if less than 2yo) 14 2 (Hx +) 5 (Hx -) 15 --20 --- What to tell family (+ tests to peanut, soy, carrot, blueberry) • Do NOT eat anymore peanut? Yes (do NOT) • Stop eating soy? Peanut is a LEGUME. Most (>90%) of legumes are actually tolerated by those with peanut allergy, even though about 50% show a (+) IgE via serum or skin test to other legumes. • What question to ask: has he eaten soy, blueberry, or carrot in the past and since this reaction? – He has eaten ALL of these since this peanut ingestion without problems (even tofu) – Soy lecithin or small amounts of soybean oil do NOT count as significant soy ingestion CURVE BALL: What if the testing to peanut was negative in THIS case? • Ok to eat peanut? • Repeat peanut testing? When to repeat? • Skin testing? Fresh food skin testing? Negative tests (skin or blood test) DO NOT guarantee lack of allergy, especially if clinical history suggests allergy CLINICAL HISTORY Skin Testing Food specific IgE Food Allergy Diagnoses PEANUT allergy factoids • • • • • Not a true “nut”; member of legume family. 1.5 million Americans have peanut allergy. 95% of peanut allergic patients may eat legumes. 15-20% of children may outgrow peanut allergy. Cold-pressed peanut oil – contains protein More Peanut Allergy Factoids • If a child has peanut allergy, their sibling has a 7% chance of having peanut allergy. Siblings should be tested before peanut allergy is introduced. • Although peanut and Tree nut do NOT cross-react, about 25-50% of those with peanut allergy also have tree nut allergy. • Reactions to peanut allergy usually occur with ~1 kernel of peanut. Reactions can occur with trace amounts (0.1-10mg). • Prevalence of peanut allergy has doubled in the past decade (current prevalence is ~1%) Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 55yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction Crustacean Allergy • 21 y/o w/anaphylaxis to shrimp at ages 5yo and 16yo. • Doctors told his family he was allergic to iodine in seafood • Has been avoiding seafood. • Food specific IgE (i.e. RAST) to shrimp >100; Skin test 12/35 w/f IgE towards Protein in Food NOT Iodine Crustacean Allergy A Medical Myth Exposed Question: Does this patient have to worry about iodine or radiocontrast? Answer: NO. There is no relationship between shellfish allergy and allergy to contrast Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction 2yo old with facial rash • Child presents w/occasional erythema on her face w/various foods, but unable to pinpoint which foods. • She is otherwise well without other symptoms after food ingestion • PMHx/Birth Hx uneventful except for a h/o forcepts delivery Diagnoses? Auriculotemporal syndrome (Frey’s syndrome): • Non-Immune Mediated Adverse Food Reaction • A masquerader of food allergy • Transient uni or bilateral facial flushing or sweating following ingestion of spicy or flavorful foods. • Infants/children w/history of forceps delivery & damage to auriculotemporal nerve. Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction 17yo who couldn’t swallow his pill • Took an allergy pill but “didn’t go all the way down.” • Presented the to ER Allegra D Next step… • History of prior dysphagia, but this was first time needing ED visit • Placed on Prevacid • Despite good adherence on Prevacid for several weeks still w/intermittent symptoms of dysphagia • Scheduled for endoscopy & biopsy Endoscopic findings • Endoscopy 60 eosinophils/hpf in esophagus Gastrointestinal Eosinophils Normal values, per 400x microscopic field: • • • • Duodenum (20) Colon (10-20) Gastric antrum (10) Esophagus (0) > 98% reported Eosinophilic Gastroenteritis (EG) cases involve antrum and/or duodenum Eosinophils in the Esophagus • Reflux? – Biopsy done while on PPI trial (at least 2mo) – Less likely to see >20 eos/hpf in GERD • Diagnoses = Eosinophilic Esophagitis (EoE) Eosinophilic Esophagitis Endoscopic findings in EoE Biopsy is KEY to diagnoses Normal (32%) Furrows (41%) Rings (12%) White plaques (15%) Eosinophilic Esophagitis - Histology Superficial Layering Severe Eosinophilia Eosinophilic Microabscess Definition of EoE • Persistent symptoms on a PPI (adherent to therapy) • Endoscopy is performed 4-8wks after initiation of PPI, and biopsy reveals >15 eos/hpf in esophagus • Approximately 5 to 10% of pediatric patients and 6% of adult patients with poorly controlled GERD are thought to have EE • Chronic condition Clinical presentation • Clinical presentation varies per age – Infants/younger children • Feeding dysfunction, vomiting, abdominal pain, FTT – Adolescents & adults • Dysphagia, food impaction, chest pain, GERD symptoms (refractory). Eosinophilic