Palliative Care: Achieving Comfort for those with
advertisement

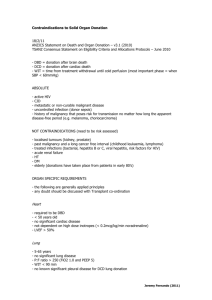
Breakout Session A: “Wait!! This patient is NOT brain dead… How can they be a donor?” Donation After Cardiac Death Case Studies Moderator: • Margie Whittaker, RN, Mission Hospital Presenters: • Julie Vaupel-Phillips, RN, CHOC Children’s • John Brady, RN, St. Mary Medical Center • Esther Montoya, RN, OneLegacy WAIT!! THIS PATIENT IS NOT BRAIN DEAD…HOW CAN THEY BE AN ORGAN DONOR? Moderator: Margie Whittaker, RN Manager SICU Mission Hospital TRANSPLANT TIME LINE 1954 First Successful Kidney Transplant 1962 First Successful Cadaveric Kidney Transplant 1963 First Successful Lung Transplant 1967 First Successful Heart and Liver Transplant “HOW TO BE…” Being in action! The answers are in the room “Report out” on Questions to Run-on: • Scribe • Spokesperson All Teach / All Learn QUESTIONS TO RUN ON… How will you apply what you learned today during future end of life care plans? How will you remember to include donation? OBJECTIVES By the end of this presentation, the attendee will be able to: 1. Identify best practices in DCD 2. Recognize the importance of collaboration and communication in donation 3. Describe strategies to improve the DCD process Pediatric Donation After Cardiac Death (DCD) Julie Vaupel-Phillips, MHA, RN, CCRN Director of PICU and ETS Services CHOC Children’s Hospital Donation Facts • In the USA 1% all deaths are considered brain death. • One organ donor has the potential to save up to 8 people by donating organs and may provide 50 people with tissue and cornea transplants. • There are more people on the organ wait lists than organs available. 18 people die each day waiting for an organ transplant • Literature shows that parents want to be asked about organ donation, including donation after cardiac death. • Families of children are more likely to agree to organ donation than families of adult patients. Donation after Cardiac Death (DCD) • DCD offers an option to patients and families who may wish donation to occur after life sustaining equipment is withdrawn, and death is determined by cardiopulmonary criteria. • For DCD to occur, patient death is determined by cessation of cardiac & respiratory function, rather than by the absence of cerebral and brain stem function. • DCD is generally practiced in the USA Donation after Cardiac Death Things to think about: • Some children die despite all our efforts • Death is not a failure • Death is a natural part of life. • Donation is a family driven process. • The family has already made the decision to allow the patient to die. • The families decision to donate must be separate from their decision to withdrawal of support. • Family participation is essential • The patient must always be provided comfort measures Donation after Cardiac Death at CHOC Children’s Hospital • 2005, Q3 1 DCD • 2006, Q1, Q3 2 DCDs • 2007, Q3 1 DCD • 2008, Q3 1 DCD • 2009 0 DCD • 2010 0 DCD • 2011, Q1, Q2 Things to Consider with PEDS DCD • The parents may change their mind at any time. • Expect that the parents will want to be present in the OR and hold their child at the time of death. • Expect that the OR will not be comfortable with the parents coming into the OR. • Try to time the OR for evening, night or early am when there are fewer cases in the department. • Request an OR room that has an easy egress but is private so that the family can be as comfortable as possible. • Huddle frequently and often. Case Study • 3 month old female • Twin A • Found unresponsive in crib • Asystolic when arrived in ED • Metabolic workup positive for fatty acid oxidative defect • Parents informed of poor prognosis • Family requested withdrawal of support and asked about organ donation • OneLegacy contacted • Consent obtained for Organ Donation Case Study • Patient prepared for transport to OR. • Patient 4.2 kg, no local recipients. • Stanford University accepts liver and kidneys. • OR Booked for 16:00 • Flight plans set for transplant team to fly from Palo Alto. • Parents request to be close to the OR but will not be present in the OR. Family in secluded area of the OR. • Family Care Coordinator and Priest support the family. • 20 minutes from OR time, the transplant team experiences an in-flight emergency • Flight is diverted to Sacramento Case Study • Family is informed but are willing to wait the 3-4 hours it may take to get the team down to Orange County. • Transplant team arrives (8 pm) and patient brought back to the OR. • Parents placed in secluded OR room. • Withdrawal of LST performed by the PICU Intensivist. • Patient was pronounced dead 11 minutes after withdrawal of life support. • Parents immediately informed, baby blanket and toy returned to them. • Surgery starts after 5 minutes of observation period. • Liver and Kidneys successfully recovered. Words of Advice… • Support internal staff and each other • Expect the unexpected • Develop a plan − For family-demographics, communicate and explain what will occur, what they will see and hear, and all the what if’s − For patient-palliative care, terminal extubation person, − For staff-roles and responsibilities • Post case debrief (OPO & hospital) for staff involved • Learn something from every case • DCD is patient/family centered care Their lives depend on it! Thank you. Donation After Cardiac Death Case Review St Mary Medical Center