File - Samantha A. Redmon
advertisement

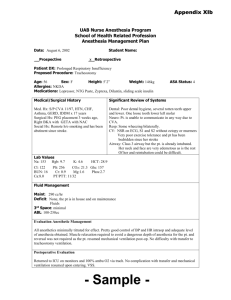
RUNNING HEADER: Medical Surgical Module Care Plan #2 Medical Surgical Clinical Care Plan #2 Samantha A. Redmon University of Arizona Medical Surgical Module Care Plan #2 2 Patient Background Date of Care: 10/16-10/17 Gender: Male Female Age Range (e.g. 60-65 yr): 50-55 Hospital Day #: 4 & 5 Advanced Directives (e.g. Living Will, Medical Durable Power of Attorney, Do Not Resuscitate or Allow Natural Death): Full Code. Allergies (Drug/Food/Environment): No known food, drug or environmental allergies. Admission diagnosis: Acute respiratory failure; vocal cord paralysis. Patient stated Chief Complaint: Worsening of SOB episodes; cough with white sputum; wheezing. Patient stated in emergency department, “it feels like something is blocking my breathing.” Briefly describe hospital course: Patient admitted to the ED on 10/12 presenting with stridor and expiratory wheezes, as well as complaints of increasing shortness of breath and hoarseness within the last 24 hours. While in the ED, patient entered acute respiratory failure and an awake tracheotomy was performed. Patient was transferred to ICU for stabilization, and transferred to current unit. Patient scheduled for arytenoidectomy on 10/17 to widen the laryngeal inlet. Previous 24 hour I & O totals: Intake of 100 mL; output of 1,675 mL; net -1,575 mL. Current Orders (exclude labs/medications/diagnostic tests): Activity: Ambulation q2h Diet: Regular IV type/site: 18 g peripheral IV, right forearm; 18 g peripheral IV, left forearm. IV fluids: N/A Others: I/O q shift; SCDs on lower legs when non-ambulatory, HOB at least 30 degrees; ROM exercises q8h; trach care q8h, humidified air (room air). Interdisciplinary Services/Consults (e.g. PT, OT, ST, dietary, hospice): Respiratory therapy Language spoken: English Religious preference: Catholic Insurance: State Medicaid program Immunization status (flu and pneumonia): Not on file. Domestic/Child/Elder abuse issues: None reported. History of illicit drug/alcohol/tobacco use: Current marijuana user (2-3 times/week for 30+ years). Medical Surgical Module Care Plan #2 3 Medical and Surgical History Medical History Brief Description of each Diagnosis Acute respiratory failure Acute respiratory failure is defined as a sudden change in the ability of the lungs to effectively exchange oxygen and/or carbon dioxide between the environments and the tissues. It is typically diagnosed with a PaO2 of less than 50 mmHg, a PaCO2 of greater than 50 mmHg, and a pH of less than 7.35. (Phipps, Monahan, Sands, Marek, & Neighbors, 2003, p. 592) Vocal cord paralysis Vocal cord paralysis occurs when infection or physical trauma causes damage to the vagus nerve or the laryngeal nerves. Vocal cord paralysis typically presents in stridor, weak or hoarse voice, and severe dyspnea. (Phipps et al., 2003, p. 494) June, 2014: Pneumonia May, 2014: Pedestrian struck Marijuana use Surgical History Tracheotomy Arytenoidectomy Lower respiratory tract infection, caused by colonization of the lung tissue by such pathogens as Pseudomonas aeruginosa, Staphylococcus aureus, Streptococcus pneumoniae and others. (Phipps et al., 2003, pp. 525-526) Patient was struck by a motor vehicle while crossing the street, sustaining the following injuries: pneumothorax, right kidney laceration, right pelvic fracture, closed TBI, right ulnar fracture, acute blood loss, and 8 or more right rib fractures. Patient may be educated about the risks of smoking and illicit drug use, including psychosocial, behavioral, economic and physiological implications. Potential interventions might include counseling, whereby the patient receives accurate education about risks and cessation measures. Since the patient cites pain relief as the main benefit of marijuana use, other, more healthful pain management alternatives such as t’ai chi’, hypnosis, guided imagery or acupuncture may be explored. (Phipps et al., 2003, pp. 13-15) Brief Description of each Surgery A tracheotomy is a surgical procedure whereby an incision is made on the anterior aspect of the throat for the purpose of accommodating a tube which is inserted directly into the trachea (Phipps et al., 2003, p. 515). In the case of this patient, an alternative airway was created to bypass the laryngeal stenosis that was obstructing his airway. Arytenoidectomy is the surgical resectioning of the arytenoid cartilage for the purpose of restoring the airway diameter of the larynx compromised by bilateral vocal cord paralysis (Phipps et al., 2003, p. 494). In the case of this patient, the procedure was intended to create a more permanent, reliable airway that will provide for adequate ventilation following decannulation. Medical Surgical Module Care Plan #2 4 Pathophysiology Medical/Surgical Primary Medical Diagnosis Diagnosis Acute respiratory Acute respiratory failure (ARF) occurs when the failure, attributed to respiratory system incurs a sudden loss in the ability to vocal cord paralysis effectively exchange oxygen and carbon dioxide with the environment. The three criteria used to diagnose ARF include a PaO2 of less than 50 mmHg, a PaCO2 of greater than 50 mmHg, and pH lower than 7.35. Trauma, infection or obstruction at any point along the respiratory tract can potentially result in ARF. Common pathologies that lead to ARF include cystic fibrosis, pulmonary