Revision History - (S&I) Framework
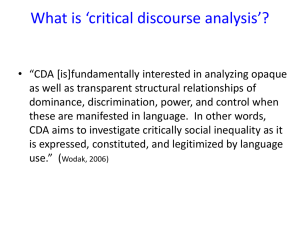
advertisement

U.S. Health and Human Services Office of the National Coordinator for Health IT Standards & Interoperability Framework Transitions of Care Initiative Discharge Instructions Implementation Guidance Version 2.0 November 15, 2011 Office of the National Coordinator for Health Information Technology Revision History Date Document Version 8/13/2011 1.0 Initial draft of Discharge Instructions Implementation Guidance, intended to serve as an implementation primer for potential pilot participants 2.0 Version 2 of the Discharge Instructions Implementation Guidance is now available for public review, and focuses on specific improvements in assisting implementers with care transition information exchanges: Alignment of CDA to CIM Full designation of applicable value sets High level constraints applied to each CDA Section Additional split out of Care Transition Information Exchanges into individual guidance documents Expanded tooling support now available within MDHT 11/15/2011 Document Revision Description Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 2 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Table of Contents 1. Introduction ..................................................................................................................................................... 5 Purpose ...........................................................................................................................................................5 Scope ...............................................................................................................................................................5 1.2.1 Use Case Scenarios .............................................................................................................................6 1.2.2 Information Exchanges .......................................................................................................................6 Audience..........................................................................................................................................................6 Organization of This Guide ..............................................................................................................................7 Templates ........................................................................................................................................................7 Conformance ...................................................................................................................................................7 Conventions.....................................................................................................................................................7 Section Preamble ............................................................................................................................................7 1.8.1 CDA Implementation Table .................................................................................................................8 1.8.2 Implementer Notes .............................................................................................................................8 2. Discharge Instructions Implementation Guidance ............................................................................................ 9 CDA Header Information .................................................................................................................................9 2.1.1 Contact Information .........................................................................................................................10 2.1.2 Person Information ...........................................................................................................................11 2.1.3 Provider Information ........................................................................................................................12 Discharge Instructions ...................................................................................................................................13 2.2.1 Advance Directives Section ...............................................................................................................14 2.2.2 Allergies, Adverse Reactions, and Alerts Section ..............................................................................15 2.2.3 Hospital Discharge Medications Section ...........................................................................................16 2.2.4 Immunizations Section .....................................................................................................................17 2.2.5 Plan of Care Section ..........................................................................................................................18 2.2.6 Problem List Section .........................................................................................................................19 2.2.7 Medical Equipment Section ..............................................................................................................20 3. TOC Clinical Information Model (CIM) ............................................................................................................ 21 ToC CIM Objects ............................................................................................................................................21 4. Additional Guidance for Implementers and Vendors ...................................................................................... 25 Tools ..............................................................................................................................................................25 4.1.1 OHT/MDHT .......................................................................................................................................25 4.1.2 Trifolia ...............................................................................................................................................25 4.1.3 NIST Validation/MU testing sites ......................................................................................................26 4.1.4 TOC Quickstart Site ...........................................................................................................................26 4.1.5 myCDA ..............................................................................................................................................26 Educational Resources ..................................................................................................................................26 4.2.1 Clinical Document Architecture (CDA) ..............................................................................................26 4.2.1.1 HL7 Structured Documents Technical Committee Wiki ...................................................26 5. Appendix A – Reference Documents ............................................................................................................... 27 6. Appendix B – Acronym List ............................................................................................................................. 28 7. Appendix C – Recommended Value Sets ......................................................................................................... 