esophagitis • Gastroesophageal Reflux – Heartburn more likely Dysphagia more likely – pH probe pH probe • Abnormal • Normal – Acid blockade Acid blockade • Responsive • Generally Unresponsive – 1-5 eos/HPF >15 eos/HPF • Eosinophilic Esophagitis – – – – – Male > Female – Esophageal morphological abnormalities (such as rings, furrows, or exudates) Differential diagnosis • • • • • GERD Eosinophilic gastroenteritis Crohn’s disease; inflammatory bowel disease Medications Infection – Viral – Candidal – Parasitic • Hypereosinophilic syndrome Spectrum of Immune mediated Food Allergy IgE-Mediated Mixed Non-IgE-Mediated Skin - Urticaria - Atopic Dermatitis - Angioedema Respiratory (isolated symptoms rare) - Asthma Rhinitis - Dermatitis herpetiformis Histamine related symptoms??? Gastrointestinal - GI “Anaphylaxis” - Oral Allergy syndrome Systemic - Eosinophilic gastrointestinal disorders(EoE) -Anaphylaxis -Food-associated or exercise-induced anaphylaxis - Celiac disease - Infant gastrointestinal disorders EoE and atopy • Strong association of EoE w/allergies • Allergy testing may help w/management of concomitant atopic disease Food allergy in EoE: IgE and non-IgE mechanism • Children w/EoE – Food likely a factor in many children w/EoE. Information gained from allergy testing may help guide therapy. – Often improve on elemental diet • Adults w/EoE – Less likely food allergy – Dietary therapy sometimes used in motivated adults. • How do we determine which food? – Skin prick testing (IgE mediated) – Patch testing (non-IgE mediated) – Food elimination • Most common foods (milk, wheat, egg, soy) Example of Patch Testing Treatment • Why treat? – Strictures – Hiatal hernia – No evidence of increased cancer risk • Therapeutic options – – – – – – Dietary avoidance Medications (po steroids, topical “swallowed” steroids) PPIs Montelukast (questionable benefit) Anti-IL5 (experimental) Dilation (strictures) Take home message • Eosinophilic esophagitis should be considered in … • Adolescent & adults with: – history of food impaction – persistent dysphagia – GERD that fails to respond to medical therapy • Children with: – Recurrent vomiting, abdominal pain, refractory GERD Cases • • • • • • • • • • • • Infant w/“mucousy”/blood streaked stools Teenager with oral itching to certain foods Infant with eczema Sarah and the Cashew Cookie Stephanie vs the Bagel 15yo w/fatigue, h/a, occasional abd pain and loose stools 12yo w/salmon allergy 3yo w/hives after peanut ingestion Crustacean allergy 2yo w/facial rash after food ingestion 17yo who couldn’t swallow his pill Infant w/delayed vomiting after solid food introduction Infant w/delayed vomiting after solid food introduction • Baby J: 20 wk old, former FT infant, exclusively breast-fed • 16 wks small amts rice cereal tolerated • 17 wks few bites of apple introduced • 18 wks larger amts rice cereal & apples – 1.5-2h later: nonbilious emesis (2hrs dry-heaving) – Limp, brought to ED – Admitted: heme (+) stools, normal head CT, KUB & barium enema – Diagnosed w/apple allergy & EpiPen prescribed Additional history… • Next few days, he did well exclusively breast-fed • Day before admission, he was given a spoonful of rice cereal. 2hrs later developed emesis (nonbilious, repetitive). • In ED, limp and ill-appearing. • Afebrile, HR 157 bpm, BP 63/45. • Treatment: subcutaneous epinephrine without improvement and IVF • Negative sepsis workup; determined to have…? Spectrum of Immune mediated Food Allergy IgE-Mediated Mixed Non-IgE-Mediated Skin - Urticaria - Atopic Dermatitis - Angioedema Respiratory (isolated symptoms rare) - Asthma Rhinitis - Dermatitis herpetiformis Histamine related symptoms??? Gastrointestinal - GI “Anaphylaxis” - Oral Allergy syndrome Systemic - Eosinophilic gastrointestinal disorders(EoE) -Anaphylaxis -Food-associated or exercise-induced anaphylaxis - Celiac disease - Infant gastrointestinal disorders FPIES: Food Protein Induced Enterocolitis Syndrome • Onset: early infancy • Most common triggers milk & soy • Other foods: grains (rice, oats, barley), meat & poultry, certain veggies & fruit (sweet potato, squash, string beans, banana), legumes (peas, lentils), seafood. • Rice-induced FPIES more likely to have severe symptoms • Reactions to breast milk reported (less likely) Clinical features of FPIES • • • • Vomiting (~2hrs post ingestion) Diarrhea (~5hrs post ingestion) Lethargy Dehydration that may progress to: – Acidemia – Hypotension – Methemoglobinemia Labs and Biopsy Findings in FPIES Laboratory Findings • Possible elevated PMNs, eosinophilia, and thrombocytosis occurring w/in several hrs after ingestion Biopsy Findings • Colonic biopsies – crypt