A Practical Guide to Clinical
Medicine
A comprehensive physical examination and clinical education site for medical students and
other health care professionals
Web Site Design by Jan Thompson, Program Representative, UCSD School of Medicine;
Content and Photographs by Charlie Goldberg, M.D., UCSD School of Medicine and VA
Medical Center, San Diego, California 92093-0611.
Introduction
History of Present Illness
The Rest of the History
Vital Signs
The Eye Exam
Head and Neck Exam
The Lung Exam
Exam of the Heart
Exam of the Abdomen
Breast Exam
Male Genital/Rectal Exam
The Upper Extremities
The Lower Extremities
Musculo-Skeletal Exam
The Mental Status Exam
The Neurological Exam
Putting It All Together
Medical Links
Write Ups
The Oral Presentation
Outpatient Clinics
Inpatient Medicine
Clinical Decision Making
Commonly Used Abbreviations
A Few Thoughts
References
Send Comments to: Charlie Goldberg, M.D.
The "daVinci Anatomy Icon" denotes a link to related gross anatomy pictures.
Male Genital And Rectal Exam
Preparing and Positioning the Patient:
This is generally the last part of the complete physical examination. While it may cause the
patient (and perhaps you) some embarrassment as well as discomfort, it provides important
information and should not be skipped. Explain to the patient what you are going to do (and
why) and then proceed.
If they have not already done so, ask the patient to remove their underwear. I believe that
this examination is easier to perform and yields more information if it is done with the
patient standing while you are seated in front of them. In this position, it is easier to
examine the testes, evaluate for inguinal hernias and perform the rectal exam. However, if
the patient is unable to stand/unsteady on their feet, it can be performed while they lie on
the exam table.
The Genital Exam:
Have the patient stand in front of you and raise their gown to the level of the umbillicus,
exposing the entire genital region. Put on a pair of gloves prior to beginning. The gloves do
not have to be sterile.
Observation:
1. Note if there are any bulges or scars in the inguinal region, consistent with current
or past hernias.
2. Any obvious penile or scrotal abnormalities?
3. Any obvious skin abnormalities on the penis, scrotum or surrounding areas?
The Penis:
1. First examine the glans (i.e. the head) of the penis. If the patient is uncircumcised,
draw back the foreskin so that you can look at the glans in its entirety. Make sure
that you return the foreskin to its normal position at the end of the exam, else it can
cause severe venous and arterial obstruction, leading to necrosis of the head of the
penis, a condition referred to as paraphymosis. Occasionally you will be unable to
retract the foreskin from the head of the penis, referred to as phymosis.
Paraphymosis: Picture on left demonstrates edematous foreskin which has become
trapped behind
the head of the penis. Picture on right demonstrates foreskin in appropriate position
covering head of penis.
This was achieved by applying steady pressure to the head of the penis, reducing
edema, which then
allowed repositioning of foreskin. Note that patient has Foley catheter inserted.
Phymosis: Scarred down foreskin which can not be retracted over head of penis.
2. Look at the opening of the urethra. Make note of whether it is more or less at the tip
of the penis, on the top-side (known as epispadias) or on the bottom-side
(hypospadias). Check for any obvious milky discharge suggestive of urethritis, a
condition most commonly caused by the sexually transmitted diseases Gonorrhea
and Chlamydia.
3. Feel along the shaft of the penis. Are there any underlying firm areas? Any unusual
curvature to the normally straight penis? Occasionally, fibrosis occurs along the
shaft, which causes palpable plaques and penile curvature.
4. Examine at the base of the penis/amidst the pubic hair for any skin abnormalities
(e.g. pigmented areas, ulcers, vessicles etc.). You will obviously look harder if the
patient complains of seeing/feeling something in that region.
Penile Condyloma: Growth at edge of
glans due to HPV infection.
Syphilitic Ulcer
5.
