CLABSI
advertisement

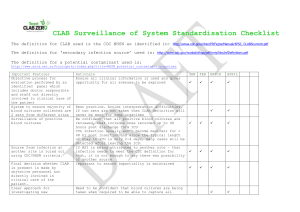
Why Maintenance is so High Maintenance: How to Achieve Success Tamara Johnson RN Director Clinical Integration Ivera Medical Corporation OBJECTIVES Understand why CABSI and CLABSI are important Top 10 Reasons Maintenance is High Maintenance Understand the dynamics associated with Port Protection and compliance and their role in the “maintenance bundle” Overcoming Port Protection challenges (Process Changes) 2 CLABSI TIMELINE 2001 – Beginning of the term “Never Events” 2008 – CMS releases reimbursement guidelines which include Vascular Catheter Related BSIs (no CL modifier) 2011 – National Healthcare Safety Network begins monitoring mandatory surveillance reporting on CLABSI 2012 – Updated CLABSI Definitions from CDC 2013 – Updated CLABSI Definitions from CDC 2014 – Updated CLABSI Definitions from CDC 3 FROM OUR FRIENDS AT THE CDC… Central Line Associate Blood Stream Infection (CLABSI) - a laboratory –confirmed bloodstream infection (LCBI) where the central line (CL) or umbilical catheter (UC) was in place for >2 calendar days on the date of the event, with day of device placement being Day1, and a CL or UC was in place on the date of event or the day before. If a CL or UC was in place for >2 calendar days and then removed, the LCBI criteria must be fully met on the day of discontinuation or the next day. If the patient is admitted or transferred into a facility with a central line in place (e.g., tunneled or implanted central line), day of first access is considered Day 1.1 1. ) http://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf 4 A CENTRAL LINE INCLUDES: Central Venous Catheter (CVC) Peripherally Inserted Central Catheter (PICC) Dialysis Catheter Umbilical Catheter Hickman Catheter Broviac Catheter Groshong Catheter 6 IMPACT OF CLABSI $34, 500 - $56, 000 per episode2 $54,000 - $75,000 in adult Surgical ICU3 80,000 ICU BSI’s a year – leading cause of ICU nosocomial infections4 250,000 CLABSI’s a year2 30,665 deaths a year from CLABSI5 2.) Moreau N. Nursing 2009;34:14-15 3.) Hollenbeak CS. J Infus Nurs. 2011:3309-3313 4.) O’Grady NP, et al. American Journal Infection Control 2011;39(4suppl 1):51-34 5.) Klevens RM, et al. Public Health Rep. 2007;122-160-166 7 MECHANISMS LEADING TO CLABSI6 Pathogen migration along external surface – typically within first 7 days Hub contamination leading to intraluminal colonization Needleless connector contamination leading to intraluminal colonization Established from a different source Contaminated infusions 6.) The Joint Commission. Preventing Central Line–Associated Bloodstream Infections: A Global Challenge, a Global Perspective. Oak Brook, IL: Joint Commission Resources, May 2012. http://www.PreventingCLABSIs.pdf. 8 PROTECTING OUR PATIENTS… Implementation of “Bundles” Bundle7 - a structured way of improving the processes of care and patient outcomes: a small, straightforward set of evidence-based practices — generally three to five — that, when performed collectively and reliably, have been proven to improve patient outcomes. CDC Guidelines for CLABSI Bundles 7.) http://www.ihi.org/explore/bundles/Pages/default.aspx 9 CLABSI BUNDLES Central Line Insertion Practices (CLIP)8 Hand Hygiene All 5 Maximal Barrier Precautions Sterile Gloves Sterile Gown Cap Mask Worn Sterile drape covering entire patient Chlorhexidene gluconate (CHG) Insertion Site Daily assessment to determine need 8.) http://www.cdc.gov/nhsn/PDFs/pscManual/5p sc_CLIPcurrent.pdf 10 CLIP VS MAINTENANCE Extraluminal vs Intraluminal CLIP = happens one time on a patient Maintenance = happens all day long by a lot of different people (#1) 1 vs ??? “Bloodstream infections related to long-term CVC use are almost always a result of intraluminal biofilm development.” - James Davis, RN, CIC Senior Infection Prevention Analyst Pennsylvania Patient Safety Authority 11 CENTRAL LINE MAINTENANCE “GUIDELINES” Hand hygiene compliance ✔ Scrub access port or hub immediately prior to each use with appropriate antiseptic (70% IPA, CHG, provodine iodine) ✔ Access catheters with only sterile devices ✔ Dressing care. Replace wet, soiled or dislodged (using aseptic technique with clean or sterile gloves) ✔ Replacement of administration sets and needleless connectors ✔ Perform daily assessments to determine need for CVL ✔ #2 9.) http://www.cdc.gov/hicpac/BSI/BSI-gui 2011.html 12 NEEDLELESS CONNECTOR DISINFECTION 2007 Java Vol 12, No 3, 140-142 13 Do I need to scrub when I remove CUROS®? “SCRUB THEhas HUB” NO. If CUROS been in place for at least 3 minutes, you do not need to scrub the port before your rst access. 15 seconds Scrub the hub: When there is visible soil on the port (blood, lipids, etc...) Between sequential accesses per hospital protocol: SALINE FLUSH MED ADMIN SALINE FLUSH NEW CUROS Scrub if you remove CUROSand leave the access port exposed for a period of time before accessing. ML-0030 Rev A | 0911 14 IS 15 SEC EVERY SINGLE TIME, EVERY SINGLE ACCESS A PRACTICAL EXPECTATION TODAY? Ideal web page load time 3.5 seconds (2010 PhoCusWright/Akamai Study) #3 15 AND THE SURVEY SAYS… 16 • Sent an electronic survey1 and asked staff nurses to report their compliance involving of Worth a Try: CLA-BSI Reduction disinfection Associated BYU College of Nursing With Alcohol Cap Implementation peripheral and central IV access ports and IV tubing end nursing.byu.edu Lorraine Linford, RN, BS, CNSC; Sharon Sumner, RN, BSN, IP; Carrie Taylor, RN, MSN, CIC; Katreena Merrill, RN, PhD care. CLA-BSI PICC Incidence and Interventions Over Time Purpose • Determine whether an alcohol cap decreases central line associated blood stream infections (CLA-BSI). • Determine the effect of an alcohol cap on the number of contaminated blood culture specimens. • Determine the financial impact of using an alcohol cap. CLA-BSI Pre and post alcohol cap implementation Feedback from Nursing Staff We scrub less than 5 seconds. Background • About 250,000 central line associated bloodstream infections (CLA-BSI) occur annually.2 • CLA-BSI increases patient mortality and costs between $25-55,000 per incident.3 • To prevent infection in patients with IV access devices the CDC recommends disinfecting needleless connectors. • Current disinfection practices may be insufficient protection against microbial contamination. Method • Implemented an alchohol cap in the adult inpatient and NBICU departments of a large tertiary care trauma center in January 2012. • Compared retrospective rates of CLA-BSI, blood culture contamination rates (2011/2012), compliance and financial impact following the implementation of the alcohol cap. • Sent an electronic survey1 and asked staff nurses to report their compliance involving disinfection of peripheral and central IV access ports and IV tubing end care. Feedback from Nursing Staff We scrub less than 5 seconds. If you scrub the connector, select the description closest to your process. Quick swipe with alcohol pad If you scrub the connector, select the description closest to your process. • Opt • Alco Al Al Al Al • Imp • Com Result Quick swipe with alcohol pad Blood Culture Contamination • PLC Method (Continued) • Required education for staff nurses was distributed electronically or in person. Aseptic maintenance of IV tubing end Proper blood culture technique Use of alcohol cap • Monitored compliance to the cap and tubing end management on a weekly basis. • Measured incidence of CLA-BSI and incidence of contaminated blood cultures • Analyzed financial impact Short scrub motion (less than five seconds) Intervention Long vigorous scrub (15 seconds) • Optimizing needleless connector prep prior to IV access • Alcohol impregnated cap placed on: All central line needleless connectors All peripheral IV needleless connectors All IV tubing ports Alcohol swabs for access as needed • Improved aseptic maintenance of IV tubing end • Compliance reported weekly to nursing staff Other (please specify) Results Long vigorous scrub (15 seconds) • PLCC line and overall CLA-BSI rates were significantly decreased (p<0.05). • Blood culture contamination rates showed a moderate decrease (p=7.05). Other (please specify) • Net cost savings using alcohol cap was $683,030. Short scrub motion (less than five seconds) Interve Alcohol Cap Value Analysis Summary 2012 annualized projection dec • Bloo dec • Net Conclu • The the • An a by a Conclusions References 1 use of an alcohol cap may be effective in reducing Evans S,• The Sharp J, Linford L, et Risk of Symptomatic DVT Associated with P the rate of CLA-BSI and contaminated bloodal. cultures. 3 alcohol cap may reduce the annual cost of CLA-BSI • An 17 Infections. 2011. CDC. gov byHollenbeak, C The Cost of Catheter-Related Bloodstream Infections as much as 28% CHALLENGES WITH CLABSIs Many Ports of Entry into the bloodstream #4 18 CHALLENGES WITH CLABSI Cannot See Microorganisms – blessing and curse #5 Culture from a patient’s needleless connector. – Wendy Kaler, MT, MPH, CIC 19 CHALLENGES WITH CLABSI No Immediate Accountability – Patient doesn’t yell OUCH! #6 20 CHALLENGES WITH CLABSI Dynamic Bedside environment – nurse gets interrupted every two minutes #7 21 PORT PROTECTION What is a Port Protector? 70% IPA in a cap Medical grade foam pad To be placed on any swab-able, luer-activated device To disinfect and act as a physical barrier between accesses when not in use 22 HOW A PORT PROTECTOR WORKS Passive Disinfection • • • • • • Chemical agent – 70% Isopropyl Alcohol Time of exposure – 3 - 5 minutes (per DFU) Physical barrier – up to 4 - 7 days if not removed (per DFU) No scrubbing necessary (for first access) FDA 510(k) Single use 23 TYPES OF PORT PROTECTORS 24 ADVANTAGES TO PORT PROTECTION Minimizes risk • Disinfected and protected vs. exposed and contaminated Consistent disinfection • No user variability #8 Saves time* • Hub Scrub not necessary for first access if port protector in place for specified time Visible tool for managing compliance • Allow for complete compliance with TJC NPSG 07.04.01 Peer Reviewed Data Studies have demonstrated reduction in CLABSI, Contaminated Blood Cultures, and Intraluminal contamination • What’s next? • 25 PORT PROTECTOR CLINICAL STUDY Observational before-after study in adult oncology nursing unit (Sweet, 2012) Control period – manual cleaning with alcohol wipes, retrospective CLABSI data 1 year, 472 patients, 6851 central line days 16 CLABSIs, 2.3 infections/1000 catheter days Intervention period – using port protectors on neutral mechanical valve NC 6 months, 282 patients, 3005 central line days 1 CLABSI, 0.3 infections/1000 catheter days Reduction of contaminated blood cultures taken from catheters 26 PORT PROTECTOR CLINICAL STUDY Case-crossover study with PICCs indwelling for 5 or more days, 3 hospitals (Wright, 2012) 1.5 mLs of blood drawn from PICC for culture on days 5, 6, 7 and twice weekly thereafter 3 phases – 799 patients enrolled Manual scrubbing – 32/252 (12.7%) contaminated. 4 cfu/mL median Use of port protector 20/364 (5.5%) contaminated, p=0.002, 1 cfu/mL median Return to manual scrubbing – 22/183 (12%) contaminated, 2 cfu/mL median Avoid 21 CLABSI, 4 fewer deaths, 13 new admissions 27 PORT PROTECTOR CLINICAL STUDY Observational before-after study in 2 adult ICUs (Ramirez, 2012) Control period – manual disinfection with alcohol pad for 15 seconds, normal surveillance data 4 CLABSIs, 1.9 infections/1000 catheter days Intervention period – application of port protectors on all NCs 1 CLABSI, 0.5 infections/1000 catheter days 28 SIX SIGMA PROJECT – TX HOSPITAL 1. Open MAR 2. Scan Medication 3. Prepare Medication 4. Open Alcohol Pad = 66 sec per injection 5. Scrub Hub for 15 sec 6. Dry for 15 sec 7. Administer Medication (Avg. time spent in 12hr shifts giving IV injections) 29 ADVANTAGES TO PORT PROTECTION 1. Open MAR 2. Scan Patient 3. Scan Medication 4. Prepare Medication = 23.7 sec per injection 5. Remove Port Protector 6. Administer Medication 7. Replace with new port protector 64 % reduction! 