embolism, severe infection, spinal cord injury and prolonged mechanical ventilation. Vocal cord paralysis can also result when the nerves that innervate the muscles causing dilation and constriction of the larynx fail to function. This loss of function can be idiopathic, but typically results from blunt trauma, cancer or severe infection. When the vocal cords become paralyzed, the larynx is no longer able to maintain patency, and the airway is thus obstructed. ARF related to vocal cord paralysis typically presents in sudden symtpoms such as stridor, severe dyspnea, and weak phonation. An emergent respiratory situation may require the placement of a tracheostomy to bypass the obstruction; if laryngeal paralyisis persists, the cartilage to which the vocal cords attach may be surgically resected to reopen the airway in a procedure called arytenoidectomy. (Phipps et al., 2003) Patient’s Manifestations (Signs and Symptoms) Patient reports experiencing unrelenting hoarseness, periods of dyspnea and expiratory wheezes since being extubated in June of this year after being hit by a motor vehicle. Albuterol treatments, prescribed by patient’s primary care provider, have not been effective in relieving symptoms. Patient experienced a sudden increase in the severity of these symptoms, bringing him to the emergency department. While in the ED, patient began exhibiting stridor and entered acute respiratory failure, the cause of which was determined to be vocal cord paralysis. An emergency awake tracheotomy was performed in the ED to bypass the laryngeal stenosis created by the paralyzed vocal cords, providing patient with an alternative airway. After patient was sufficiently stabilized, an arytenoidectomy was performed to surgically widen the laryngeal inlet for the purpose of restoring the natural airway. Tracheostomy will remain in place until it is determined that the natural airway will be sufficient for ventilation. Since patient was pedestrian-struck in May of this year, it is plausible that trauma attributed to the impact itself, prolonged intubation, extubation, traumatic brain injury, hospital-acquired pneumonia, or a combination of any of these is a potential cause of vocal cord paralysis and resulting respiratory failure. Current treatment includes a combination bronchodilator to promote dilation of the airway and pain management with opioid analgesics. Post-surgical pain is currently insufficiently managed, as patient consistently reports a pain level of 7/10, despite adherence to a strict medication program. Furthermore, patient identifies a tolerable pain level of 4/10. Medication Worksheet Drug Names (Generic, Brand) Time Due Classification & Mech. of Action Heparin (Hep-Lock) Anticoagulant, antithrombolytic. 0600 1400 2200 Inhibits the clotting factors prothrombin or thrombin (dosedependent). Docusate (Colace) Stool softener. Indications Prevention of postoperative DVT/PE. Dose, Route, Frequency 5,000 units sub Q 0900 1700 Oxycodone (Roxicodone) Draws water into colon resulting in softening of stool for ease of passage. Opioid analgesic. Binds to opiate receptors in the CNS, altering the perception of and response to painful stimuli. Most common or serious side effects Bleeding, heparininduced thrombocytopenia, anemia. q8h Promote bowel movement despite reduced bowel motility due to narcotics and analgesia. 100mg Reduction of moderate postoperative pain as needed. 15 mg PO Mild abdominal cramps, diarrhea, skin rash. b.i.d. PO q4h PRN Respiratory depression. Confusion, sedation, constipation. Contraindications & Major Interactions Contraindications: Hypersensitivity, uncontrolled bleeding, severe thrombocytopenia, open wounds. Interactions: Aspirin, NSAIDs, clopidogrel, dipyridamole, some penicillins, ticlopidine, abciximab, eptifibitide, tirofiban and dextran (may increase risk of bleeding). CI: Abdominal pain of unknown origin, nausea/vomiting, loose stool/diarrhea. I: No known significant drug-drug or food interactions. CI: Hypersensitivity, significant respiratory depression, paralytic ileus, acute/severe asthma. I: MAO inhibitors (unpredictable reactions; begin with 25% of usual oxycodone dose). Other CNS depressants, such as alcohol, antihistamines, barbiturates. Potent CYP3A4 inhibitors and inducers. Nursing Interventions and Patient Teaching Nursing Interventions: Assess for bleeding gums, nosebleed, unusual bruising, black, tarry stools, hematuria; fall in hematocrit or blood pressure (may indicate unusual bleeding) Patient Teaching: Report signs of unusual bleeding to HCP; use soft toothbrush and electric razor; avoid potential injury; inform HCP of medication use before treatment or surgery. Nurse should advise patient that Colace is designed for short-term therapy; long-term use may result in electrolyte imbalance, physiological dependence. Encourage patient to use other forms of bowel regulation and to cease use with presence of loose stool. NI: Assess pain factors prior to and one hour post administration. Assess BP, pulse and respirations prior to and throughout therapy. Assess bowel function regularly. PT: Warn patient of abuse potential. Take caution when changing position, ambulating, do not use alcohol while taking this medication. Refrain from driving until effects are known. Educate patient to turn, cough and deep breathe q2h to decrease risk of atelectasis. Hydromorphone (Dilaudid) Opioid analgesic. Binds to opiate receptors in the CNS, altering the perception of and response to painful stimuli. Ipratropium bromide and albuterol sulfate (DuoNeb)* 0500 1100 1700 2400 Bronchodilator. Inhibition of B2cholinergic receptors in bronchial smooth muscle, thereby dilating airway. *Administered by respiratory therapist (Deglin & Vallerand, 2013) Reduction of moderate to severe post-operative pain as needed. 