CLABSI
advertisement

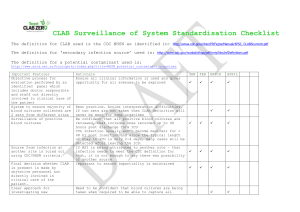
Factors determining success in reduction of Central Line Associated Blood Stream Infection (CLABSI) on statewide levels HeeWon Lee, Doris Duke Clinical Research Fellow PI Peter Pronovost, M.D. PhD., Bradford Winters, M.D. PhD. Background CLABSI • A common, costly, and fatal cause of hospital-related deaths, with approximately 31,000 annual deaths in the US • $3 billion spent worldwide.1 • However, CLABSIs are preventable.2,3 1. Klevens RM, Edwards JR, Richards CL Jr, et al. Estimating health care-associated infections and deaths in US hospitals, 2002. Public Health Rep. 2007; 122(2):160-166. 2. Edwards JR, Peterson KD, Mu Y, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37(10):783-805. 3. Berenholtz SM, Pronovost PJ, Lipsett PA, et al. Eliminating catheter-related blood stream infections in the intensive care unit. Crit Care Med. 2004;32(10):2014-2020. Background On the CUSP: Stop BSI • Project led by the Johns Hopkins Quality Safety Research Group • Implementing a two-component, multifaceted hospital safety program has – Saved lives, health care $ – Reduced CLABSIs by 66% – Sustained a median infection rate of 0, and mean of 1 infection per 1000 catheter-days for more than 3 years in Michigan.4 4. Pronovost PJ, Goeschel CA, Colantuoni E, et al. Sustaining reductions in catheter relate bloodstrea infections in Michigan intensive care units: observational study BMJ. 2010;240:c309. Background On the CUSP: Stop BSI Timeline Hospital recruitment, registration, orientation with QSRG on CUSP Month 0 Month 3 Implementation of program: 1. Evidence-based Behaviors to Prevent CLABSI 2. Multifaceted Safety Program 1. Continued contact with QSRG 2. Data collection--submission of monthly CLABSI and monthly team checkup tool data Month 28 Background On the CUSP: Stop BSI I. Evidence-based Behaviors to Prevent CLABSI5 1. Remove Unnecessary Lines 2. Wash Hands Prior to Procedure 3. Use Maximal Barrier Precautions 4. Clean Skin with Chlorhexidine 5. Avoid Femoral Lines 5. Marschall et al. Infect Control Hosp Epidemiol 2008. CDC.gov Background On the CUSP: Stop BSI II. Multifaceted Safety Program (Team Checkup Toolkit)5 1. Learning from Defects 2. Daily Goals Checklist 3. Morning Briefing 4. Observing Rounds 5. Shadowing Another Profession 6. Culture Debriefing 7. Physician Call List “When we all work together, we all win together” Background Expansion of Stop BSI Project Overall goal: 75% national reduction in CLABSI over 3 years But wait! Problems exist… • Despite the expansion of the program to numerous states… – Median rates of CLABSI remain high or unchanged – Some hospitals claim to use the checklist, despite having high or unknown infection rates – Some hospitals say that the ICU patients are too sick and that infection is inevitable – Hospital enrollment in the program has been slow.6 6. Department of Health and Human Services. Department of Health and Human Services initiative http://www/jjs/gpv/ Accessed July 1, 2010. What factors are associated with success of reducing CLABSIs? Hypothesis States with higher rates of meeting the CLABSI reduction goals are associated with greater hospital participation and adherence to the two-component, multifaceted safety program. CLABSI definition7 • For determining CLABSI rate – Numerator: # of CLABSIs – Denominator: # of central line-days – Expressed as a rate of X CLABSI/1,000 central line days • #CLABSI/# central line days X 1000 7. National Healthcare Safety Network (NHSN): Device-Associated (DA) Module www.cdc.gov/nhsn/psc_da.html. Accessed July 1, 2010. Study Design Prospective observational cohort study Hospital recruitment, registration, orientation with QSRG on CUSP 1. Continued contact with QSRG: hospital participation and dropout rates 2. Data collection--submission of monthly CLABSI and monthly team checkup tool data Month 0 Month 3 Month 28 Baseline CLABSI rate 1o outcome: 2o outcome: Reduction of CLABSI from baseline rate in the first 3 months of participation Sustained reduction of CLABSI from baseline rate after 28 months of initiation of project Stratification Hospitals by… • Teaching status • Bed size • Presence in a state with mandatory participation in the National Healthcare Safety Network (NHSN) States by… • Number of teaching/academic institutions present • Presence of mandate to report Statistical methods 1. Two sample Wilcoxon rank-sum test for comparison of medians with baseline CLABSI rates 2. Poisson regression modeling for comparison of CLABSI rates before, during, and up to 3 and 28 months after implementation of program Limitations of study • Observational study • Confounders? • Inconsistent data from individual hospitals regarding use of multifaceted toolkit Implications of study • CLABSI are preventable! – On the CUSP: Stop BSI project has demonstrated effective elimination of CLABSI on a statewide level in Michigan • Many states are participating, but CLABSIs still exist • Study is the first of its kind in examining all participating states and CLABSI rates • By identifying factors associated with success in reducing CLABSI, we may be better able to reach the goal of reducing and eventually eliminating CLABSI, further helping save lives and healthcare $ Acknowledgements • Small group leaders: – Dr. Vered Stearns, Dr. Pete Miller • Small group members: – James Chen, Hormuz Dasenbrock, Andrew Ibrahim, Kevin Jeng, Yong Suh • Research mentors: – Dr. Bradford Winters, Dr. Peter Pronovost • QSRG team members