30 EVEN SIMPLE SOLUTIONS HAVE CHALLENGES The “Silver Bullet Syndrome” Hand Hygiene Clean, Dry, Intact Dressings Confusing Protocol Forced Compliance vs. Non-Forced Compliance 31 COMPLIANCE Forced Compliance Car keys • Need them to drive car Non-forced Compliance Seat Beat • Car drives fine without seatbelt • Need for HARD WIRED habit #9 32 MAIN CHALLENGE? #10 33 Thank You! Questions? 34 CHALLENGE ACCEPTED Product Location Easy access – grab and go Education – reinforce the “WHY” Process vs. Product Simple Protocols All Patients, All Lines, All the Time Eliminates confusion Supports Behavioral Changes Auditing Reinforcement to “hardwire” new process – 21 Days Management engagement Visibility to actual practice 35 AUDIT PROGRAM – UNIT BASED • Real time feedback/education • Accountability • Share compliance results • Nursing leadership support “If can not measure it, you can not improve it.” – Lord Kelvin • • • • • Clinical ladder Magnet story CUSP HEN IP Liaisons ADVANTAGES TO PORT PROTECTION 37 The single biggest problem with COMMUNICATION is the illusion that it has taken place. - George Bernard Shaw 38 REAL TIME COMMUNICATION Post Compliance Rates Staff nurses, management, CLABSI committee Share Success Stories Prime tubing in med room, place PP on Celebrate Victories Reward positive Gain more champions 39 WEEKLY UNIT REPORTING SICU CUROS AUDITING FORM Enter data by 5 pm every Monday Patient Compliance - Blue Line 3 5 8 10 9 10 10 11 10 11 Port Compliance - Red Line 10 15 40 39 15 20 25 45 39 17 Weekly Trends 100%+ 90%+ 80%+ 70%+ 60%+ 50%+ 40%+ 30%+ 20%+ 10%+ 0%+ 4-Mar+ 11-Mar+ 18-Mar+ 25-Mar+ 1-Apr+ 8-Apr+ 15-Apr+ 22-Apr+ 29-Apr+ 6-May+ 13-May+ 20-May+ 40 CELEBRATE SUCCESSES 41 I DON’T HAVE TIME! 42 ORGANIZATIONS WHERE ONE BREACH IN PROCESS CAN IMPACT LIVES… 43 MONITORING PROCESS COMPLIANCE High reliability organizations, i.e. military, aviation, nuclear power Continuous monitoring of critical processes # of observations Multidisciplinary/multidepartmental Process examples Line insertion Line entry Provide feedback - immediate and monthly Monitoring & Effect on CLABSI rate Bundle use alone not associated with lower CLABSI rate. Rate when process monitored & achieved > 95% compliance Furuya et al; Presentation at Fifth Decennial International Conference on HAI. March 2010, Atlanta. 44 SHEA/IDSA PRACTICE RECOMMENDATIONS INFECTION CONTROL AND HOSPITAL EPIDEMIOLOGY, VOL. 35, NO. 7 (JULY 2014) PP. 753-771 2014 Update Section 1: Rationale and Statements of Concern Section 2: Background – Strategies to Detect CLABSI Section 3: Background – Strategies to Prevent CLABSI Section 4: Recommended Strategies for CLABSI Prevention Basic Practices Special Approaches Section 5: Performance Measures Internal Reporting External Reporting Section 6: Examples of Implementation Strategies Engage Educate Execute Evaluate 45 $$$ REIMBURSEMENT FYI 2015 HAC Reduction Program (1%) Penalty enforced after VBP & Readmission adjustments Domain 1 – AHRQ 35% PSI-7 CLABSI PSI-13 Sepsis Domain 2 – CDC Measure 65% CAUTI CLABSI VBP (Zero Sum Bucket) (1.5% - 2% in 2017) Improvement (Self) – current performance vs baseline Achievement (Others) – how does current performance stack up to others Both make up your Total Performance Score Readmission Reduction Program (3%) 46 CONCLUSION CABSI and Central Line Definitions Challenges with BSI Prevention No immediate accountability It only takes ONE exposure to put a patient at risk Overcoming BSI Challenges Education as to WHY Monitoring maintenance care ENGAGE NURSING LEADERSHIP – Unit based programs Important tools to assist Port Protection Visual auditing tool Means to communicate compliance 47 ANY QUESTIONS? 48