communication challenges - Dynamics of Health Care in Society Mrs
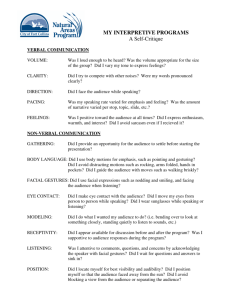
advertisement

Dynamics of Care in Society Communication 1 Objectives: Identify & define the concepts & elements of communication theory Recognize a communication dilemma Identify nonverbal aspects of communication Utilize sensitivities & problem solvng skills to achieve interpersonal communication that occurs in the health delivery process Formulate appropriate communication strategies to detect & avert breakdowns in communication Differentiate between open & closed ended questions Develop skills to design open-ended questions Determine the appropriate questions to ask patients Be familiar with appropriate, caring responses Know how to obtain help if there is a language barrier Communication defined: a sharing of information or ideas, including content as well as the feelings or emotions Verbal & nonverbal behavior within a social context Listen…Talk to your doctor Methods of COMMUNICATION •One on one •Small group •Large audience •Mass communication TV, radio, film, newspapers, internet FORMS OF COMMUNICATION: 1. VERBAL: spoken words, manner, tone, non-language sounds (sighs or sobs) 2. NON-VERBAL: touch, eye contact, kinesics (body movement), proxemics (personal space) 3. WRITTEN: letters, memos, chart documentation, agendas, reports… COMMUNICATION PROCESS Channel: medium Communication Process Flow of communication between a medical assistant and a patient THE SENDER… The one who initiates the message or communication. Puts the thought, idea, experience or act into a form that can be transmitted. THE MESSAGE… The thought, idea or expression from the sender. Often a dual message, verbal and nonverbal simultaneously. THE RECEIVER… The one to whom the message is sent. The receiver is prompted (by the message), to analyze, interpret and respond. THE FEEDBACK… COMMUNICATION CHALLENGES: •Educational/intellectual level: ex. medical terminology unfamiliar to patient •Psychological/Emotional: grief, anger, anxiety, perceptions, pride, financial concerns •Physiological: Impairments in cognition or hearing, age, sex , developmental stage •Culture/language barriers: •Stereotyping, prejudice, bias •Distractions: Attention, Environment, Hunger, Pain (Texting…where does it fit?) Be an active & critical listener •Be attentive •Ask questions •Concentrate •Avoid distractions •Take notes Strategies •Use reflections open ended questions statements to repeat back what you heard ex. “Mr. Wellness, you were saying that the new medication is making you vomit.” •Use paraphrasing use your own words to restate what you heard ex. “it sounds as if you are saying you do not want to take the medication anymore”. •Use open ended questions to gain further information (activity…open vs closed ended questions) Ex. “Can you describe the type of pain?” •Closed ended questions are necessary for times when specific information is required. Ex. “Are you in pain right now?” •Summarize organize the information they have communicated and check back for accuracy •Listen with an accepting attitude. •Use encouraging words that will invite them to continue on. "Mmm, hmm" "I see." "Right." “ Uh, huh." "Tell me more." "Sounds like you have some ideas on this." "I'm interested in what you have to say." "Let's talk about it." •Use nonverbal actions to show you are listening. relaxed posture head-nodding facial expression relaxed body expression eye contact •Use Silence is natural and sometimes appropriate in conversations NEGATIVE IMPACTs ON COMMUNICATION Giving an opinion Offering false reassurances Being defensive Showing approval or disapproval Stereotyping Asking why Changing the subject inappropriately Things to avoid while being an active listener •Do not interrupt. •Do not interrogate. Limit the number of questions you ask so that you are "drilling" them. •Do not try to think of your response in your own head while you are listening. •Do not change the subject. •Avoid phrases like: "Are you sure." "You shouldn't feel that way." "Its not that bad." “You're making something out of nothing." "Sleep on it. You'll feel better tomorrow." •Do not be judgmental … allow speaker to feel that they can communicate questions and ideas. NON-VERBAL COMMUNICATION What is the message for each? NON-VERBAL COMMUNICATION Includes: 1. Appearance 2. Kinesics or body movement Facial