abscesses, diffuse inflammatory cell infiltrate with prominent plasma cells • Small bowel biopsies – acute inflammation, edema, and mild villous injury • Focal erosive gastritis & esophagitis w/eosinophilia also described Allergy evaluation • NON-IgE mediated – Negative IgE testing (skin or blood test) – Possible role for patch testing (experimental) Treatment of acute reaction • Intravenous fluid boluses • Supportive care • Epinephrine, antihistamines, and oral steroids traditionally do NOT help Definitions to know • Food protein colitis • FPIES – Common – Rare – Milk, Soy – Often breastfed infants – Healthy infants who present with blood or mucus in stool – Symptoms subside after removal of causative protein – Resolves by 12mo – Milk, Soy, grains, etc… – Rare if exclusively breastfed – Severe & protracted vomiting, dehydration, lethargy and shock few hrs after ingestion – Symptoms subside after removal of causative protein – Resolves by 1-3yrs of age Management of FPIES • Avoid suspected food • Can usually continue breastfeeding (maternal avoidance of offending food) • Formula-fed & reacted to milk/soy: – Sub hydrolyzed or preferably amino acid formula • Caution with hydrolyzed formulas – consider medical supervision w/first ingestion – Do NOT sub cow’s milk formula for soy (or vice versa) … 50% infants may react to both. FPIES: prognosis • Usually able to tolerate offending food by 1-3yrs of age • Recommend challenge under medical supervision if food re-introduced – IV access in patients w/history severe reactions Resources • Food Allergy & Anaphylaxis Network – www.foodallergy.org • American Academy of Allergy, Asthma, and Immunology – www.aaaai.org • American College of Allergy, Asthma, and Immunology – www.acaai.org • APFED (American Partnership for Eosinophilic Disorders – www.apfed.org • The FPIES Foundation – www.fpiesfoundation.org • Center for Food Safety and Applied Nutrition – www.cfsan.fda.gov • US Food and Drug Administration Medwatch – www.fda.gov/medwatch The End dnaimi@nwasthma.com References • Sicherer, SH, Teuber, S. Current approach to the diagnosis and management of adverse reactions to foods. J Allergy Clin Immunol 2004; 114:1146 • Sampson, HA, Ho, DG. Relationship between food-specific IgE concentrations and the risk of positive food challenges in children and adolescents. J Allergy Clin Immunol 1997; 100:444. • Sampson, HA. Utility of food-specific IgE concentrations in predicting symptomatic food allergy. J Allergy Clin Immunol 2001; 107:891. • Food allergy: a practice parameter. Ann Allergy Asthma Immunol 2006; 96:S1. • Greer, FR, Sicherer, SH, Burks, AW. Effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics 2008; 121:183. References • Sampson HA, Munoz-Furlong A, Campbell RL. Et al. The second symposium on the definition and management of anaphylaxis: Summary report. J Allergy Clin Immunol 2006;117:391-7. • Lieberman P, Kemp SF, Oppenheimer JJ, et al, The diagnosis and management of anaphylaxis: An updated practice parameter. J Allergy Clin Immunol 2005; 115 (3):S485-523. • Bock SA, Muñoz-Furlong A, Sampson HA. Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol 2001; 107(1):191-3. • Sampson HA, Mendelson LM, Rosen JP. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med 1992; 327:380-4. References • Cianferoni A and Spergel JM. Food allergy: Review Classification and Diagnosis. Allergology International 2009; 58: 457-466. • Sampson HA and JA Anderson. Summary and Recommendations: Classification of GI Manifestations due to Immunologic Reactions to Foods in Infants and Young Children. J Pediatr GI Nutr 2000; 30: S87-S94. • Mehr S et al. Food Protein Induced Enterocolitis Syndrome--16 year Experience. Pediatrics 2009;123:e467-472. • Liacouras CA, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011 Jul;128(1):3-20. • Sampson HA. Update on Food Allergies. JACI 2004;113: 805-819. Additional References • • • • • • Sampson HA. Update on Food Allergies. JACI 2004;113: 805-819. Cianferoni A and Spergel JM. Food allergy: Review Classification and Diagnosis. Allergology International 2009; 58: 457-466. Sampson HA and JA Anderson. Summary and Recommendations: Classification of GI Manifestations due to Immunologic Reactions to Foods in Infants and Young Children. J Pediatr GI Nutr 2000; 30: S87-S94. Nowak-Wegrzyn, et al. Food Protein Induced Enterocolitis Syndrome--caused by Solid Food Proteins. Pediatrics 2003;111:829-835. Sicherer SH. Food protein induced enterocolitis syndrome: case presentations and management lessons. JACI 2005;115:149-156. Mehr S et al. Food Protein Induced Enterocolitis Syndrome--16 year Experience. Pediatrics 2009;123:e467-472.