29 Advance Directive Type Recommended Value Set........................................................................................29 Allergy/Adverse Event Food and Other Allergens Value Set .........................................................................30 Allergy/Adverse Event Reaction Value Set ....................................................................................................30 Allergy/Adverse Event Type Value Set ..........................................................................................................30 Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 3 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Care Transition – Body Site Value Set ...........................................................................................................30 Care Transition – Contact Type Value Set .....................................................................................................31 Care Transition – Country Value Set .............................................................................................................31 Care Transition – Medication Brand Name Value Set ...................................................................................31 Care Transition - Medication Clinical Drug Name Value Set .........................................................................31 Care Transition - Medication Drug Class Value Set .......................................................................................32 Care Transition – Patient Class Value Set ......................................................................................................32 Care Transition – Postal Code Value Set .......................................................................................................32 Care Transition - Problem Value Set .............................................................................................................33 Care Transition – Provider Role Value Set .....................................................................................................39 Care Transition – Provider Type Value Set ....................................................................................................40 Care Transition – Relationship Value Set ......................................................................................................41 Care Transition - Severity Value Set ..............................................................................................................42 Care Transition – State Value Set ..................................................................................................................42 Health Insurance Subscriber Relationship Value Set.....................................................................................42 Health Insurance Type Value Set ...................................................................................................................43 Ingredient Name Value Set ...........................................................................................................................44 Immunizations Administered Vaccines Value Set Recommendation............................................................44 Immunization Reason Value Set ....................................................................................................................46 Medication Fill Status Value Set ....................................................................................................................47 Medication Method of Delivery Value Set ....................................................................................................47 Medication Product Form Value Set .............................................................................................................47 Medication Route Value Set ..........................................................................................................................47 Medication Type Value Set ............................................................................................................................48 Problem Status Value Set ..............................................................................................................................48 Problem Type Value Set ................................................................................................................................48 8. Appendix D – XML Samples for Discharge Instructions ................................................................................... 49 Sample CDA Header XML Schema .................................................................................................................49 Sample RecordTarget XML Schema ...............................................................................................................49 Sample Author XML Schema .........................................................................................................................50 Sample Informant XML Schema ....................................................................................................................50 Sample Custodian XML Schema ....................................................................................................................51 Sample Participant XML Schema ...................................................................................................................51 Sample DocumentationOf XML Schema .......................................................................................................52 Sample Advance Directives XML Schema ......................................................................................................53 Sample Allergy XML Schema .........................................................................................................................54 Sample Problems XML Schema .....................................................................................................................55 Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 4 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 1. Introduction In support of the national objectives for healthcare reform, the Office of the National Coordinator for Health Information Technology (ONC) Standards and Interoperability (S&I) Framework has sponsored the development of harmonized interoperability specifications. These specifications are designed to support national health initiatives and healthcare priorities, including Meaningful Use, the Nationwide Health Information Network, and the ongoing mission to improve population health. The S&I Framework is comprised of several initiatives, each focusing on a single challenge with a set of valuecreating goals and outcomes to enhance the efficiency and effectiveness of healthcare delivery. Among the first initiatives launched by the S&I Framework is the Transitions of Care (ToC) Initiative, which focuses on improving the exchange of core clinical information among providers, patients, and other authorized entities in support of Meaningful Use for the improvement of patient care. The S&I Framework Transitions of Care initiative identified core information to be exchanged in the following scenarios: 1. 2. When a patient transfers between healthcare providers When electronic clinical information is shared from providers to patients. The Transition of Care information exchanges are accomplished using the recommended Clinical Document Architecture (CDA) interchange standard developed by Health Level Seven (HL7). This implementation guidance is provided to assist the implementation community in their efforts to quickly access the numerous resources available as well as provide practical guidance that is outside the scope of the HL7 balloted standards. Purpose This implementation guide enables the exchange of key clinical information among providers in the instance of a transition of patient care. Adopting and implementing transition of care standards provides the following benefits: 1. Establishes a common standard for the exchange of clinical information. By adherence to a common semantic model, the standard provides semantically consistent information across instances of exchange. 2. Implementation of the clinical constructs defined by the Transitions of Care Initiative ensures compliance with the following Meaningful Use criteria: Electronic Copy of Health Information, Electronic Copy of Discharge Instructions, and Clinical Summary for each Office Visit. 3. Facilitates the ease of adoption of Meaningful Use 1 and anticipated Stage 2 for which eligible providers receive a monetary incentive. Scope The scope of the transition of patient care is defined in the use case as two scenarios, both supported by key outputs or constructs that contain specific patient information to facilitate the exchange of information in the event of a care transition. Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 5 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 1.2.1 Use Case Scenarios Scenario 1: The Transfer of Patient Information from One Provider to Another Actor: The transfer of patient information from one provider to another actor occurs in two ways: 1. 2. The exchange of Discharge Instructions and Discharge Summary between a provider and patient to support the transfer of a patient between care settings, or The exchange of clinical summaries between providers and patients to support the closed-loop transfer of a patient from one care setting to another consultation referral. Scenario 2: The Transfer of Patient Information between Providers: The transfer of patient information between providers occurs in three ways: 1. 