expressions Gestures Eye movement 3. Facial expressions 4.Posture & gait 5. Tone of voice 6. Touch Can create positive or negative feelings, Watch for nonverbal cues that show how the patient feels about being touched, Maintain proper personal space, position, & posture 7. Eye contact 8. Proxemics (personal space) Larger when talking to a stranger Becomes smaller the better you know someone Typically larger between two men than between two women Differs from culture to culture How are these a reflection of professionalism ????? Give an example of how non-verbal clues create misperceptions ????? NON-VERBAL COMMUNICATION may vary with culture Handout… What is the message for each? TIPS FOR MAKING SURE PATIENTS WITH LOW HEALTH LITERACY (patients' ability to understand their disease and how to manage their care) …GET THE APPROPRIATE MEDICAL INFO 1. Look for patients who need help: A patient can read and write with average skill and still not understand the language you use. 2. Avoid jargon: many well-intentioned physicians make the mistake of using technical terms, then trying to define them. (also remember most Americans read at an 8th grade level) 3. Use the “teach back” method: Avoid asking patients, "Do you understand?" most will say they do even when they are confused. Joanne Schwartzberg, MD, director of the AMA's department of geriatric health, suggested saying, "I want to make sure I did a good job teaching you. Tell me how you are going to do this when you get home.“ Ask them to repeat your instructions in their own words . 4. Avoid unnecessary details: …yet be specific when necessary. Address one problem or issue at a time, or on separate meetings 5. Use pictures: Illustrations often convey instructions better than words. (Sample pictogram s on next slide) 6. Enlist the aid of a family member or friend or translator Positive messages come from: · Attentiveness: Maintaining eye contact, looking relaxed, facing the speaker, nodding the head to show understanding without interrupting. · Voice and Facial Expression: Clear, strong voice volume, relaxed face with smile when appropriate, and minimal frowning. · Movement and Position: Don’t stand stiffly in one spot, sit down or move around with a relaxed stance, and use movement as an energizer. Silence: As a sign of effective listening, use silence after asking a question so people can think of their responses; don’t be afraid of silence. HAZARDOUS SUBSTANCE SYMBOLS Dynamics of Care in Society Written Communication for Health Care Professionals 42 Written communication “practical writing”… for a specific purpose, ex: Reports Business letters Interoffice memos Manuals Forms Applications Chart documentation “Practical Writing” Types Narrative writing…tells what happened, paragraph form, Descriptive writing…details of person, object, event Informative writing…giving directions, explaining how to, answering questions, making something easier to understand, use bullets or steps, Persuasive writing..giving an opinion or stating a point of view and supporting it with reasons in order to persuade the reader to accept or possibly take action on it Recording and Reporting Record patient information completely & precisely Record information only in secure & appropriate locations Record any action you take concerning a patient (“if it is not documented…it didn’t happen”) Just the facts… Minimize medical jargon (if for a patient) Drafting hints… Get started… get comfortable, be concise, have logical transitions of thought Outline ideas… organize before you write * brainstorm * group similar ideas together * find unifying themes * have a beginning, middle, end Revising…check for… * clarity * sentence & paragraph structure Proofreading… refinement…check for… * grammar, punctuation, spelling * final touches Tips for… “Well & Clearly Written” - create an outline to clarify and order your concepts - write a really bad first draft with no rewriting - rewrite, read out loud, rewrite, read again and rewrite - have colleagues comment on your draft - trust feedback from reviewers and rewrite again - let it sit, return for a fresh read out loud, and finalize Ideas for Learning to Write Better • Read examples you like and also review your colleague’s draft papers and edit them. • Take course in essay writing - good analysis, clear arguments and exposition, and convincing conclusions. • Write for