High Flow Therapy: Definitions
advertisement

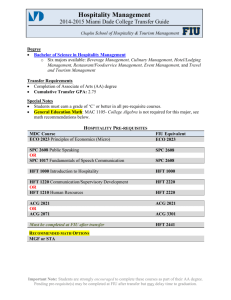
High Flow Therapy (HFT) in the Adult Population Agenda • High Flow Mechanisms of Action • Clinical Application and Research • Precision Flow® Demonstration • Q&A High Flow Therapy: Definitions - Flow rate that exceeds patient flow demands at various minute volumes ● A method to achieve actual FiO2 of 1 ● Eliminate entrainment of ambient air - Accomplished in the nasopharynx only with proper gas conditioning ● Conventional cannula therapy limited by nasal damage ● HFT becomes more than oxygen therapy - Combination of technologies to achieve optimal temperature, humidity and flow rate at the point of delivery HFT Clinical Review Flow First™ 4 Continuum of Care: Old Model Weaning Rescue Acuity Mechanical Ventilation Bi-Level CPAP Bi-Level CPAP General 02 Therapy General 02 Therapy Choice of Therapy 5 Continuum of Care: New Model Weaning Rescue Mechanical Ventilation Acuity Bi-Level CPAP Bi-Level CPAP High Flow Therapy General 02 Therapy General 02 Therapy Choice of Therapy 6 Control the Factors that Matter… Combination of proprietary technology to achieve optimal: Flow Fi02 Temperature Humidity at the point of delivery. High Flow Therapy: Mechanisms of Action Flush Dead Space ● CO2 Elimination ● Oxygen Efficiency Supports Inspiration ● Cannula Flow > inspiratory ● Work of Breathing Humidify / Warm Airways ● Mobilization of Secretions ● Nasal comfort 8 Humidify / Warm Airways Inspiratory Gas Conditioning ●Nasopharynx is highly efficient at conditioning inspiratory gas ●Anatomical Structure ●Mucosal Architecture Humidify / Warm Airways Humidify / Warm Airways Conditioning Prevents Injury Inadequate warming and humidification can cause: ● Thickened Secretions ● Decreased mucocilliary action ● Thermal challenge ● Bloody secretions ● Lung atelectasis Inspiratory Gas Conditioning Why BTPS? ●Williams et al, 1996, Crit Care Med 24(11): 1920-9 Flush Dead Space & Support Inspiration Pulmonary Physiology Oxygenation PiO2 ~150 mmHg Ventilation Ambient Air PiCO2 ~0 mmHg PAO2 ~100 mmHg Alveolar PACO2 ~40 mmHg PaO2 ~95 mmHg Blood PaCO2 ~40 mmHg Pulmonary Physiology and Dead Space Pulmonary Physiology and Dead Space Pulmonary Pathophysiology Pulmonary Pathophysiology Flush Dead Space & Support Inspiration ● High nasal flow, unimpeded at mouth, fills the upper airways – storing O2 during exhalation and flushing CO2 ● High mask flow, impeded by pressure at the mouth - stores less O2 in the upper airways during exhalation and adds prosthetic dead space Tiep, et al: Resp Care, 2002: High Flow Nasal vs High Flow Mask oxygen delivery: Tracheal Gas Concentrations Through an airway model Mechanism of Action Review Dead space washout ● Supports CO2 ventilation ● Enhances oxygenation Matched inspiratory flow ● Attenuates nasopharyngeal resistance Adequate gas conditioning ● Improves conductance and compliance ● Reduces energy cost of gas conditioning Mechanisms by Application HFT DOES NOT TREAT A DISEASE, THE MECHANISMS TREAT SYMPTOMS Oxygen Flush Humidity Mild Pressure COPD Fibrosis Asthma CHF Here are merely a few disease states and how the mechanisms of action treat the symptoms. Can you think of other respiratory insufficiencies where the symptoms can be treated by HFT? 21 The Interface…Delivering the Flow Platform “A” 22 Platform “B” Calculating Minimal Flow AARC Definition…. ……flows that exceed patient demand at various minute volumes. Textbook Adult Values: Tidal volume = 500ml Breathing rate = 12 / min Inspiratory fraction = 0.3 Spontaneous Inspiratory Flow avg. = 20 lpm + what is the peak flow? + Are they larger? + Are they breathing heavy? Err Aggressively…but within reason Calculating Minimal Flow Extrapolated from equations in Mosby’s Respiratory Care Equipment, 7th Ed. Flow Requirements: Adults Inhalation: RR = 12+ Tidal Volume = 500ml Inspiratory time fraction = 0.3 (~1.5 sec) = 25 - 35 LPM Exhalation: Expiratory time = ~3.5 sec Extrathoracic dead space = 0.8 ml/kg (~50 ml) Inhalation flow is sufficient 25 Indications for Use: Indications: ● Spontaneously breathing patients who are requiring supplemental oxygen therapy ● Any patient who is on an oxygen mask that is: 1. Not compliant, 2. not improving, 3. Or has an increase in work of breathing ● Post- extubation support or weaning from NPPV ● Patients requiring supplemental heat & humidity for artificial airways Contraindications: ● Patients not spontaneously breathing ● Patients that have a deviated septum ● Patients with severe facial trauma or disfigurement Clinical References ● Calvano et al. - Respir Care 2008; 53(12):1739-43. - HFT stabilizes end-stage respiratory failure patient on HFT just to make her comfortable when she refused intubation and biPAP. ● Dewan & Bell. - Chest 1994;105:1061-5 - Oxygenation improved but also work tolerance and reduced dyspnea with high flow cannula ● Hasani et al. - Chron Respir Dis 2008: 5, 81-6 - Showed that mucocilliary functions are actually improved with BTPS humidification ● Chatila et al. - Chest 2004;126:1108-15 - Temple Lung Center in Philadelphia showed in COPDers that with Vapotherm blood O2 and CO2 improves as did work performance. ● Dysart et al. - Respir Med 2009;103:1400-5 - Summarizations of the Mechanisms of Action of HFT Precision Flow® Overview • Flow, FiO2, Temperature All In One • One Control, Easy To Use • Smart Technology • Robust Design w/ Limited Maintenance • Audio/Visual Alarm Functionality • Quick Start Up • No Disinfecting Precision Flow™ Integrates Humidification and Gas Blending in One Device Main Unit - Front Panel Flow Display Oxygen Display Temperature Display Alarm Mute and Display Dim Run, Standby Button Setting Control Knob Safety Features Battery Low, Charging Blocked Tube Alarm Disposable Water Path Fault or Absent Cartridge Fault Water Out Alarm System Fault Alarm High and Low Cartridge Indicators Gas Supply Fault Disposable Patient Circuit (DPC) The Disposable Patient Circuit (DPC) Consists of Water Spike Filter Membrane Three Components: 1. Disposable Water Path (DWP) 2. Vapor Transfer Cartridge (VTC) 3. Patient Delivery Tube Cartridge Sensors 30 Day on Single Patient Available Low or High Flow Kits Impeller Heater Plate Delivery Tube Precision Flow Overview: Vapor Transfer Cartridge: ● Key to efficient, high performance humidification and gas conditioning ● Also serves as filter--pore size much smaller than 0.05 microns Patient Delivery Tube: ● Patented triple lumen design ● Design prevents rain-out ● Keeps gas conditioned out to patient ● Safer than traditional heater wire design Q&A