0.4 mg IV Hypotension, confusion, sedation, constipation. CI: Hypersensitivity. Extended release only: significant respiratory depression, paralytic ileus, acute/severe asthma. I: MAO inhibitors (unpredictable reactions; begin with 25% of usual oxycodone dose). Other CNS depressants, such as alcohol, antihistamines, barbiturates. Nalbuphine, pentazocine. Bronchospasm with excessive use. Nervousness, restlessness, tremor, chest pain, palpitations. CI: Hypersensitivity to adrenergic amines, ipratropium, atropine, belladonna alkaloids, or bromide. Acute bronchospasm. I: Other adrenergic agents; MAO inhibitors; beta blockers; tricyclic antidepressants; potassiumlosing diuretics; caffeinecontaining products. q2h PRN Reduce bronchospasms that impede breathing. 3 mL nebulizer q6h NI: Assess pain factors prior to and one hour post administration. Assess BP, pulse and respirations prior to and throughout therapy. Assess bowel function regularly. PT: Warn patient of abuse potential. Take caution when changing position, ambulating, do not use alcohol while taking this medication. Refrain from driving until effects are known. Educate patient to turn, cough and deep breathe q2h to decrease risk of atelectasis. NI: Assess lung sounds, pulse, and BP prior to and at peak of administration. Note amount, color, and character of sputum produced. Monitor pulmonary function tests before initiating therapy and periodically during therapy. Notify provider immediately if wheezing is noted. PT: An unpleasant taste may be experienced. Report cough, nervousness, headache, nausea, GI distress, diaphoresis, dizziness, palpitations, or chest pain occurs, or if shortness of breath is not relieved by medication. Laboratory Values Worksheet Lab Data Normal Value Result #1 (10/13) Result #2 Result #3 Description of Lab Test WBC Number of total leukocytes in the blood. 3.4-10.4 (thousand/mcl) 10.4 N/A N/A Normal The primary phagocytic cells present in early inflammation. 1.8-7.8 (thousand/mcl) N/A N/A Neutrophils 9.4 N/A Participate in cellular and humoral immune response. 1-4.8 (thousand/mcl) N/A Lymphocyte 0.8 Remove dead and injured cells, cellular debris, microorganisms. 0.3-1 (thousand/mcl) N/A N/A Monocytes 0.1 High; Indicates infection or inflammation. Likely high due to the physiological stress this patient is experiencing due to respiratory failure. Low; could be caused by a variety of things, including infection. Patient has had a recent history of infection and ilness that may be contributing to lymphocytopenia. Low; could be caused by a variety of things, including infection. Patient has had a recent history of infection and ilness that may be contributing to monocytopenia. A protein contained within the erythrocyte, which is responsible for binding to and transporting oxygen throughout the body. 13.5-17.5 (thousand/mcl) N/A N/A Hemoglobin 15.3 Hematocrit Portion of a volume of blood occupied by erythrocytes. 40-51 (thousand/mcl) 44 Platelets Cell fragments capable of aggregating and adhering to form clots, thereby limiting blood loss. 150-450 (thousand/mcl) 221 Serum Na Imperative to cell membrane transport, acid-base balance and metabolism. 136-145 mmol/L 139 Serum K Imperative to nerve and muscle function, acid-base balance, renal function and intracellular osmotic pressure. 3.5-5.1 mmol/L 4.2 Serum Cl Imperative to acid-base balance, extracellular osmotic pressure and renal function. 101-111 mmol/L 105 Serum CO2 Measure of the serum bicarbonate level; indicative of acidbase balance. 20 to 29 mmol/L 24 BUN A measure of urea nitrogen as a product of protein breakdown in the blood. 9-26 mmol/L 14 Creatinine Estimation of glomerular filtration rate. 0.7 to 1.3 mg/dL 0.8 Glucose Measure of the body’s ability to manage blood glucose levels. 70-105 mg/dL 133 Pathophysiology Normal N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A N/A Normal Normal Normal Normal Normal Normal Normal Normal High; Patient does not have a history of diabetes mellitus nor is he being monitored or treated for DM, so high blood glucose may be attributed to non-fasting state. Ca ABGs: pH pO2 pCO2 HCO3 BE On room air or what % O2 Indicative of renal function, endocrine function; calcium is essential to proper nerve and muscle function. 8.6-10.6 mg/dl 9 Measure of components of the blood which contribute to pH. pH: 7.35-7.45 pO2: 70-95 mmHg pCO2: 35-45 mmHg HCO3: 22-26 mEq/L BE: 0-2 meq/L pH: 7.41 pO2: 79 pCO2: 46 HCO3: 28.5 BE: 3 Room air (Phipps et al., 2003) N/A N/A N/A N/A Normal Bicarbonate and base excess both exceed normal range. Elevated bicarbonate, slightly elevated CO2 and normal pH is potentially indicative of metabolically-compensated respiratory acidosis. Patient was likely not ventilating optimally at this time, and thus retaining CO2; his kidneys could have compensated by releasing more bicarbonate in attempt to alkalize the blood. Diagnostic Testing Worksheet (e.g., x-ray, ECG, colonoscopy, etc.) Tests Purpose of Test Biopsy: partial right and left arytenoid tissue Microscopic examination of the surgically excised arytenoid tissues to determine whether a possible structural contribution to vocal cord paralysis exists. Date of Test Test Results 10/17 Right and left tissue specimens both appear normal, and are composed predominately of mature cartilage. Chest X-ray (single view) Confirmation of tracheostomy tube placement. 