2. 3. 1.2.2 The exchange of information to support the transfer of patient information from one provider to another, A closed loop referral, or A complex series of care transitions. Information Exchanges Discharge Instructions: The Discharge Instructions contains the standard set of information to be communicated from a provider to a patient (or also to another provider) and includes follow-up or plan of care. The Discharge Instructions may be generic, patient-specific, or disease-specific depending on the facility’s practices and the patient needs. The document includes standard basic data set including demographic data, active reconciled medication list (with doses and sig), allergy list and problem list. The document is given to the patient by their care manager before physical discharge and upon patient acknowledgement, the physical discharge is triggered. Sender: Hospital EHR System Receiver: PCP EHR System The Discharge Instructions are supported by the Transition of Care Clinical Information Model (CIM). The CIM model provides a concise and defined vocabulary for the sharing of care transition information used to generate the constructs. The ToC CIM can be represented in XML but provides specialized XML tag names and other structure for data that is constrained to meet the specific information exchange requirements of the care transition. The ToC CIM also provides the reference vocabulary for consistent and reusable care transition information exchanges. The structure and meaning of ToC CIM object data is defined by the model and associated data dictionary and are represented as an XML schema, thereby providing a common framework for the exchange of information during a care transition. For more information on the ToC CIM, see Section 3. Audience The audience of this implementation guide includes, but is not limited to, software developers, vendors, the ToC Reference Implementation and Pilots Workgroup, and other HIT implementer parties. This implementation guide is also intended to be of specific use to ONC Initiative Partners (OIP) who are interested in transitioning from current CDA-based solutions to a new Consolidated CDA approach. Several assumptions are made regarding the audience: There is a solid understanding and knowledge of HL7 CDA R2 prior to implementing this guidance The reader has a foundational understanding of healthcare standards. The reader has technical knowledge of data models and implementation experience. Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 6 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Organization of This Guide This implementation guide contains both CDA sections and entries to show how specific care transition CDA-based documents can be assembled in support of health information exchange. Each exchange or set of exchanges would contain a general CDA header and one or more of four critical care transition constructs. The CDA Header is applied across all the construct document-level templates uniquely defined in this guide. Each care transition construct references reusable section-level and entry-level templates from the Consolidated CDA Release 2 Implementation Guide, which serves as a library documents, sections and entries. Templates Template identifiers (template IDs) are assigned at the document, section, and entry level. When valued in an instance, the template identifier signals the imposition of a set of template-defined constraints. The value of this attribute provides a unique identifier for the template in question. Please refer to the Consolidated CDA IG (Section 1.6) for additional information on template identifiers and how they are used. Conformance CDA implementers characterize conformance requirements in terms of three general levels that correspond to three different, incremental types of conformance statements: Level 1 requirements impose constraints upon the CDA Header. The body of a Level 1 document may be XML or an alternate allowed format. If XML, it must be CDA-conformant markup. Level 2 requirements specify constraints at the section level of a CDA XML document: most critically, the section code and the cardinality of the sections themselves, whether optional or required. Level 3 requirements specify constraints at the entry level within a section. A specification is considered "Level 3" if it requires any entry-level templates. Refer to the Consolidated CDA IG (Section 1.7) for additional information regarding levels of constraint, conformance statements, conformance verbs, cardinality, vocabulary conformance, and null flavor. Conventions The conventions used in this document are intended to outline a set of tables for implementers to use as guidance. Refer to the Consolidated CDA IG (Section 1.8) for information regarding XPath notation, XML examples, and sample documents. Section Preamble A description of the CDA section is provided, within the context of a care transition. This preamble includes the list of conformance statements required for the CDA section template, as well as underlying entry-level templates that may apply. These conformance statements MAY be an addition to the conformance statements contained within the Consolidated CDA guide. Some of these conformance statements also specify the use of specific value sets for a care transition, which are drawn from existing implementation guidance such as HITSP C80 and HITSP C83. A full listing of all conformance statements can be drawn from the conformance statements links in the Implementer Notes (Section 1.7.2). Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 7 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 1.8.1 CDA Implementation Table The CDA Implementation table immediately follows the section preamble and contains key implementation details about the section. Reference Document The source for the section template. 1.8.2 CDA Template ID (Proposed) The CDA Template ID for the section. The implementer SHALL include the template ID in each section to declare conformance to the CDA Consolidation Guide. Required/ Optional Indicates whether the CDA Section is required or optional for the care transition. Consolidated CDA IG Reference Provides the specific reference to the CDA Consolidation Implementation Guide to determine conformance requirements and optionality. Code Set Provides the recommended terminology to be used for that section. Reference Document: For some sections, implementation guidance is provided both for Consolidated CDA and HITSP C83. This is provided to ensure smooth transition planning for those implementers who may already be using a C32 or CCD for a care transition information exchange. CDA Template ID (Proposed): A conformance statement that should be followed for each CDA Section. In order to be conformant with the Consolidated CDA Guide, a CDA Document SHALL declare conformance for the specific section by including a <templateID> element with the root attribute set to the value. Required/Optional: This indicates whether the CDA Section and/or Entry is required for the particular information exchange or is optional. Consolidated CDA IG Reference: This will indicate the specific location of the CDA Section and/or Entry within the Consolidated CDA Guide. This reference allows an implementer to quickly access the relevant conformance statements for the CDA Section and/or Entry. Code Set: The recommended code set to be used for that CDA Section and/or Entry. Implementer Notes The implementer notes include the following: Links to conformance statements Links to XML samples of the CDA Section and/or Entry, where appropriate These links are provided as an implementer resource and are derived from CDAtools.org made available by Open Health Tools (OHT) for use in support of this implementation guidance. In many cases, the current samples and conformance statements provided are linked to HITSP C32 and/or the CCD. As the Consolidated CDA Guide is completed within the HL7 ballot process, all links will be updated to point to the most recent Consolidated CDA examples and conformance statements. The HITSP C32 and/or CCD examples and conformance statements are FULLY USABLE in conjunction with Consolidated CDA. Data Element CDA XPath Reference R/O CIM Reference Null Values Notes Does the data element allow for Additional implementation CDA FULL XPATH REFERENCE HERE HITSP C83 data element listed for A link to the CDA XPath specific to Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Required or Optional A reference to the applicable Page 8 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology implementer reference (to include business names in future releases) this data element, so implementers know where a specific data element will go CIM Object and CIM Data Element a null value or not? notes, such as required value sets, required XML entries, etc. Data Element: The data element listed in this table is drawn from HITSP C154 and is provided to give implementers a specific business name to reference when populating the relevant CDA Section and/or Entry. CDA XPath Reference: This XML expression outlines where the data element would be captured within a CDA document. R/O: Indicates whether the data element is required or optional within the specific CDA Section and/or Entry. Null Values: Outlines whether null values are allowed or not for this data element. CIM Reference: References the specific ToC CIM data element. Notes: Additional implementation notes, such as which value set to be used to encode an element or where this data might also be represented within a CDA document. 