Emergency Planning and Medical Response in the Mining Industry
advertisement

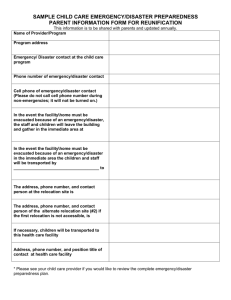
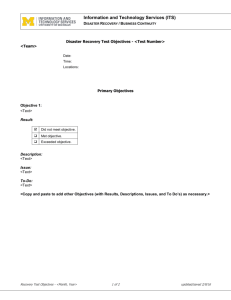
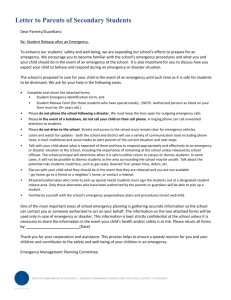
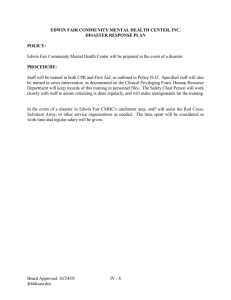
MINE MEDICAL PROFESSIONALS’ ASSOCIATION 14TH ANNUAL CONGRESS 20 – 22 May 2011 Emergency Preparedness presented by Mike Emmerich Nexus Medical Emergency Planning and Medical Response in the Mining Industry in South Africa Overview: • Fundamentals • Where we have come from? • What we currently have in place • What we need in place • Where too from here? • Strategies • References Fundamentals of Medical Incident Management •Every (medical) incident represents different challenges and nothing can replace “hands-on” experience/practice. What is an Incident? An event that could…. •Have (serious) financial impact. •Attract media, public and/or political attention. •Have the potential to cause personal injury, property and/or environmental damage. What is a Disaster? An event/incident that: •Extends your resources. •When normal community and organisational arrangements are overwhelmed •More than 1 patient could constitute a disaster. Phases of a Disaster •The Disaster Management Act of SA (No.57 of 2002) describes the following phases of a disaster: •Pre-Disaster Risk Reduction: •Prevention •Mitigation •Preparedness •Early Warning Phases of a Disaster •The Disaster Management Act of SA (No.57 of 2002) describes the following phases of a disaster: •Post-Disaster Risk Reduction: •Response •Recovery •Rehabilitation •Reconstruction Where Have We Come from? • Rescue teams have been around since the late 1920's • Specialised medical response teams only emerged post the Kloof Mine 1994 accident. • Training of Mine Medics was then formally started under the guidance of GFTS in 1996 and Nexus Medical was the subcontractor to GFTS from 1999 Where Have We Come from? • MRS took over the supervision in 2001 and it was still managed by Nexus Medical • In 2006 the College was formally accredited with the HPCSA until 2009 (with a contracted college principal) when MRS closed their college and stopped all medical training, due to HPCSA Pending resolutions. Where Have We Come from? Research/Legislation During this Period • SIMRAC 801 2001 and its follow up study scheduled for 2006 • Draft Guideline for the Compilation of a Mandatory COP on Emergency Medical Care and First Aid: 2008/04/18 • The Draft COP is based on the findings of the original SIMRAC 801 2001 report. What We Currently Have in Place: • No effective COP • Less than 200 BLS medics still in the system, with very few new medics being trained • No clear guidance from HPCSA re BLS training • No clear guidelines from industry leaders re Chamber, DME etc... • Individual mines seeking their own solutions. What We Currently Have in Place: • “Service Providers” offering cover at most mines, with many mines experiencing problems. • Mines now seeking solutions based on international best practice guidelines/standards/protocols. What We Currently Have in Place: • Service Providers” offering cover at most mines, with many mines experiencing problems. • A void exists in the training of BLS medics on the traditional short course training programmes. • Mines now seeking solutions based on international best practice guidelines/standards/protocols. What We Need in Place: • A working COP that covers new best practice international guidelines • A COP that articulates the thinking in current medical training and qualification terminology • Medics trained under an international standardised training programme • Medics who are both competent and can show “currency of competency”. Where too from here? • Industry standard protocols at the various levels of care (FA, BLS, ILS, ALS) at the pre-hospital and inhospital phase of care, including additional short course skills training for medical doctors (ITLS, ATLS, ACLS) Where too from here? • Medical Staff available both above and below ground • Skill levels on key treatment areas to be highlighted (as per guidelines in draft COP) • Appropriate equipment and drug therapies to be kept current with changes in ECC guidelines and other areas of patient care; eg: HCN in underground fires Where too from here? • Plan where medical teams, equipment are positioned (both above and below ground) as per guidelines from SIMRAC 801 re risk assessment. • Plan where medical stations and clinic are positioned above ground • Have clear “patient evacuation plans” with the relevant service providers, who are trained in the mining environment. Where too from here? • Dry run exercises of the entire rescue/extrication/treatment/transport continuum • From site of possible accident to last possible point of treatment • Continual alignment of protocols with international best practice benchmarking and research so as to remain current and competent. Strategies: • Dr William Haddon developed a framework by which we can identify interventions to address fatal mining injuries (Haddon, 1970). • By applying Haddon's theories - ten technical strategies for injury control and the targeting of interventions at the three phases of an injury event: pre-injury, injury, and post-injury (Robertson, 1992) • We can readily identify several interventions that may be useful in reducing the number of fatalities and injuries among South Africa's miners. Strategies: Haddon's ten technical strategies for injury prevention. (Haddon, 1972): 9. Begin to counter the damage already done by the environmental hazard: Locate emergency response teams closer to mining sites to expedite rescue efforts. 10. Stabilize, repair, and rehabilitate the object of the damage: Offer comprehensive medical and rehabilitative services to miners who experience non-fatal injuries. Example of “Prevention Strategies or Countermeasures” Strategies for Injury Prevention Move rapidly to detect and evaluate damage that has occurred and counter its continuation and extension. Action Train people in First Aid, with specific attention to entrapment Train medics (mine and service providers) in the acute care of entrapped patients Stabilize, repair, and rehabilitate Develop a standardised trauma the damaged object. management and treatment system. Be Proactive! •Plan ahead – Disaster/Incident Management Plan •Be prepared: Design a ERP •Do a Risk Assessment •Incident Management Plan •Emergency Management Plan •Appropriate training and testing. Proactive not reactive Closing Comments: • We need to fast track the finalisation of an EMS COP • The various industry role players need to be more vocal in the obvious shortfalls in the current system • If need be we must look outside the current programmes and go beyond our borders for best practice international programmes. • The longer we wait the fewer medics there will be left in the system! For more information please contact: Mike Emmerich CCA-ALS, ACLS-EP, PALS, ATLS, ITLS, FMA, AMR eACLS, ACLS, ITLS, PALS & AT&T Instructor ESCI Instructor Advanced Life Support Paramedic 082-557-1870 www.nexusmedical.co.za mike@nexusmedical.co.za nexusmedical@iafrica.com