10/14 Lungs clear. Small amount of air in the mediastinum (pneumomediastinum). Tracheal tube in place. Chest X-ray (single view) Rule out pneumothorax and pneumonia as a potential cause of acute respiratory distress. 10/13 Lungs clear. No evidence of pneumothorax. Stable, moderate pneumomediastinum noted. Mind Map Key Problem: Acute pain Key Problem: Risk for infection Supporting Data: Chief Complaint/Medical Diagnosis (Reason for needing health care): Hiatal hernia; GERD Surgical site (tracheostomy) Anticipated assessments (prep): Neurological, Invasive tracheal tube cardiovascular, respiratory, pain, mobility, Trach care infx potential tracheostomy site, IV sites Multiple IV sites Actual assessments (care plan): Neurological, Reduced activity cardiovascular, respiratory, pain, ROM, mobility, Multiple invasive surgeries tracheostomy site, IV sites, GI, psychosocial Compromised airway Potential for aspiration Supporting Data: Pain rating 7/10 Requesting pain meds Facial grimacing, flinching esp. during trach care Successive surgeries Key Problem: Activity intolerance Key Problem: Ineffective airway clearance Supporting Data: Key Problem: Verbal communication Supporting Data: Supporting Data: Acute pain (7/10) Successive surgeries Respiratory secretions in TT Opioid analgesic use Ineffective airway due to Tracheostomy placement Excess respiratory secretions Patient unable to vocalize Expiratory wheezing Non-verbal communication Coarse overall lung sounds with dim bases (nodding, gesturing, writing on white board, mouthing words) Oxygen saturation lower than optimal (91% versus 95-100%) mucous production Patient reports fatigue Problem List and Nursing Diagnoses Problem 1. Ineffective airway clearance Nursing Diagnosis with R/T and AEB Ineffective airway clearance R/T excess respiratory secretions secondary to tracheostomy AEB expiratory wheezing, diminished lung sounds in bases, and patient complaints of periodic dyspnea. 2. Acute pain 3. Risk for infection Risk for infection R/T tracheostomy bypassing upper respiratory tract, respiratory secretion stasis, invasive device and compromised skin integrity secondary to tracheostomy and surgical procedures. 4. Activity intolerance 5. Impaired verbal communication Impaired verbal communication R/T inability to produce speech secondary to inflated tracheostomy cuff, AEB patient unable to speak on assessment and using nonverbal communication such as writing on white board. Medical Surgical Module Care Plan #1 12 Nursing Diagnosis Priority # 1: Ineffective airway clearance R/T excess respiratory secretions secondary to tracheostomy AEB expiratory wheezing, diminished lung sounds in bases, and patient complaints of periodic dyspnea. General Goal: Patient will maintain a patent airway. Outcome: Patient will maintain 02 saturation of 90% or greater throughout my shift, and demonstrate techniques designed to improve airway patency, such as directed coughing, by the end of my shift. Interventions Encourage patient to perform directed coughing to clear airway Rationale Directed deep breathing and coughing exercises are effective in mobilizing and expelling secretions that block the airway, and may also be instrumental in providing the high pressures needed to optimally expand and ventilate the lungs. (Fink, 2007, p. 1212) Patient Responses Actual: Patient successfully performs directed coughing technique to clear the airway. Expected: Patient might engage in hourly coughing exercises to maintain consistent airway patency and prevent buildup of secretions. Educate patient about the purpose of maintaining humidification of inspired air A tracheostomy intentionally bypasses the upper airway, which, under normal conditions, filters and humidifies inspired air. Insufficiently humidified air entering the lower respiratory tract leads to dehydration – and thus increased viscosity – of respiratory secretions, which can result in ciliary assault and increased risk of pulmonary infection, atelectasis, and impaired gas exchange. (Dawson, 2014, p. 66) Actual: Though I did not provide explicit education regarding the importance of humidification at this time, patient intentionally maintains the position of humidification mask near stoma. Expected: Patient will be able to communicate the rationale behind humidification. Maintain continuous pulse oximetry and educate patient about techniques to employ if O2 drops below 90% Optimal oxygen saturation ranges from 95 to 100% on room air, while a reading of below 90% suggests hypoxemia. Prolonged hypoxemia can eventually result in tissue hypoxia. Patient can be educated about the purpose of pulse oximetry (Valdez-Lowe, Gharreb, & Artinian, 2009). Additionally, the patient may be taught techniques designed to improve O2 saturation when the pulse oximeter reads lower than 90%. Such techniques might include focused breathing efforts, repositioning to optimize airway and maximize lung function, or directed cough to loosen and/or expel secretions (Fink, 2007, p. 1212). Expected: Patient will successfully demonstrate techniques that optimize ventilation in the lungs and oxygenation of the blood and tissues, and communicate when and how these methods should be used in conjunction with pulse oximeter monitoring. Evaluation of outcome: Outcome met, evidenced by the patient maintaining a pulse oxygen saturation of at least 90% observed in hourly rounding. Patient was able to demonstrate of ability to perform directed coughing to clear the airway, and displayed understanding of the purpose of humidification by maintaining position of the mask. Medical Surgical Module Care Plan #1 13 Nursing Diagnosis Priority #2: Risk for infection R/T tracheostomy bypassing upper respiratory tract, respiratory secretion stasis, invasive device and compromised skin integrity secondary to tracheostomy and surgical procedures. General Goal: Patient will remain free of infection. Outcome: Patient will remain free of signs and symptoms of infection (e.g., fever, malaise, redness, swelling, pain, purulent drainage, adventitious breath sounds) of stoma site and respiratory tract for the duration of my shift. Interventions Encourage twice daily oral hygiene (tooth brushing and 0.12% chlorhexidine rinse) Rationale Aspiration of bacteria contained in oral biofilms is a potential cause of pulmonary infection, including hospital-acquired pneumonia. The risk is particularly great among high-risk individuals such as the elderly, critically ill and mechanically ventilated patients. One pilot study found that among various protocols tested, twice daily oral care, including manual tooth brushing followed by a 0.12% chlorhexidine rinse, was the most effective in reducing the incidence of pneumonia (Quagliarello, Juthani-Mehta, Ginter, Towle, Allore, & Tinetti, 2009). Patient Responses Actual: Though patient was not supplied with a chlorhexidine mouth rinse, nor was he educated regarding the increased risk of aspiration pneumonia with insufficient oral hygiene, he nonetheless spontaneously performed oral care after meals. Head of bed at least 30 degrees when on bed rest Artificial airways such as tracheostomy increase the risk of aspiration and thus the potential for developing lower respiratory infection. Maintaining the head of bed elevation at a minimum of 30 degrees decreases the risk of aspiration (Guy & Smith, 2009). Actual: Patient’s head of bed was kept at a minimum of 30 degrees, also as an intervention to promote optimal ventilation and comfort. Perform stoma care every 6 hours or more often as needed Due to invasive nature of the tracheostomy, the stoma site should be inspected at least every 6 hours for signs of infection or inflammation such as heat, erythema, edema and pain. The area should be thoroughly cleaned according to facility protocol, with special attention to careful removal of dried secretions that might harbor bacteria, especially around sutures. (Morris, Whitmer, & McIntosh, 2013). Actual: Tracheostomy care was performed every 6 hours as directed. Patient tolerated procedure well and showed no signs or symptoms of infection, including redness, swelling, pain, malodor and purulent drainage. Evaluation of outcome: Outcome met. Patient remained free of apparent signs and symptoms of infection, both at the stoma site and in the respiratory tract. Although lung sounds were not clear throughout, and patient continued to display expiratory wheezes by the end of shift, no changes in lung sounds occurred that might suggest development of infection or worsening of breathing ability. Medical Surgical Module Care Plan #1 14 Nursing Diagnosis Priority #3: Impaired verbal communication R/T inability to produce speech secondary to inflated tracheostomy cuff, AEB patient unable to speak on assessment and using nonverbal communication such as writing on white board. General Goal: Patient will communicate non-verbally Outcome: Patient will identify his preference for non-verbal communication tools/techniques, and apply them successfully by the end of my shift. Interventions Repeat message back to patient for confirmation Rationale Provided the patient does not possess auditory barriers to communication, verbally repeating the patient’s message back to the patient gives the patient the opportunity to confirm or deny the accuracy and completeness of the message received. This decreases the chance of miscommunication from patient to nurse, and furthermore demonstrates the nurse’s interest in the patient’s needs. (Finke, Light, & Kitko, 2008) Patient Responses Actual: Patient was able and willing to confirm or deny messages by nodding or shaking head. Provide patient ample time to communicate using non-verbal strategies Despite the time-consuming nature of providing adequate time for patient communication, doing so conveys patient respect, improves accuracy of delivery, and increases overall patient satisfaction. Multiple studies indicate that patient anxiety and frustration increase, and emotional and physical health suffers when patients lose the ability to successfully communicate with their caregivers. (Finke et al., 2008) Actual: Messages were confirmed only after patient indicated closure (setting pen down, making eye contact). Patient’s behavior conveyed no indication of frustration or dissatisfaction. Allow patient to determine which non-verbal communication methods work best