2. Discharge Instructions Implementation Guidance The following construct sections describe the purpose and rules for constructing a conforming CDA document. Construct templates include constraints on the CDA header and refer to section-level templates. The Document Types and Required/Optional Sections table lists the sections used by each document type. Each document-level template contains the following information: Scope and intended use of the document type Description and explanatory narrative. Template metadata (e.g., templateID, etc.) Header constraints: this includes a reference to the US Realm Clinical Document Header template and additional constraints specific to each document type Required and optional section-level templates CDA Header Information The CDA header would contain most of the demographic information needed in support of the CIM Objects listed below. The table below maps the header to the ToC CIM, for requirements traceability. CDA Section Name US Realm Header CDA Template ID (Proposed) 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] 2.16.840.1.113883.10.20.21.1.1 Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Required/ Optional CIM Object Required Patient Information Required Culturally Sensitive Patient Care Required Patient Contact Information Required Support Contacts Page 9 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology [US Realm Document Header] 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] 2.1.1 Required Primary Care Providers and Designated Providers Contact Information For a support contact, the classCode attribute, representing the Contact Type, shall be coded as specified in the Care Transition – Contact Type Value Set For a support contact, the contact relationship SHALL have be coded as specified in the Care Transition – Relationship Value Set For a support contact, the state part of an address SHALL be recorded using the Care Transition – State Value Set For a support contact, the postal code part of an address in the United States SHALL be recorded using the Care Transition – Postal Code Value Set For a support contact, the country part of an address SHALL be recorded using the Care Transition – Country Value Set Data Element CDA XPath Reference R/O CIM Reference Null Values Notes /cda:ClinicalDocument/cda:participant Date cda:time R None Identified cda:associatedEntity or cda:patientRole/cda:patient/cda:guardian Contact Type @classCode R Contact Relationship cda:code R Contact Address cda:addr R2 cda:telecom R Contact Phone/Email/ URL cda:associatedPerson/cda :name OR Contact Name R cda:guardianPerson/cda: name Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Contact Type Primary and/or Secondary Emergency Contact Relationship Primary and/or Secondary Emergency Contact Address Primary and/or Secondary Emergency Contact Phone Use – Care Transition – Contact Type Value Set Use – Care Transition – Relationship Value Set Primary and/or Secondary Emergency Contact Name Page 10 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 2.1.2 Person Information For a patient address, each address part SHALL be identified using the <streetAddressLine>, <city>, <state>, <postalCode> and <country> tags For a patient address, more than one <streetAddressLine> MAY be present For a patient address, NO MORE than four <streetAddressLine> elements SHALL be present For a patient address, the <country> element SHALL be present for addresses outside of the United States For a patient address, at most one address for a person SHALL have a use attribute with a value containing "HP" For a patient address, at least one address for a patient SHOULD have a use attribute with a value containing "HP" For a patient address, one or more vacation addresses MAY be present for a person For a patient address, a vacation address SHALL be recorded with a use attribute containing the value "HV" For a patient address, one or more work addresses MAY be present For a patient address, a work address SHALL be recorded with a use attribute containing the value "WP" For a patient address, the <country> SHALL be recorded using Care Transition – Country Value Set For a patient name, each name part SHALL be identified using one of the tags <given>, <family>, <prefix> or <suffix> For a patient name the "first" name of the patient SHALL appear in the first <given> tag. For a patient name, the "middle" name of the patient, if it exists, SHALL appear in the second <given> tag. For a patient name, the name parts within a <name> tag SHALL be ordered in proper display order For a patient name, at most one <name> tag SHALL have a use attribute containing the value "L", indicating that it is the legal name of the patient For a patient name, more than one <name> tag MAY be present to retain birth name, maiden name and aliases For a patient name, an alias or former name MAY be identified by the inclusion of a use attribute containing the value "P" For a patient name, name parts MAY be identified as being a name given at birth or adoption by the inclusion of a qualifier attribute containing the value "BR" for birth or "AD" for adoption For a patient name, a name part SHALL be identified as the patient's preferred name by the inclusion of a qualifier attribute containing the value "CL" on the name part For a patient name, a prefix or suffix that is an academic title or credential SHALL be identified by the inclusion of a qualifier attribute containing the value "AC" on the name part For a patient, the ethnicity SHALL be coded as specified in Care Transition – Ethnicity Value Set For a patient, the marital status SHALL be coded as specified in Care Transition – Marital Status Value Set For a patient, the gender SHALL be coded as specified in Care Transition – Gender Value Set For a patient, the race SHALL be coded as specified in Care Transition – Race Value Set The primary religious affiliation MAY appear in the <religiousAffilliationCode> element For a patient, the religious affiliation SHALL be coded as specified in Care Transition – Religion Value Set For a patient, a home phone number SHALL be represented with a use attribute containing the value "HP" For a patient, a vacation home phone number SHALL be represented with a use attribute containing the value "HV" For a patient, a work phone number SHALL be represented with a use attribute containing the value "WP" Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 11 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology For a patient, a mobile phone number SHALL be represented with a use attribute containing the value "MC" For a patient, an e-mail address SHALL appear in a <telecom> element using the 'mailto:' URL scheme (see IETF/RFC-2368), and SHALL encode only a single mailing address, without any headers Data Element CDA XPath Reference R/O CIM Reference Null Values Notes /cda:ClinicalDocument/cda:effectiveTime Document Timestamp n/a R Not Applicable Not Allowed One entry only /cda:ClinicalDocument/cda:recordTarget/cda:patientRole Person ID Person Address Person Phone /Email /URL cda:id R Patient Identifiers Not Allowed cda:addr R Patient Address Allowed cda:telecom R Patient Phone Allowed cda:patient Person Name cda:name R Patient Name Allowed cda:administrativeGen derCode R Patient Gender Allowed Person