HSV Vessicles
Testicular Exam:
1. In general, the left testis lies a bit lower in the scrotum then the right. The testes
should appear as 2 discrete swellings, although if the room is particularly cold, they
may retract a bit up towards the inguinal canal (more of problem in pediatric then
adult medicine).
2. Gently feel the testes, palpating the tissue between the thumb and next 2 fingers of
your examining hand. Each should be of the same consistency and size. If there is a
significant size discrepancy (or complete absence of one of the testes) ask the
patient if this has always been the case. They may have had one surgically
removed� or perhaps suffer from a congenitally undescended testis. The patient
should be able to relate whether he was ever able to feel both testes or if anyone has
ever told him that he has a testicular abnormality. If there appears to be a single
testis, carefully examine the inguinal canal (see below) for evidence of a discrete
swelling that could represent the location of an undescended testis. Make careful
note of any discrete lumps or bumps within the body of the testis. The presence of a
firm nodule would be worrisome for testicular malignancy. Occasionally, the entire
testis feels enlarged. This is most commonly caused by a hydrocele, which is a
collection of fluid that fills a potential space surrounding the testis. Hydroceles have
a characteristic texture that is different from that of testicular tissue. You can also
distinguish them from the body of the testis by trans-illumination. To do this, shut
off the lights in the exam room and place a flash light on the scrotum, directly over
the area in question. A hydrocele will allow the transmission of light, while
testicular tissue will not.
Testicular enlargement caused by hydrocele.
Orchitis: Picture on left demonstrates testicular enlargement caused by infection
within the body of the testis.
The inflammation has spread from the testis to the skin of the scrotum, with
resulting edema causing fewer skin folds over the right testicle compared with the
left. No transillumination is seen (picture on right) as the inflamed testis does not
allow the passage of light (as opposed to hydrocele shown above, which readily
conducts light). This is not always the case, as sometimes orchitis will cause a
"reactive hydrocele" to form, which will transilluminate.
3. The epididymis is a discrete structure which lies towards the top and back of each
testis.
4. If there is any testicular pain, it may be easier to perform the exam while the patient
is supine.
Gross anatomy of the normal testis.
Diagram of male genital anatomy.
Assessment of the spermatic cord structures:
1. The vas deferens, testicular artery/vein, ilio-inguinal nerve, lymphatics and fatty
tissue make up the spermatic cord, a structure that runs from the epididymis up
through the inguinal canal. The vas can be distinguished from the rest of these
stuctures as it lies along the posterior aspect of the bundle and feels firm and wirelike. You will normally be unable to specifically identify the remaining structures.
2. Identify any discrete swellings within this collection of tissues. If present, note their
relationship to the testes and inguinal canal. Dilated veins, referred to as a
varicocele (feels like a bag of worms� really!), will be palpable throughout the
length of the cord structures.
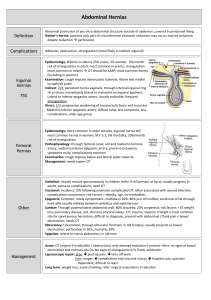
Evaluation for inguinal hernias:
1. If you detect a diffuse swelling amidst the cord structures or note the inguinal canal
area to be protuberant, the patient probably has an inguinal hernia. The following
examination, however, should be performed on all male patients, regardless of
whether you suspect any underlying abnormality. Before palpating this region, have
the patient bear down (i.e. valsalva) or cough (though have them turn their heads
first so they don't expectorate into your hair) while you look at the inguinal region.
Both of these maneuvers increase intra-abdominal pressure, forcing
intestines/omentum/peritoneal fluid through any defect which may exist and making
a hernia more apparent.