Patients communicate best with methods that are individualized to them (Ackley & Ladwig, 2011, p. 233). Some patients will prefer the use of a white board, while others will prefer the use of picture cards or pantomiming; some will prefer to use several techniques in conjunction with one another (Finke et al., 2008). Actual: Patient seemed satisfied in communicating via white board, but resorted to mouthing, pantomiming or nodding head when messages were more simple in nature. Evaluation of outcome: Outcome met. Patient was able to use a variety of non-verbal communication tools, such as writing on the white board, gesturing, head nodding and mouthing to communicate non-verbally. Patient displayed no signs of frustration with communication, no was there any apparent communication breakdown that could not be easily resolved with one or more alternative communication techniques used by the patient. Medical Surgical Module Care Plan #1 15 Evidence Based Practice A systematic review published by Finke, Light and Kitko (2008) explores barriers to, and potential improvements in, communication between the nurse and the patient with complex communication needs (CCN); specifically of concern are those patients with physical or developmental barriers, be they permanent or temporary, to producing speech. Such research is paramount to the role of the nurse as an efficient, thorough and accurate communicator, because patients suffer when communication fails. Anxiety, frustration and even compromised health status are potential risks to the patient when complex communication needs are left unmet. A total of twelve primary studies containing original data were ultimately included in this review, among which four critical themes were explored: 1) importance of nurse-patient communication; 2) barriers to such communication; 3) techniques for overcoming these barriers; and 4) potential improvements for fulfilling complex communication needs. Of the studies, six focused on subjective data from the patient’s perspective, five did so from the nurse’s perspective, and two studies gathered subjective reports from other “carers” such as family members present at bedside. A variety of augmentative and alternative communication (AAC) means, such as mouthing words, use of a dry-erase board, electronic devices and gesturing were explored in the studies. Patients most consistently reported a seeming dearth of effort among nurses to communicate, citing a perceived lack of desire, time and/or knowledge regarding the tailoring and execution of individualized AAC practices. Conversely, nurses who displayed patience and humor with the patient were rated positively. Among the suggestions for improvement were that nurses take more time to talk to and try to understand the patient’s needs; emotions such as anxiety, frustration and resentment were commonly cited consequences of ineffective Medical Surgical Module Care Plan #1 16 communication. From the nurse’s perspective, a lack of time, training, resources and support were largely to blame for communication mishandlings. In addition to feeling burdened in having to engage in difficult and often time-consuming communication, unsuccessful attempts to communicate with the CCN patient left nurses feeling frustrated and powerless, even incompetent. In the two studies that explored the perspective unpaid carers at the bedside, these individuals reported that they were forced to become responsible for communicating between the nurse and the patient, some because they felt that the nurse was incapable of effectively communicating, and others because they felt the nurse was essentially unwilling to do so. Participants in four of the twelve studies offered recommendations for improving nursepatient communication in the complex needs scenario, and among these recommendations, nurses, patients and carers alike agreed on one thing: nurses should receive AAC training and be educated on the implications of ineffective communication with the CCN patient. Among other recommendations, the theme of nurse education and awareness is common throughout, with many patients simply requesting that the nurse exhibit patience and understanding that a lack of effort and empathy can hinder recovery and emotional well being. Though all of the themes, barriers and implications of this research are relevant to my patient, I chose to implement specific interventions that I felt would be of particular importance in providing best care. Since this patient demonstrated determination to successful non-verbal communication, I felt it most necessary to ensure that the message was being received by me in the way it was intended. Therefore, providing as much time as needed for the patient to communicate a message, and repeating the message back to the patient, encourages not only complete, but also accurate communication. Despite having the tools and ability to use those tools, communication is not successful unless the intended message is conveyed its entirety. Medical Surgical Module Care Plan #1 17 Physical Assessment Data BP: 153/94 Pulse: 86 Height: 163 cm Resp: 16 Pulse ox: 91 (ORA) Weight: 77 kg Temp: 37.2 BMI: 29 Pain (Indicate Scale used): 7/10 (Verbal Numerical Rating Scale) Describe pain characteristics (PQRSTU): Soreness and throbbing in throat and chest, particularly acute at tracheostomy insertion site. Pain is exacerbated