Date of Birth cda:birthTime R Marital Status cda:maritalStatusCode R2 Religious Affiliation cda:religiousAffiliation Code O Race cda:raceCode OR sdtc:raceCode R Ethnicity cda:ethnicityCode R Gender Patient Date of Birth Patient Marital Status Culturally Sensitive Patient Care: Religion Culturally Sensitive Patient Care: Race Culturally Sensitive Patient Care: Ethnicity Allowed cda:recordTarget/cda:patientRole/cda:patient/cda:languageCommunication Language 2.1.3 n/a R Patient Language Provider Information For a provider, the provider role SHALL be coded as specified in Care Transition - Provider Role Value Set in Appendix C For a provider, the provider type SHALL be coded as specified in Care Transition – Provider Type Value Set in Appendix C For a provider, the state part of an address SHALL be recorded using Care Transition – State Value Set in Appendix C For a provider, the postal code part of an address in the United States SHALL be recorded using Care Transition – Postal Code Value Set in Appendix C Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 12 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology For a provider, the country part of an address SHALL be recorded using Care Transition – Country Value Set in Appendix C Data Element CDA XPath Reference R/O CIM Reference Null Values Notes /cda:ClinicalDocument/cda:documentationOf/cda:serviceEvent/cda:performer Date Range cda:time R None Identified Provider Role Coded cda:functionCode R2 Designated Provider Domain of Management Provider Role Free Text cda:originalText R2 None Identified cda:assignedEntity Provider Type Provider Address Provider Phone/Email/ URL Provider Name Provider's Organization Name Provider's Patient ID National Provider ID cda:code R cda:addr R cda:telecom R cda:assignedPerson/ cda:name cda: representedOrganization/ cda:name R R Designated Provider Specialties Designated Provider Address Designated Provider Phone Designated Provider Name Designated Provider Organization Allowed Allowed Allowed sdtc:patient/sdtc:id R2 None Identified Allowed n/a R2 Designated Provider NPI Allowed Discharge Instructions The Discharge Instructions would include a standard data set including demographic information, active reconciled medication list (with doses and sig), allergy list and problem list. Discharge Instructions also contains dataset relevant to the Discharge Summary/Discharge Instructions context which includes follow-up/plan of care. The following table summarizes the specific CDA templates that align to these requirements: CDA Section Name CDA Template ID Advanced Directives 2.16.840.1.113883.10.20.22.2.21 Allergies, Adverse Reactions, Alerts Hospital Discharge Medications Immunizations 2.16.840.1.113883.10.20.21.2.6.1 2.16.840.1.113883.10.20.21.2.6. 2.16.840.1.113883.10.20.22.2.11.1 2.16.840.1.113883.10.20.22.2.11 2.16.840.1.113883.10.20.22.2.2.1 Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Required/ Optional Required Required Required Required CIM Object Mapping Existence of Advanced Directives Allergies and Intolerances Active Medication List Immunization Code Set Page 13 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Medical Equipment Plan of Care Problem List 2.2.1 2.16.840.1.113883.10.20.22.2.2 2.16.840.1.113883.10.20.22.2.23 2.16.840.1.113883.10.20.22.2.10 2.16.840.1.113883.10.20.22.2.5.1 2.16.840.1.113883.10.20.22.2.5 Required Required Required History Equipment Active Problem List Advance Directives Section This section contains data defining the patient’s advance directives and any reference to supporting documentation. The most recent and up-to-date directives are required, if known, and should be listed in as much detail as possible. This section contains data such as the existence of living wills, healthcare proxies, and CPR and resuscitation status. If referenced documents are available, they can be included in the CCD exchange package. NOTE: The descriptions in this section differentiate between “advance directives” and “advance directive documents”. The former are the directions whereas the latter are legal documents containing those directions. Thus, an advance directive might be “no cardiopulmonary resuscitation”, and this directive might be stated in a legal advance directive document. The Advance Directive Type SHALL be coded using the Advance Directive Type Value Set in Appendix C The human readable description of the type of Advance Directive SHALL appear in the narrative text and SHALL be pointed to by the value attribute of the <reference> element inside the <originalText> element of the <code> The starting time of the Advance Directive SHALL be recorded in the <low> element of the <effectiveTime> element in the Advance Directive <observation> If the starting time is unknown, the <low> element SHALL have the nullFlavor attribute set to UNK The ending time of the Advance Directive SHALL be recorded in the <high> element of the <effectiveTime> element in the Advance Directive <observation> If the ending time is unknown, the <high> element SHALL have the nullFlavor attribute set to UNK If the Advance Directive does not have a specified ending time, the <high> element SHALL have the nullFlavor attribute set to NA CDA Template ID 2.16.840.1.113883.10.20.22.2.21 Required/ Optional Required Consolidated CDA IG Reference Code Set Refer to the CDAR2_IG, Section 42348-3 for Required/Optional Entries Implementer Notes The value sets recommended for the Advance Directives Section are available in Appendix C of this guide. Advance Directives conformance statements and XML examples can be found in the Advance Directives Section of the CCD. Data Element CDA XPath Reference Advance Directive Type cda:code Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 R/O CIM Reference Null Values R Advance Directive Type Allowed Notes Page 14 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Advance Directive Free Text Type cda:originalText/ cda:reference/@value R Advance Directive Existence Allowed Effective Date cda:effectiveTime R Advance Directive Range Allowed Custodian of the Document cda:participant[@type Code='CST']/ cda:participantRole[@ classCode='AGNT'] R Advance Directive Owner Allowed 2.2.2 Use: Advance Directive Type Value Set Must use: typeCode = CST moodCode = AGNT Allergies, Adverse Reactions, and Alerts Section This section lists and describes any medication allergies, adverse reactions, idiosyncratic reactions, anaphylaxis/anaphylactoid reactions to food items, and metabolic variations or adverse reactions/allergies to other substances (such as latex, iodine, tape adhesives) used to assure the safety of health care delivery. At a minimum, it should list currently active and any relevant historical allergies and adverse reactions. In general this section should not include environmental allergies, even if severe and directly related to the presenting problem, since they constitute a medical problem; environmental allergies should be listed in the problem list and past medical history. The Allergies Section SHOULD contain at least one Allergy Problem Act entry The Allergies Section SHALL include all data elements listed The Adverse Event Type in the Allergies Section SHALL be coded as specified in Allergy/Adverse Event Type Value Set in Appendix C Food and substance allergies (captured in Product Coded data element) in the Allergies Section SHALL be coded as specified in the Allergy/Adverse Event Food and Other Allergens Value Set in Appendix C Allergies to a class of medication (captured in Product Coded data element) in the Allergies Section SHALL be coded as specified in the Allergy/Adverse Event Medication Drug Class Value Set in Appendix C Allergies to a specific medication (captured in Product Coded data element) in the Allergies Section SHALL be coded as specified in the Allergy/Adverse Event Medication Clinical Drug Name Value Set in Appendix C The Reaction Coded in the Allergies Section SHALL be coded as specified in the Allergy/Adverse Event Reaction Value Set in Appendix C The Severity Coded in the Allergies Section SHALL be coded as specified in the Allergy/Adverse Event Reaction Value Set in Appendix C CDA Template ID (Proposed) 2.16.840.1.113883.10.20.21.2.6.1 2.16.840.1.113883.10.20.21.2.6. Required/ Optional Required Consolidated CDA IG Reference Refer to the CDAR2_IG, Section 48765-2 for Required/Optional Entries Code Set LOINC 2.16.840.1.11 3883.6.1 Implementer Notes The value sets recommended for the Allergies, Adverse Events, and Alerts Section are