Right Inguinal Hernia
2. If you are examining the right inguinal region, place the index finger of your right
hand along the spermatic cord, inverting the scrotal skin as you trace the cord to
where it emerges from the external ring of the inguinal canal. You may be able to
put the tip of your finger into this narrow opening. Put the fingers of your left hand
over the inguinal canal, which runs obliquely towards the patient's anterior-superior
iliac crest, or on top of any noticeably swollen area. Have the patient repeat the
above maneuvers that increase intra-abdominal pressure and note if you can feel,
with either hand, any bulging tissue that would be consistent with a hernia.
Hernia Exam
3. Exam of the left inguinal area is done in the same way, though hand positioning is
reversed. Hernias are generally non-tender and there should be no evidence of acute
inflammation (i.e. skin edema or redness). If present, it suggests
incarceration/strangulation of the entrapped contents, the most dreaded
complication of a hernia, and constitutes a surgical emergency.
4. Inguinal hernias come in all sizes. Distinguishing direct from indirect hernias on the
basis of exam is rather difficult and not clinically important as both should generally
be repaired and the final determination can be made at the time of surgery. Some
hernias will be barely palpable by the index finger placed in the external ring of the
inguinal canal. Others can be quite massive. In this setting, it may be difficult to
distinguish the cord structures or testis from the contents of the hernia, though give
it a try. The testis should be located at the bottom of the scrotum.
Large right inguinal hernia: Prominently seen in picture on left. Picture on right
demonstrates appearance in same patient after manual reduction.
5. Auscultation on top of a hernia may allow the detection of bowel sounds, which can
be useful information if you are unsure as to the nature of an inguinal bulge.
6. In the event that the patient is unable to stand, the above examination can be
performed as described with the patient supine. This may actually be a better
position for evaluating the inguinal canal if you are concerned that it may contain a
discrete mass, as in the case of a suspected undescended testicle.
Rectal/Prostate Exams:
Have the patient turn around and instruct them to rest their chest on the exam table. This
gives you an opportunity to perform the exam while providing the patient with something
to lean against for support. You can remain seated. Separate the cheeks of the buttocks and
look at the peri-anal area. Make note of any skin abnormalities, bleeding sites, fissures or
hemerrhoids.
Thrombosed External
Hemerrhoid
Prolapsed Internal
Hermerrhoid
Rectal Fissure and
Prominent Skin Tag
The digital rectal exam can provide information about several important organ systems,
including:
1. Gross inspection of the stool. Is there obvious evidence of blood, which generally
implies that the bleeding site is close to the anus? Does the stool appear black/tarry,
which occurs when blood released from an upper intestinal source is digested and
passed thru the entire alimentary canal? In such cases it will also have a
characteristic odor. Normal appearing stool should be tested with a special agent
designed to detect hemoglobin (see below). This is referred to as checking for occult
blood (i.e. blood that would not otherwise be identifiable). In these cases, the source
of bleeding is most frequently within the colon, although it can be from anywhere in
the GI tract.
2. Palpation upwards, posteriorly, and laterally will allow you to feel for rectal based
masses.
3. Feeling anteriorly will allow you to examine the prostate gland.
Before proceeding, provide the patient with a box of tissue paper that they can use for
cleaning themselves at the end of the exam. Open a stool guiac card and place it on the
exam table next to the patient. Then:
1. Put a lot of lubricant (a.k.a. surgi-lube) on the index finger of your right hand.
2. Tell the patient that you are going to place your finger in their rectum. Remember,
this is a delicate aspect of the exam, and the patient often feels quite vulnerable.
Thus, it's a good idea to talk them through each step.
3. Place your well lubricated index finger against their anus, but do not yet insert it
into the rectum.
4. Ask the patient to bear down as if they are trying to have a bowel movement. This
helps to relax their external sphincter and should decrease discomfort. As they bears
down, gently push forward until you have placed the entire finger within the anal
canal. Pay attention to the following:
5. As your finger enters, make note if you hit any resistance. You may run into some
stool, which should easily move out of the way. A mass (e.g. a large rectal tumor)
will not move. If this occurs, do not force your finger forward.