Apple Valley John Brady, RN, CCRN, CNRN ICU Nurse Manager Donation at St. Mary Medical Center Organ donors 2000-2011 7 Organ Donors • 5 brain dead • 2 DCD (2006 and 2011) • 17 organs recovered • 14 organs transplanted • 3 organs for placed for research Day 1: Admission 45/M Status post cardio-pulmonary arrest Areflexic Medical history methamphetamine use, high cholesterol, & diabetes Down time 45 minutes Transfer in from local hospital for higher level of care Day 2 Consult to OneLegacy Patient made a DNR Family wanted to extubate soon Family initiated donation discussion with physician Day 2: OneLegacy Consult Family wanted to extubate that evening Awaiting OneLegacy’s arrival to discuss donation Patient’s mother initiated donation topic stating… It was a difficult decision but she wanted her son to save lives through donation. Day 2: OneLegacy Consult OneLegacy discussed donation options with the family. The family consented for both brain death and DCD donation, said their final goodbyes, left the hospital and requested post OR follow-up Hospital planned for EEG on Day 3 Day 3 EEG showed activity, Patient NOT BRAIN DEAD DCD Policy reviewed Huddle with all Champions: Attending Physician, Nurse Manager, Charge Nurse, Bedside Nurse, Respiratory Therapist, Palliative Care, Risk Manager and House Supervisor Day 3 Patient placed on CPAP and shallow breaths were observed; attending physician determined that there was a high probability that the patient would not survive longer than 60 minutes Palliative Care informed the family that EEG showed activity Family confirmed that they wanted to proceed with donation The Next Steps Attending physician aware that he will be pronouncing the patient OR scheduled for 18:30pm 16:00pm patient’s sister called the unit hysterical; the bedside nurse referred caller to speak with the patient’s mother The Next Steps Attending physician became concerned with recent phone call from patient’s sister and requested a second teleconference with the family to confirm donation choice Patient’s mother contacted Palliative care and verified consent for donation OR Delayed Attending physician left hospital at 19:00pm and delegates pronouncement to Hospitalists or ED physician; no new OR time set Risk Manager contacted the Medical Director who instructed the Attending to return to SMRM to pronounce the patient in OR The Gift of Life OR: Pt extubated 20:35pm; pronounced by Attending Physician at 20:59pm (24 minutes) Outcomes: Right Kidney placed locally 61 Female on waiting list 2, 899 days Left Kidney placed locally 60 Male on waiting list 2, 833 days Liver and pancreas placed for research What We Learned Planning Communication Teamwork DCD Data & The Story it Tells Presented by: Esther Montoya RN, MSN ED Donation Development Coordinator OneLegacy 1000 791 800 600 400 560 559 2005 2006 848 920 391 269 200 0 2003 2004 2007 DCDDonors 2008 2009 DCD vs. Brain Dead Donors (United States) 5416 6000 5984 5799 6187 5000 4000 5359 5477 6081 5822 3000 2000 1000 269 391 560 559 791 848 920 0 2003 2004 2005 2006 2007 2008 2009 2010 BDDonors DCDDonors OneLegacy DCD History 30 25 24 25 19 20 14 15 10 5 25 21 16 3rd Qtr 7 2 20 03 20 04 20 05 20 06 20 07 20 08 20 09 20 10 20 11 0 DCD Donors OneLegacy Brain Dead vs. DCD Donors 400 350 3rd Qtr 416 450 326 339 371 359 381 358 324 284 300 250 7% 200 150 6% 4% 4% 4% 5% 4% 7% 6% 100 50 2 7 14 16 25 19 24 25 21 0 2003 2004 2005 2006 2007 2008 2009 2010 2011 Brain Dead DCD OPO DCD Comparison 100 80 60 40 76 60 20 0 72 23 MIOP MAOB 2008 PADV 2009 CAOP 2010 OneLegacy (CAOP) compared to high performing OPO’s (DCD) in the US: MIOP= Michigan-Gift of Life MAOB= New England Organ Bank-MA PADV= Gift of Life Donor Program-PA DCD & Organs Transplanted 7.00 6.00 Average=1.84 5.00 4.00 CAOP PADV MAOB MIOP Average=1.66 3.00 2.00 Average=1.80 1.00 Average=1.48 0.00 2008 2009 2010 Potentially 84 More Lives Saved California Donor Registry Designated Donors Among Recovered Donors 50% 45% 40% 37% 33% 35% 30% 25% 20% 28% 25% 46% 42% 38% 41% 37% 33% 30% 27%27% 19% 15% 10% 5% 0% Organ Donors 2007 Tissue Donors 2008 2009 2010 Eye Donors 2011 YTD Trends in Donation • Registered Donors= 20.7 % in our service area, 27.3% Nationally • DCD donors occurred at 52 out of 220 hospitals since (2003-2011) • AA= 33 23% A= 36 25% • B= 30 21% C= 44 31% • Hospitals with DCD P&P’s: 2003 = <2% 2011 = >90% • 2010 Research/study – Clinical trigger cards introduced to selected hospitals to capture DCD potentials. Clinical Trigger Research 2009 2010 2011 2011 3rd Qtr Projection Referrals 4398 5144 3597 5383 Eligibles 549 487 362 541 Donors 382 349 270 406 DCD 24 (6%) 25 (6.9%) 21 (7.4%) 30 (7.3%) What Story does the Data Tell? • Highlights areas of potential growth by trends – DMV and Registered donors – DCD donation TOGETHER WE CAN DO BETTER -PARTNERS FOR LIFE! What we learned? Practices for Success: – Communication and collaboration is key – All inclusive clinical trigger card & early referral – Implementation of supportive P&P’s – Pt. and family centered care philosophy QUESTIONS TO RUN ON… How will you apply what you learned today during future end of life care plans? How will you remember to include donation? WHAT WE LEARNED? Practices for Success: Communication & collaboration is key All inclusive clinical trigger card & early referral Implementation of supportive P&P’s Pt & family centered care philosophy