available in Appendix C of this guide. Allergies, Adverse Events, and Alerts Section conformance statements and XML examples can be found in the Allergies Reaction Section of HITSP C32/C83 Alert Section conformance statements and XML examples can be found in the Alerts Section of the CCD Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 15 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Data Element CDA XPath Reference R/O CIM Reference Null Values Notes cda:act[cda:templateId/@root=’2.16.840.1.113883.10.20.22.4.30’]/cda:entryRelationship[@typeCode='SUBJ']/cda:o bservation[cda:templateId/@root='2.16.840.1.113883.10.20.22.4.7’] Adverse Event cda:effectiveTime R Reaction Date Allowed Date Use Care Transition Adverse Event Allowed with cda:code R Reaction Type – Adverse Event Type specific constraints Type Value Set cda:participant[@typeCode='CSM']/cda:participantRole[@classCode='MANU']/ cda:playingEntity[@classCode='MMAT']/ All Environmental Allergens AND/OR Product Freecda:name R All Food Allergens Text Allowed AND/OR Medication Intolerance Product Coded cda:code R A/I Attributes Allowed cda:entryRelationship[@typeCode='MFST']/cda:observation[templateId/@root=’2.16.840.1.113883.10.20.22.4.9’] Reaction FreeText cda:text R2 List of Reactions Allowed Reaction Coded cda:value R2 Reaction Attributes Allowed If not known, a codified Null value is required If not known, a codified Null value is required cda:entryRelationship[@typeCode='SUBJ']/cda:observation[templateId/@root=’2.16.840.1.113883.10.20.22.4.8’] Severity FreeText cda:text R2 Severity of Intolerance or Allergy Allowed Severity Coded cda:value R2 Severity Attributes Allowed 2.2.3 If not known, a codified Null value is required If not known, a codified Null value is required Hospital Discharge Medications Section The Hospital Discharge Medications Section defines the medications that the patient is intended to take (or stop) after discharge. At a minimum, the currently active medications should be listed with an entire medication history as an option. The section may also include a patient’s prescription history and indicate the source of the medication list, for example, from a pharmacy system versus from the patient. In addition to conformance statements defined in the Consolidated CDA guide, the following additional conformance statements are applicable: The Hospital Discharge Medications Section SHALL include entries from the Medication section The Hospital Discharge Medications Section SHALL provide the relevant medications ordered for the patient for use after discharge in coded form. CDA Template ID (Proposed) Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Required/ Consolidated CDA IG Reference Code Set Page 16 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Optional 2.16.840.1.113883.10.20.22.2.11.1 2.16.840.1.113883.10.20.22.2.11 Required Refer to the CDAR2_IG, Section 10183-2 for Required/Optional Entries Implementer Notes 2.2.4 Hospital Discharge Medications Section conformance statements and XML examples can be found in the Hospital Discharge Medications Section of HITSP C32/C83 Immunizations Section The Immunizations Section defines a patient’s immunization status in the context of a care transition. The Immunizations Section SHOULD include current immunization status The Immunizations Section MAY contain the entire immunization history. The Immunizations Section SHALL support all data elements listed. The Coded Product Name in the Immunizations Section SHALL be coded as specified in the Immunizations Administered Vaccines Value Set in Appendix C The Refusal Reason in the Immunizations Section SHALL be coded as specified in the Immunizations Reason Value Set in Appendix C CDA Template ID (Proposed) 2.16.840.1.113883.10.20.22.2.2.1 2.16.840.1.113883.10.20.22.2.2 Required/ Optional Optional Consolidated CDA IG Reference Code Set Refer to the CDAR2_IG, Section 11369-6 for Required/Optional Entries CVX Implementer Notes The value sets recommended for the Immunizations Section are available in Appendix C of this guide. Immunization Section conformance statements and XML examples can be found in the Immunizations Section of the CDA R2 Consolidation Guide. This section also needs to conform to the Immunizations Narrative Section conformance statements. Data Element CDA XPath Reference R/O CIM Reference Null Values Notes cda:substanceAdministration[cda:templateId/@root = '2.16.840.1.113883.10.20.1.24'] Refusal Administered Date @negationInd R Contraindication Allowed cda:effectiveTime R Immunization Date Allowed cda:entryRelationship[@typeCode='SUBJ']/cda:observation/cda:value Medication Series Number Reaction R Immunization Series Allowed cda:entryRelationship[@typeCode='CAUS']/cda:observation[cda:templateId/@root= 2.16.840.1.113883.10.20.1.54] Observed O Reaction Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 17 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Performer cda:performer/ cda:assignedEntity O Immunization ID cda:consumable/cda:manufacturedProduct Coded Product Name Free Text Product Name Drug Manufacturer Lot Number cda: manufacturedMaterial/ cda:code cda:originalText cda: manufacturerOrganization cda:manufacturedMaterial /cda:lotNumberText R R R R Active Medication List Active Medication List Active Medication List Active Medication List Allowed Allowed If the name of the product is unknown, the type, purpose or other description may be supplied. Allowed Allowed cda:entryRelationship[@typeCode=RSON]/cda:act[cda:templateId/@root=2.16.840.1.113883.10.20.1.27] Refusal Reason 2.2.5 R2 Contraindication Reason Plan of Care Section The Plan of Care Section contains data that defines pending orders, interventions, encounters, services, and procedures for the patient. It is limited to prospective, unfulfilled, or incomplete orders and requests only. All active, incomplete, or pending orders, appointments, referrals, procedures, services, or any other pending event of clinical significance to the current care of the patient should be listed unless constrained due to privacy issues. The plan may also contain information about ongoing care of the patient and information regarding goals and clinical reminders. Clinical reminders are placed here to provide prompts for disease prevention and management, patient safety, and health-care quality improvements, including widely accepted performance measures. The plan may also indicate that patient education was given or will be provided. This section SHALL conform to the HL7 History and Physical Note and HL7 Consultation Note requirements for this section This section MAY include entries conforming to the Hospital Discharge Medications and Immunizations Sections to provide information about the intended care plan. CDA Template ID (Proposed) 2.16.840.1.113883.10.20.22.2.10 Required/ Optional Required Consolidated CDA IG Reference Code Set Refer to the CDAR2_IG, Section 18776-5 for Required/Optional Entries Implementer Notes Plan of Care Section conformance statements and XML examples can be found in the Plan of Care Section of the CCD NOTE: The data elements required for the Plan of Care Section are being developed as part of the S&I Framework Longitudinal Coordination of Care WG. Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 18 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 2.2.6 Problem List Section This section lists and describes all relevant clinical problems at the time the document is generated. At a minimum, all pertinent current and historical problems should be listed. In addition to conformance statements defined in the Consolidated CDA guide, the following additional conformance statements are applicable: The Problem List Section SHOULD contain all reconciled problems, including all discharge diagnoses. In the Problem List Section, the Problem Name SHALL be recorded in the Problem Entry by recording a <reference> where the value attribute points to the narrative text containing the name of the problem. In the Problem List Section, the Age (at Onset) SHALL be recorded in the <low> element of the <effectiveTime> element In the Problem List Section, the Treating Provider or Providers SHALL be recorded in a <performer> element under the <act> that describes the problem In the Problem List Section, the Treating Provider ID SHALL be present in the <id> element beneath the <assignedEntity> In the Problem List Section, the Problem Type SHALL be coded as specified in the Problem Type Value Set in Appendix C. In the Problem List Section, the