Title Slide Arial 40pt Bold w/shadow goldenrod
advertisement

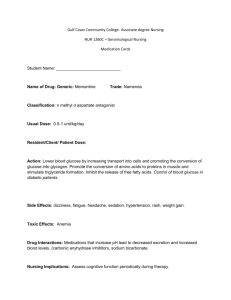
Utilizing Technology for Optimal Control CGMS® System™ and Bolus Wizard Calculator Bruce W Bode, MD FACE Atlanta Diabetes Associates Steps to Quality Care Gather Information Refine Treatment Complete Assessment Limitations of Conventional Testing • Blood glucose monitoring – Limited data points – incomplete picture – Fails to detect asymptomatic hypoglycemic episodes – Data collection and logging problems – Susceptible to inaccurate results • A1C blood test: 90-day averaging – Does not identify a patient’s wide blood glucose excursions Daily Patient Log 400 350 Glucose (mg/dl) 300 250 200 150 Target Range 100 Fingerstick Measurement Insulin Bolus 50 0 Dinner Breakfast Lunch 8:30 am 12:00 noon 6:00 p.m. Bedtime 10:30 p.m. Daily Patient Log and Sensor Data 400 350 Glucose (mg/dl) 300 Fingerstick Measurement Sensor Measurement 250 200 150 Target Range 100 50 Insulin Bolus 0 BreakfastLunch Dinner Bedtime 8:30 a.m. 12:00 noon 6:00 p.m. 10:30 p.m. Benefits of Continuous Glucose Monitoring • Supplements A1C and SMBG information • Can identify post prandial glucose excursions • Can identify undetected nocturnal hypoglycemia • Helpful visual patient teaching tool GlucoWatch® Biographer ® CGMS System • • • • Sensor Monitor Sen-serter® CGMS® system Solutions Software • Com-Station TM TM 1-90 The Sensor • • • • • Tiny, flexible, sterile Inserted just under the skin Disposable 24 to 72-hour usable life Sends measurement signal to monitor every 10 seconds • Measures glucose values within the range of 40-400 mg/dl (2.2 mmol/l) The Sen-serter ® • Makes insertion virtually painless • Helps give insertions consistent depth and angle • Design is similar to insertion devices available for insulin pump disposables The Monitor • Connected to the sensor via a small, flexible cable • Worn like a pager • Records an averaged glucose value every 5 minutes (up to 288 per day) • Also records meals, exercise or other events entered by patient • Holter-style monitor The Com-Station and ® CGMS System Solutions Software TM TM • Com-Station — — Downloads data from monitor to software Downloads meter data and Medtronic MiniMed pump data • Software — Converts stored sensor data into easy-to-use reports, graphs and charts — Saves data in individual patient files — Included with CGMS® System GoldTM and runs on standard PC platforms Calibration Measurement Range 40-400 mg/dl Sensor Signal • Patient enters 3 or more blood glucose values per day • Sensor glucose data is calibrated based on blood glucose values • Patient enters event markers for meals, insulin, … Blood Glucose Conc. CGMS System Reports ® • Sensor Summary • Sensor Daily Details • Sensor Modal Day • Sensor Modal Time Periods Sensor Modal Day Report Glucose Excursion Statistics & Charts • Definition: — # and total duration of glucose values above, within and below target glucose ranges (statistics and pie charts) • Benefit: — Familiar statistical means of analyzing time spent out of the target range in a simple to understand format Statistics: Glucose Area Above/ Below Target Limit • Definition: —Area between the sensor tracing and the target glucose line (mg/dl*day); also known as Area Under the Curve (AUC). • Benefit: —More complete statistical means of analyzing the extent and duration of glucose excursions Glucose Area Above Target Limit AUC= 30 mg/dl*days 230 Modal Meal and Time Range Blocks Definition: Averages and ranges for pre/post meal and other identified time periods (statistics and graphing on separate report) Benefits: Clear identification of the glycemic impact of marked events Ability to analyze all meal periods and any overnight