by movement of head and thorax, during coughing and deep breathing, and in producing speech. Pain is only somewhat managed with opioid analgesics. I&O Restrictions: Regular diet, no restrictions. Emesis: N/A Tube feeding (type and rate): N/A Residuals: N/A Difficulties noted with feeding (e.g., assistance, problems swallowing/chewing): Patient demonstrates no difficulty chewing or swallowing. Patient denies dysphagia, but does complain of discomfort upon swallowing. Hydration status (e.g., dehydrated including associated assessment data): Skin turgor, mucous membranes, urinary output, sputum consistency and level of consciousness are all indicative of good hydration status. Tube/drains (e.g., Chest tube, JP, Hemovac, etc.): 6 Shiley, non-fenestrated tracheostomy tube is midline and secured with sutures. Cuff is inflated to 5 mmHg. Inner cannula is clean and free of secretions and other obstructions. Shift I = O= 1,600 ml 1,100 ml 24 hours intake: 24 hours urine output: 2,500 mL 2,100 mL Activity Ability to walk/gait/weakness: Patient is able to ambulate ad lib and can turn without any demonstrable or reported weakness. Patient able to rise from bed in a maximum of two attempts. Gait is smooth, coordinated and even. Assistive Devices: N/A Sleep habits (e.g., home vs. hospital, sleep aids, equipment, etc): Patient reports improvement in sleep quality and duration since tracheotomy, and fewer episodes of sleep apnea. Medical Surgical Module Care Plan #1 18 Fall risk assessment rating (state tool used): Hendrich II Fall Risk Score of 2 (not a fall risk). Side rails (number): 2 (while in bed) Bed position (Hi-Lo): Low Restraints (e.g., type and why): N/A Neurological/Mental Mental Status: Level of Consciousness (LOC): Awake, alert and calm. Orientation: Oriented to person, place, time and reason for hospitalization. Pupils (e.g. PERRLA/ size in mm): PERRLA, 4mm. Motor (e.g. ROM X 4 extremities): Full range of motion displayed in all four extremities. Sensation (e.g. X 4 extremities): No loss of sensation, numbness or tingling in extremities. Sensory deficits (e.g. hearing, vision, taste, smell, sensation): No objective or subjective indications of deficits. Describe any sensory deficits (e.g., HOH) and any adaptive devices utilized (e.g. hearing aids, eye glasses): Eyeglasses used for distance only. Can this person express her/himself clearly and logically? Patient is able to successfully communicate with healthcare personnel and spouse via whiteboard or mouthing when speaking becomes too tiresome and painful. No indicators of receptive or expressive aphasia. Patient’s communication, both spoken and written, is semantically clear and logical. Musculoskeletal Bones, joints, muscles assessment data (e.g., fractures, contractures, arthritis, spinal curvatures): No fractures, contractures or abnormal spinal curvature noted. No objective or subjective indicators of arthritis. Devices (e.g., cast/splint/collar/brace) present. Include extremity circulation checks distal to device which includes pulses, temperature, sensation, color, edema): N/A Circulatory devices (e.g. TED hose, SCD’s, etc.): Lower-leg SCDs in use during periods of bed rest. Medical Surgical Module Care Plan #1 19 Cardiovascular Heart Sounds (e.g., S1, S2, regular/irregular, murmur): S1/S2 clearly identifiable; no murmur noted. Apical pulse is strong and regular. Description of Peripheral Pulses: Radial, brachial, dorsalis pedis and posterior tibialis pulses assessed. All are even, regular, non-thready, non-bounding and bilaterally symmetrical. Capillary Refill (in seconds): 3 seconds; upper and lower nail beds assessed. Neck Vein Distention: No evidence of jugular vein distention noted in semi-Fowler’s position. Edema (e.g., degree, pitting, location): None observed aside from that reported at tracheostomy site. Chest pain (e.g., duration, strength, radiation): No complaints of current or previous chest pain. Other: N/A Respiratory Chest Shape: Gently rounded, chest expansion occurs evenly bilaterally. Breathing Pattern (e.g., depth, rate, rhythm, use of accessory muscles): Breathing is unlabored and regular in rate, rhythm and depth; no sign of accessory muscles employed in breathing. Breath Sounds (e.g., clear, coarse, wheezes, location, etc.): Lung sounds are coarse throughout. Expiratory wheezes noted in RUL. Diminished breath sounds in RLL and LLL. Cyanosis (e.g., location, severity): No evidence of cyanosis. Cough (e.g., productive, nonproductive): Productive cough. Sputum (e.g., color, amount, how obtained): Sputum is thin and blood-tinged; moderate amount, produced by cough. Use of O2 (e.g., nasal cannula, mask, trach collar, other): On room air. Flow rate of O2: N/A Humidification: Humidification via mask; placed near tracheostomy. Smoking History (e.g., years smoking, quit date, never): No history of cigarette smoking, but patient does report current, regular marijuana use approximately 2-3 days per week for an estimated 30 years. Medical Surgical Module Care Plan #1 20 Pack Years: N/A Gastrointestinal Appearance: Abdomen is gently rounded and symmetrical, and free of lesions or visible protrusions. Slight ecchymosis noted at heparin injection sites. Abdominal pain (e.g., tenderness, guarding, distention, soft, firm): Abdomen non-distended and soft upon palpation. Patient denies tenderness, and no guarding demonstrated. Bowel sounds (e.g., hypoactive, hyperactive, normoactive, quadrants): Normoactive in all four quadrants. Bowel pattern (including last bowel movement & elimination issues): Approximately 100 mL of loose stool in morning of 10/16. NG tube (describe residual and output): N/A Ostomy (type, stoma site, output): N/A Other: N/A Urinary Urinary pattern (e.g., incontinence, Foley, frequency issues): Voiding without Foley. Patient denies dysuria, frequency or urgency. No hematuria or other signs of GU infection. Catheter: N/A Ostomy: N/A Type: N/A Type: N/A Skin and Wounds Describe skin (e.g., color, turgor, rash, bruises): Slight bruising at heparin injection sites; skin is appropriately warm and uniform in color; turgor is satisfactory. All other parameters unremarkable. Wounds: Skin at tracheostomy site is erythematous and slightly edematous. Thin, blood-tinged mucous drainage cleared from site and dried exudate removed from sutures during tracheostomy care. Dressings (e.g., clean, dry, intact, sutures, staples, steri-strips): IV dressings (2) clean, dry and intact and secured with occlusive dressing and steri-strips. Drains (e.g., type, location): N/A Risk for pressure ulcer assessment (Identify tool used): 20/23 (Braden Scale for Predicting Pressure Ulcer Risk); not a pressure ulcer risk. Medical Surgical Module Care Plan #1 21 Eyes, Ears, Nose, Throat (EENT) Eyes (e.g. redness, drainage, edema, ptosis): Sclera are white, conjunctiva moist and pink, palpebrae are non-edematous. No discharge or lesions noted. Globes are round, normal fundus noted. Eyes appear equal bilaterally. Ears (e.g. drainage): Intact, bilaterally symmetrical and free of lesions or drainage, no complaints of tenderness or pain. Nose (e.g. redness, drainage, edema): Nostrils are patent; nose is non-edematous and nonerythematous; no drainage noted. Mouth (e.g., gums, teeth, mucous membranes): All teeth intact and apparently free of decay, gingivae are pink, non-edematous and free of lesions. Throat (e.g. pain, edema): Trachea and tracheostomy are midline. Patient exhibits strong swallow. Pain, swelling and drainage at tracheostomy site as previously expounded. Psychosocial, Cultural and Spiritual Marital status: Married Occupation: Employed as a scrap metal worker until he was pedestrian struck in May 2014. Spiritual considerations: Patient is Catholic, denies the need for spiritual support at this time. Emotional state: Calm, cooperative and accepting. Cultural needs or habits during hospitalization: None identified by myself, and patient denies the need for additional support. What support systems does this person currently have available? Wife has been bedside for most of patient’s hospital stay and is instrumental in helping patient in performing ADLs, including toileting, bathing, dressing and repositioning. Patient and spouse appear to share a close, positive relationship. Patient’s father and sister have also visited; the overall family dynamic appears to be one of mutual respect and support. Patient cites religious faith and family support for his strength. Medical Surgical Module Care Plan #1 22 References Ackley, B.J., & Ladwig, G.B. (2011). Nursing diagnosis handbook: An evidence-based guide to planning care (9th ed.). St. Louis, MO: Mosby. Dawson, D. (2014). Essential principles: tracheostomy care in the adult patient. British Association of Critical Care Nurses,19(2), 63-72. doi: 10.1111/nicc.12076 Deglin, J., & Vallerand, A. (2013). Davis’s drug guide for nurses (13th ed.). Philadelphia, PA: F.A. Davis. Fink, J. B. (2007). Forced expiratory technique, directed cough, and autogenic drainage. American Journal of Respiratory and Critical Care, 52(9), 1210–1221. Retrieved from http://rc.rcjournal.com/content/52/9/1210.full.pdf+html Finke, E. H., Light, J., & Kitko, L. (2008). A systematic review of the effectiveness of nurse communication with patients with complex communication needs with a focus on the use of augmentative and alternative communication. Journal of Clinical Nursing 17, 2102– 2115. doi: 10.1111/j.1365-2702.2008.02373.x Guy, J. L., & Smith, L. H. (2009). Preventing aspiration: A common and dangerous problem for patients with cancer. Clinical Journal of Oncology Nursing, 13(1), 105-108. doi: 10.1188/09.CJON.105-108. Morris, L. L., Whitmer, A., & McIntosh, E. (2013). Tracheostomy care and complications in the intensive care unit. American Association of Critical-Care Nurses, 33(5), 18-30. doi: http://dx.doi.org/10.4037/ccn2013518 Phipps, W. J., Monahan, F. D., Sands, J. K., Marek, J. F. & Neighbors, M. (2003). Medicalsurgical nursing: Health and illness perspectives (7th ed.). St. Louis, MO: Mosby. Medical Surgical Module Care Plan #1 23 Quagliarello, V., Juthani-Mehta, M., Ginter, Towle, V., Allore, H., & Tinetti, M. (2009). Pilot testing of intervention protocols to prevent pneumonia in nursing home residents. Journal of the American Geriatrics Society, 57(7), 1226-1231. doi: 10.1111/j.15325415.2009.02311.x Valdez-Lowe, C., Gharreb, S. A., & Artinian, N. T. (2009). Pulse oximetry for adults. American Journal of Nursing, 109(6), 52-59. doi: 10.1097/01.NAJ.0000352474.55746.81 Statement of academic integrity: “I have reviewed the Code of Academic Integrity and can attest that this document is consistent with the provisions of the code and represents my own original work. Signed, Samantha A. Redmon.” Medical Surgical Module Care Plan #1 24