Problem SHALL be coded as specified in the Care Transition - Problem Value Set Recommendation in Appendix C CDA Template ID (Proposed) 2.16.840.1.113883.10.20.22.2.5.1 2.16.840.1.113883.10.20.22.2.5 Required/ Optional Required Consolidated CDA IG Reference Refer to the CDAR2_IG, Section 11450-4 for Required/Optional Entries Code Set LOINC 2.16.840.1.11 3883.6.1 Implementer Notes The value sets recommended for the Problem List Section are available in Appendix C of this guide. Problem List Section conformance statements and XML examples can be found in the Problem List Section of the CDA R2 Consolidation Guide. This section also needs to conform to the Problem List Narrative Section conformance statements. Data Element CDA XPath Reference R/O CIM Reference Null Values Notes cda:act[cda:templateId/@root='2.16.840.1.113883.10.20.1.27']/ cda:entryRelationship[@typeCode='SUBJ']/cda:observation[cda:templateId/@root='2.16.840.1.113883.10.20.1.28'] Start Date of Part of Problem Problem Date cda:effectiveTime R Allowed Problem Entry Active Problem Part of Problem Problem Type cda:code R Not Allowed Type Entry Active Problem Part of Problem Problem Name cda:text R Allowed Name Entry Active Problem Part of Problem Problem Code cda:value R Allowed Attributes Entry cda:act[cda:templateId/@root='2.16.840.1.113883.10.20.1.27']/cda:performer Treating Provider Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 O Problem Assignee Page 19 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology cda:entryRelationship/cda:observation[cda:templateId/@root ='2.16.840.1.113883.10.20.1.38'] Age (at Onset) O cda:entryRelationship[@typeCode='CAUS']/cda:observation Cause of Death R Allowed cda:entryRelationship/cda:observation[cda:templateId/@root ='2.16.840.1.113883.10.20.1.38'] Age (at Death) O Time of Death R Treating Provider ID R2 Problem Status 2.2.7 cda:entryRelationship /cda:observation /value/@code Allowed Problem Assignee ID R See Notes Allowed Allowed The CIM assumes for an active problem list that the Problem Status is Active Medical Equipment Section The Medical Equipment Section defines a patient’s implanted and external medical devices and equipment that their health status depends on, as well as any pertinent equipment or device history. This section is also used to itemize any pertinent current or historical durable medical equipment (DME) used to help maintain the patient’s health status. All pertinent equipment relevant to the diagnosis, care, and treatment of a patient should be included. The Medical Equipment Section SHALL conform to the HL7 Medical Equipment CCD section The Medical Equipment Section SHALL conform to Health IT Standards Committee recommendations for the use of SNOMED-CT in coding devices. The Medical Equipment Section shall capture the following information for “History of Medical Device Use” o <code code='46264-8' displayName='HISTORY OF MEDICAL DEVICE USE'> In the Medical Equipment Section, under the <text>element, the Medical Equipment History SHALL be provided in a narrative format. CDA Template ID 2.16.840.1.113883.10.20.22.2.23 Required/ Optional Required Consolidated CDA IG Reference Code Set Refer to the CDAR2_IG, Section 46264-8 for Required/Optional Entries Implementer Notes Medical Equipment Section conformance statements and XML examples can be found in the Medical Equipment Section of the CCD. Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 20 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 3. TOC Clinical Information Model (CIM) The Transitions of Care (ToC) Clinical Information Model (CIM) has been developed in support of the S&I Framework to promote healthcare stakeholders’ collective understanding of care transitions. It is a prototype that is intended to serve as a logical overlay and unbiased representation of the data needed to support care transitions. Moreover, while CIM provides insight to clinicians into the type of data needed to support care transitions, it also gives implementers and vendors perspective on how to store and exchange that data. The ToC CIM is intended to be a logical view of the common data model that underlies all care transition information. In practice, it will manifest itself as physical data within an organization engaged in transitions of care but is not tied to an underlying information model. The focus of the CIM is on providing a clear view for a clinician on the data they are accustomed to looking at and manipulating within their clinical workflow. In this way, it provides a functional perspective that allows for the mapping of care transition requirements to an underlying technical standard. For the TOC CIM, this means mapping to the underlying CDA on which entity, known as a CIM Object, would be based. A secondary purpose is to enable the creation of an object-oriented model that maps the requirements for care transitions to ToC CIM objects. This is a longer-term goal that will require further testing and analysis of the ToC CIM. For additional information on the development of the CIM, reference the TOC Clinical Information Model on the wiki. ToC CIM Objects The following table lists the CDA implementation guidance for all ToC CIM Objects, as defined by the S&I Framework Transitions of Care Initiative. Specific guidance is provided showing a mapping from each CIM Object to the relevant CDA Section and Entry-Level templates that are used to provide the CIM Data Elements needed. Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 21 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology All CDA Mappings CIM Object Name Active Medication List Active Problem List Admitting and Discharging Diagnoses Allergies and Intolerances Anticipatory Guidance Behavioral Health History Care Team Members Consultant(s) Assessment(s) and Plan(s) Recommendations Culturally Sensitive Patient Care Demographics Diet Discontinued Medications Equipment Existence of Advanced Directives Family History Follow-up Appointments Goals CDA Template ID CDA Section ID 2.16.840.1.113883.10.20.22.2.1.1 2.16.840.1.113883.10.20.22.2.1 2.16.840.1.113883.10.20.22.2.38 4.28 Medications 2.16.840.1.113883.10.20.22.2.7 2.16.840.1.113883.10.20.22.2.24 2.16.840.1.113883.10.20.22.4.33 2.16.840.1.113883.10.20.21.2.6.1 2.16.840.1.113883.10.20.21.2.6. TO BE DETERMINED TO BE DETERMINED TO BE DETERMINED 2.16.840.1.113883.10.20.22.1.9 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] 1.3.6.1.4.1.19376.1.5.3.1.3.33 2.16.840.1.113883.10.20.22.2.1 2.16.840.1.113883.10.20.22.2.23 2.16.840.1.113883.10.20.22.2.21 2.16.840.1.113883.10.20.22.2.15 2.16.840.1.113883.10.20.21.2.10 2.16.840.1.113883.10.20.21.2.1 Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 4.40 Problem List 4.20 Hospital Discharge Diagnosis 4.2 Allergies, Adverse Reactions, Alerts CDA Entry ID 5.14 Medication Activity 5.16 Medication Information 5.12 Indication 5.13 Instructions 5.17 Medication Supply Order 5.19 Precondition for Substance Administration 5.9 Drug Vehicle 5.3 Allergy Problem Act 5.5 Condition 5.6 Condition Entry 5.7 Discharge Diagnosis 5.4 Allergy Alert Observation 5.3 Allergy Problem Act 4.35 Plan 4.4 Assessment 4.5 Assessment and Plan 4.11 Discharge Diet 4.28 Medications 5.14 Medication Activity 5.16 Medication Information 4.26 Medical Equipment 4.1 Advance Directives 4.13 Family History 4.35 Plan 4.30 Objective Page 22 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology All CDA Mappings CIM Object Name CDA Template ID Health Literacy Health Maintenance History Present Illness TO BE DETERMINED TO BE DETERMINED 1.3.6.1.4.1.19376.1.5.3.1.3.4 Immunization History 2.16.840.1.113883.10.20.22.2.2.1 2.16.840.1.113883.10.20.22.2.2 Invasive and Non-Invasive Procedures 2.16.840.1.113883.10.20.22.2.7 Medical History 2.16.840.1.113883.10.20.22.2.39 2.16.840.1.113883.10.20.22.2.1 Medication History 2.16.840.1.113883.10.20.22.1.7 Operative Summary CDA Section ID 4.35 Plan 4.18 History of Present Illness 4.24 Immunizations 4.41 Procedure Description 4.42 Procedure Disposition 4.43 Procedure Estimated Blood Loss 4.44 Procedure Findings 4.45 Procedure Implants 4.46 Procedure Indications 4.47 Procedure Specimens Taken 4.48 Procedures Section 4.27 Medical History 4.28 Medications 5.21 Procedure Activity 5.22 Procedure Activity Act 5.23 Procedure Activity Observation 5.14 Medication Activity 5.16 Medication Information 5.2 Alert Status Observation Patient Contact Information 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] Patient Information 