and early morning time periods separately Modal Meal and Time Range Blocks Modal Meal and Time Range Blocks Patient Role in CGMS • Attends office visit for sensor placement and to learn sensor use • Wears each sensor for one to three days • Enters at least four BG per day • Enters event markers • Keeps detailed diabetes care log sheet • Protects monitor and sensor site Pearls for Interpretation • What is the goal of the sensor “run” —Lower A1C —Lower the risk of Hypoglycemia —Safety • Look for trends —Fasting state —Postprandial —Treatment of highs/ lows/ exercise • Review Log —MUST have detail of events, meals, medication, exercise (duration, intensity, type), Rx of highs and lows Case Study # 1 • DC, female, age 50 • Type 1 X 40 years, A1C 7.1% • CSII basal rate: 0.8 u/hr for 24 hours • Insulin:Carb ratio = 1.0 u : 15 grams • Correction Factor: BG-100 divided by 50 • History of frequent, severe hypoglycemia • CGMS done to determine pattern of lows and reduce/ eliminate them Modal Day View Sensor Daily Details- Day #3 “STRESSFUL DAY – 0.8 u 209 Bad Hair Day” 3.3 u 252 2u 109 22 toast, jelly toast, jelly, 97 gm gms Choc milk milk 97 42 choc 5u 63 1 cup hamburger helper, 1 can Sprite, no bolus 135 Case Study #2 • MG, age 37 • Type 1 X 18 years • History of volatile BG’s, unexplained hypoglycemia with increasing hypo unawareness; A1C = 5.6% • CSII basal rates: 12 am - 0.6 u/hr; 2pm - 0.5 u/hr; 7pm - 0.6 u/hr • Insulin : Carb ratio = 1u : 20 grams • Correction Factor: BG- 120 divided by 70 • CGMS done to determine patterns overall & gain insight into patterns of lows Modal Day Sensor Daily Details- Day #2 1.5u 4oz juice 2u Meter BG not entered 2 toast + jelly, yogurt; 0 insulin 22 CHO Meter BG not entered; stop bolus; 8 oz. OJ 40 gm, 0.5u, 1u / 2 hrs Sensor Daily Details- Day #3 Meter BG not entered 12 grapes+ 1 plum; o insulin taco salad; 1.1u 2 toast + peanut butter Meter BG not entered; 1u 1u then 0.5 X 1 hour 2 .4 u tootsie rolls 2 sl veggie pizza; 1u then 2u 12 grapes Case Study # 3 • • • • GL, male, age 39 Type 1 X 8 years A1C= 7%; recent increase from 6% CSII basal rates: 12 am - 1.0 u/hr ; 4:30 am - 1.6 u/hr; 11:30 - 1.0 u/hr • Insulin: carbohydrate ratio =1u : 10 grams • Correction Factor: BG- 100 divided by 40 • CGMS done to assist with improving overall glycemic control Modal Day View Milk choc 15g; 8u Cheese / Crackers 20 g; 3units 6u Ice Cream; 3 u 2u; 57 g CHO Juice box; no insulin 80 CHO; 7u 30 gm CHO; Heavy Exercise Case 4: 40 year old nurse wore sensor for CGMS Training purposes 300 200 100 October 2000 Clinical Information Normal A1C Normal lab fasting BG Laboratory Confirmed elevated post prandial BG Family history of type 2 diabetes Patient with PCOS Mild background retinopathy on screening ophthalmology exam 2 months later After 10 kg weight loss Exercise program initiated Lower carb, higher fiber diet Update 2002: on metformin has regained Some weight, but not all CGMS Resulting Therapy Adjustments 58% Increase Meal Bolus Decrease Basal Insulin 49% Change Method of Counting Carbs 49% 30% Increase Basal Insulin 30% Change Treatment of Hypoglycemia 24% Change Treatment of Hyperglycemia Change from Regular to Lispro Decrease Meal Bolus 0% 15% 12% 20% 40% Percent of Patients (N=33) Sabbah H: Diabetes 49(suppl. 