broad audiences too - if you can capture them, you can capture professionals • Read your writing out loud and then edit! For Research Assistance… UCLA Library under services menu tab choose references & research help MEDICAL DOCUMENTATION Purposes of documentation in HC 1. Communication among the health care team 2. Assessment (vital signs, hx, symptoms…) 3. Quality Assurance (competence & quality of care) 4. Reimbursement (verification for insurances…) 5. Legal Record (admission of evidence) 6. Education (use for training) 7. Research: Useful Data Gained From Patient Records Examples: Nurse updates patient’s record with new info from patient Doctor sees nurse’s note & orders speech therapy consult to eval swallowing ability Pharmacist views medical history before filling prescription Discharge planner evaluates occupational therapist’s notes on progress in independence with ADL’s Advantages of Computerized Documentation Ease of access to data Multiple users simultaneously Different locations Various devices Easy storage & retrieval; faster recording of data Nearly unlimited file space Easy back-up for security Easy to add or attach info Improved legibility Safe Computer Recordkeeping 1. Don’t share passwords/computer signature 2. Don’t leave logged-on terminal unattended 3. Follow protocol for correcting errors 4. Allow only authorized personnel to create, change, or delete files 5. Back up records regularly 6. Don’t leave patient info displayed on monitor in view of others 7. Keep running log of electronic copies made of files 8. Never use unencrypted email to send protected health info 9. Follow confidentiality procedures for sensitive material What you’ll find in the medical record… Admission sheet – general demographic info, insurance info… Graphic sheet – for vital signs… Physician’s orders – for medications, instructions, procedures… Progress notes – on patient’s progress, new or changing info from each of the members of the health care team Medical history and exam – Allergies, Immunizations, Childhood diseases Current & past medications Previous illnesses, Surgeries, Hospitalizations Family medical history Reports – test results, lab results, consultations… Psycho-Social History Marital status Occupation Education Hobbies Diet Alcohol & tobacco use Sexual history Miscellaneous – correspondence, AD, organ donor… Good Medical Documentation Tips 1.It is accurate (ex. Correct spelling, Errors marked through, labeled with “error,” initialed, & dated…) 2.It is complete (ex. All supporting information – lab results …) 3.It is concise (ex. Only relevant information) 4.It is legible 5.It is organized (ex. Most recent information first, date stamped…) Progress Notes --- 3 Types 1. SOAP notes Subjective data Statements from patient describing condition Symptoms experienced Objective data Data that provider can measure, see, feel, or smell Test results Vital signs Assessment Patient’s diagnosis Possible disorders to be ruled out Plan Description of what should be done Diagnostic tests Treatments Follow-up 2. Charting by exception • • • • • • • • • Covers only significant or abnormal findings Decreased charting time Greater emphasis on significant data Easy retrieval of significant data Timely bedside charting Standardized assessment Greater interdisciplinary communication Better tracking of important patient responses More cost effective 3. Narrative Paragraph format Includes: Contact with patient What was done for patient Outcomes Can be time-consuming to write & difficult to read It is the oldest & least structured type Handout… PROPER TELEPHONE COMMUNICATION ANSWERING…. 1. ANSWER PROMPTLY 2. IDENTIFY SELF 3. FIND OUT WHO IS CALLING 4.SPEAK COURTEOUSLY, CLEARLY & PLEASANTLY 5. USE DISCRETION IN RELEASING INFORMATION, REMEMBER CONFIDENTIALITY 6. END CALL GRACEFULLY Handout… SCREENING…. 1. DON’T OFFEND CALLER 2. ASK WHO IS CALLING, NATURE OF BUSINESS OR EMERGENCY 3. ANSWER QUESTIONS TACTFULLY 4.ASK IF MESSAGE CAN BE LEFT 5. PLACE ON HOLD AND GET GUIDANCE, HELP IF NEEDED Handout… TAKING A MESSAGE…. 1. OBTAIN TIME, DATE, NAME OF CALLER , PURPOSE OF CALL 2. TAKE NOTES, REPEAT INFO BACK TO CALLER FOR ACCURACY 3. USE MESSAGE FORMS & FOLLOW THOUGH WITH PASSING MESSAGE TO CORRECT RECIPIENT. Handout… HANDLING COMPLAINTS…. 1. STAY CALM 2. GATHER INFO 3. BE SYMPATHETIC 4.OFFER TO FIND OUT WHAT CAN BE DONE 5. END CALL ON PLEASANT NOTE