6. By gently rotating your hand, you can use the pad of your index finger to feel to the
left, right and then directly backwards (i.e. towards yourself) and along the sacrum.
Make note of any irregularities/masses. What you encounter will vary with the
clinical situation. You might, for example, feel a fluctuant collection in a patient
with a pelvic abscess associated with a perforated appendix.
7. Orient your finger so that it is directed anteriorly (i.e. toward the patient's
umbillicus). It should now be resting on the prostate gland, which is palpated
through the wall of the rectum. Make note of the following:
a. The prostate has two lobes with a cleft running between them. Can you feel
each lobe distinctly? Do they feel symmetric? Are their any discretely firm
areas (referred to as nodules)? Normal prostatic tissue feels more or less like
the tip of your nose. Anything firmer is suspicious for malignancy. If you
feel a firm area, check and see if the prostate is freely mobile or if it feels
fixed to the pelvis, which can occur via direct extension of a malignancy.
b. Does the prostate gland feel big? You will obviously have no idea until you
have had an opportunity to examine many to get a sense of the range of
normal. In general you should be able to get you finger over the top of the
gland. This may be difficult if:
the patient is obese/has large glutteal cheeks,
you have small fingers
they have a big prostate
Do the best that you can. One helpful way of trying to feel the full extent of
the prostate is to make sure that the patient is leaning over the exam table,
which has the effect of directing the prostate out towards you. Then take
your left arm and wrap it around their waist, enabling you to draw the
patient towards you as you push with your examining finger.
c. Any pain on palpation, which is suggestive of prostatic infection? Does the
gland feel swollen? Again, this is a very subjective finding which is only
apparent after examining many normal prostates. It occurs in the setting of
infection. Try to have the patient distinguish between the discomfort of the
exam in general from any pain specifically produced by pushing on the
prostate.
8. Assessment of rectal tone. This can be done either at the beginning or the end of the
examination. In certain diseases of the central or peripheral nervous system,
innervation of the sphincters that help maintain rectal continence may be affected
(e.g. in the setting of sacral nerve root compression associated with a tumor) and
muscular tone can be diminished or absent. There is a certain subjective tightness
that you will notice when you enter the rectum with your finger. You can further
assess external sphincter tone by asking the patient to try to hold on to your finger
with their rectum (granted, this is an odd request), allowing you to feel the
contraction of this muscle.
9. Exam of the stool. There is usually some stool in the rectal vault that will coat your
finger at the end of the exam. Inspect it after you withdraw your hand, looking for
red or digested blood as described above. Take the stool guiac card that you have
placed on the table prior to beginning the exam and put a small smear of stool in
each of the windows. Then turn the card over and open the back. Place a drop of
developer on the back side of each window as well as over the control spot. The
control will turn blue, the color indicating hidden hemoglobin. If you are having a
difficult time convincing yourself that there is truly some blue present within the
specimen, take the card and hold it up so that light passes through the windows,
accentuating any color changes.
Guaiac Testing Equipment
Guaiac Positive (Note blue coloration in boxes)
As you are evaluating the stool, allow the patient to wipe themselves off with the tissue
paper that you made available to them earlier. It is generally a nice idea to pull the curtain
and give them some privacy while they clean up and dress. To remove your stool-covered
glove, take the index finger of your left hand (which should still be clean) and place it
under the cuff of the right glove. Then pull that glove down towards your fingers, inverting
it in the process.
In the event that the patient cannot stand, this examination can be performed with the
patient lying on the exam table. Place them on their side, with knees tucked up towards
their chest. Their back should be as close to the edge of the table (i.e. as close to you) as
possible. The remainder of the exam is performed as described above. You may either sit or
stand.
home | Clinical Images | Curricular Resources | For Our Students | BioMed Library | Web Resources | SOM 201 (ICM) Course | Next
Copyright ©1997-2008, The Regents of the University of California.
All rights reserved. Last updated 8/16/2008.