1):718, 2000 60% 80% Reasons to Use CGMS • Improve glycemic control • Reduce risk of hypoglycemic events Fine-Tuning Pump Therapy Using the Bolus Wizard Calculator Targeting Insulin Dosing What must be known: • Target BG • Current BG • Anticipated CHO intake • Insulin : CHO ratio • Correction factor Most common bolusing errors • Under-estimation of carbohydrates consumed (CHO bolus) • Over-correction of post-prandial elevations (CF bolus) — Remaining unused, active insulin — Stacking of boluses Bolus: Source of Errors • “Inability” to count carbs correctly — Lack of knowledge, skill — Lack of time — Too much work • Incorrect use of SMBG number • Incorrect math in calculation • “WAG” estimations Using the Bolus Wizard™ Calculator with the Paradigm Link™ Monitor Paradigm 512™ Paradigm Link™ • Monitor sends BG value to pump via radio waves • Carbohydrate intake is entered by patient • “Bolus Wizard” calculates a suggested insulin dose using personal settings The Bolus Wizard™ Calculator • Can be customized with up to 8 different setting per day for: —Blood glucose targets —Carbohydrate ratios —Insulin-sensitivity factors • Simplifies Diabetes Management —May reduce math errors —Decreases the number of correction boluses required* —Lowers the entry error rate when using the Paradigm LinkTM Blood Glucose Monitor, powered by BD LogicTM Technology How to Utilize The Bolus Wizard Feature Paradigm® Pump MiniMed Main Menu Press ACT Bolus Bolus Bolus • Opens Main Menu Suspend Suspend Basal Basal Prime Prime Utilities Utilities Optional Feature May be turned ON or OFF How to Utilize The Bolus Wizard Feature Paradigm® Pump MiniMed Bolus Menu Set Bolus Bolus History Bolus BolusWizard WizardSet SetUp Up Max Bolus Dual/Square Bolus Easy Bolus BG Reminder How to Utilize The Bolus Wizard Feature MiniMed MiniMed WIZARD SETUP Edit Settings EditSettings Settings Edit ReviewSettings Settings Review Wizard: MiniMed Carb units: Review Settings Carb CarbRatios: Ratios: BG Units: Carb Ratios: 12:00 A 10 11:30 A 12 6:00 P 15 Sensitivity: BG Targets: off on exchanges grams May set different ratios10 for B:L:D: + mg/dL mmol/L Up to 8 50 different SF & BG Targets 100 in 24 hrs. Example 1 Consider Robin Smith: Parameters to enter into pump: Target BG Carb Ratio Correction Factor 100 10 50 Breakfast - Step 1. Check BG • The Paradigm system automatically sends Blood Glucose readings from the Link Monitor (powered by BD Logic™ Technology) to the pump • Otherwise, the patient enters in the Blood Glucose reading into the pump after testing Breakfast - Step 2. Accept BG • Robin accepts the transferred blood glucose value —Requires confirmation —Can change glucose value if necessary • Enters CHO grams —53 grams of carbohydrate Breakfast - Step 3. Accept Dose • The dose estimate is displayed —5.3 U for 53 grams carb (CIR = 10) —No correction dose —Shows total 5.3 U • Accept suggested dose • Pump delivers dose Late Lunch - Step 1,2 • Robin has a late lunch at 2:10 PM — Blood glucose 160 — Accepts the transferred BG value • Enters CHO grams — 50 grams of carbohydrate 50 Late Lunch - Step 3. Accept Dose • The dose estimate is displayed —5.0 U for 50 grams carb (CIR = 10) —Correction dose = 1.2 U (160-100) / 50 = 60/50 = 1.2 —Shows total 6.2 U • Accept suggested dose • Pump delivers dose Early Supper - Step 1,2 • Robin plans to have appetizers at 5:30 PM — This is only 3.5 hours after lunch. — There is still an active insulin depot — Blood glucose is 157 — Accepts the transferred BG value • Enters CHO grams —50 grams of carbohydrate 50 Early Supper - Step 3. Accept Dose • The dose estimate is displayed — 5.0 U for 50 grams carb (CIR = 10) — Correction dose = 1.1 U (157 -100)/50 — Remaining active insulin = 2.6 U — Remaining active insulin > correction dose — No correction dose is recommended — Total shows 5.0 U • Accept dose • Pump delivers dose Summary • Utilizing technology can help you to optimize therapy with your patients with diabetes. • CGMS System Gold can identify high and low BG levels undetected by traditional methods • New pump features like the Bolus Wizard Calculator can help fine tune pump therapy for better post prandial control