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] Patient Instructions Patient Self-Management 5.21 Immunization Activity 5.22 Immunization Medication Information 5.23 Refusal Reason 4.31 Operative Note Fluid 4.32 Operative Note Surgical Procedure Outcome of Allergy/Intolerance Patient Consent Directive CDA Entry ID 2.16.840.1.113883.10.20.21.4.20 Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 5.13 Instructions 4.35 Plan Page 23 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology All CDA Mappings CIM Object Name Payer Information CDA Template ID 2.16.840.1.113883.10.20.22.2.18 Pending Tests and Procedures Physical Activity Physical Exam Primary Care Physicians and Designated Providers Reason for Consult Request Restorative Care Review of Systems Social Determinants of Health Social History Support Contacts 2.16.840.1.113883.10.20.21.2.2 2.16.840.1.113883.10.20.22.2.19 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] CDA Section ID 4.33 Payer 4.35 Plan 4.48 Procedure 4.53 Subjective 4.34 Physical Exam CDA Entry ID 4.49 Reason for Visit TO BE DETERMINED 1.3.6.1.4.1.19376.1.5.3.1.3.18 TO BE DETERMINED 2.16.840.1.113883.10.20.22.2.17 2.16.840.1.113883.10.20.21.1.1 [US Realm Document Header] 4.51 Review of Systems 4.5.2 Social History 5.59 Social History Observation 5.21 Procedure Activity 5.22 Procedure Activity Act 5.23 Procedure Activity Observation 5.30 Vital Signs Organizer 5.31 Vital Signs Observation Surgical/Procedure History 2.16.840.1.113883.10.20.22.2.7 4.41 Procedure Description 4.48 Procedure Vital Signs 2.16.840.1.113883.10.20.22.2.4.1 2.16.840.1.113883.10.20.22.2.4 4.34 Physical Exam 4.56 Vital Signs Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 24 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 4. Additional Guidance for Implementers and Vendors The following information is supplied as a starting point for information on the various tools and information one may find useful (depending on their proficiency). • • • • Comparison and conversion tools to migrate from the existing CDA standard to new Consolidated CDA CCR-Consolidated CDA conversion tool for vendors who previously implemented CCR* Openly available data modeling tools, reference implementation code, and test suite**, to aid to lower implementation time and costs Educational resources Tools The Transitions of Care Initiative has worked to enable the availability of multiple tools and educational resources needed in support of using technology to improve care transitions. These tools are designed to provide the level of automated tooling needed in support of Consolidated CDA. 4.1.1 OHT/MDHT The implementation guidance used for Transitions of Care is designed to be generated directly from MDHT. The MDHT-generated guidance includes the appropriate level of specification and detail needed to implement a care transition information exchange, including API’s, code documentation, and models needed for implementation. MDHT allows the creation of computable models of the templates in UML. These models can be used to produce: Template Specifications (DITA, XHTML, PDF, Other) Conformance/Validation Tools Model Driven Code Generation Schematron The project has already built models from the following specifications: HL7 Continuity of Care Document HITSP C83 Sections and Entries IHE Patient Care Coordination Technical Framework HL7 Common Document Types Consolidated CDA MDHT is available for download at: https://www.projects.openhealthtools.org/sf/projects/mdht/ 4.1.2 Trifolia Tooling support is also provided by Lantana Group and their Trifolia Workbench, which supports standards authors, developers and implementers in capturing, storing and managing HL7 Clinical Document Architecture (CDA) templates. Trifolia is available for download from http://www.lantanagroup.com/resources/tools/ Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 25 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 4.1.3 NIST Validation/MU testing sites This site organizes key resources (e.g. HITSP, CCHIT, standards and testing tools) in a central place to provide a resource for implementation and interoperability testing activities. http://hit-testing.nist.gov/ http://xreg2.nist.gov/hit-testing/ 4.1.4 TOC Quickstart Site The Transitions of Care (TOC) Quickstart site is a central source to view and download Transitions of Care Initiative guides, work products and models. http://wiki.siframework.org/Transitions+of+Care+Quickstart+Page 4.1.5 myCDA This wiki page serves as a central source for educational and training resources in support of Consolidated CDA. With links to samples, FAQs, and guidance on implementing care transition information exchanges. Sample XML and XSL code is also available to help implementers get started with the use of CDA. The myCDA site is under development and will be available in the next release of this guidance. Educational Resources 4.2.1 Clinical Document Architecture (CDA) The full Clinical Document Architecture Normative Edition is available for purchase from www.HL7.org, this package includes additional publications such as Datatypes, HL7 Value Sets, and other detailed information required for proper implementation of CDA. The following links are provided for those who wish to further their understanding of the HL7 CDA and the ASTM/HL7 Continuity Of Care Document Implementation Guide. The former is the “base standard” selected by S&I Transitions Of Care Initiative for all healthcare documents. 4.2.1.1 CDA Quick Start Guide (v1.5) This Quick Start Guide supports implementers working with simple CDA documents. It covers required elements in the CDA header and body and explains fundamental concepts including the CDA approach to identifiers, vocabulary and data types. CCD Quick Start Guide (v1.0) This Quick Start Guide is for implementers working with the Continuity of Care Document (CCD) which is the basis of the HITSP/C32. Readers should be familiar with the underlying Clinical Document Architecture Release 2.0 (CDA R2) standard, (see the CDA Quick Start Guide). HL7 Structured Documents Technical Committee Wiki This Wiki site is a subset of the full HL7 Wiki site (wiki.hl7.org) Login is not required for browsing pages: http://wiki.hl7.org/index.php?title=Structured_Documents There are a number of sub-categories available from this page relative to the use of CDA, items of particular interest may be: CDA Suggested Enhancements and the associated Formal Proposals, Continuity of Care Document and CCD Errata Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 26 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 5. Appendix A – Reference Documents Document Name Consolidated CDA Implementation Guide Document Description Base standard implementation guide that is used. The Consolidated CDA IG contains a library of CDA templates, incorporating and harmonizing previous efforts from Health Level Seven (HL7), Integrating the Healthcare Enterprise (IHE), and Health Information Technology Standards Panel (HITSP). Consolidated CDA Implementation Guide can be accessed here Click here to access HITSP C80 in PDF Format Click here to access HITSP C83 in PDF Format Click here to access HITSP C154 in PDF Format HITSP C80 HITSP C83 HITSP C154 S&I Framework Transitions of Care Clinical Information Model (CIM) CDA Quick Start Guide v1.5 Reference Location The TOC CIM can be accessed here This Quick Start Guide supports implementers working with simple CDA documents. It covers required elements in the CDA header and body and explains fundamental concepts including the CDA approach to identifiers, vocabulary and data types. Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 CDA Quick Start Guide v1.5 can be accessed here Page 27 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology 6. Appendix B – Acronym List Acronym CIM CCR CDA FIPS HITSP HL7 Definition of Acronym A Clinical Information Model is a conceptual definition of the discrete structured clinical information that is used in a clinical context. The model defines the data elements, attributes, possible values and types of attributes that are needed to convey the clinical reality in a fashion that is understandable to both clinical domain experts and modelers. These models have the potential for being used as part of electronic health information exchange including EMR's, EHR's, Telehealth applications, medical devices, analytics, decision support among others. Continuity of Care Record - is a patient health summary standard. It is a way to create flexible documents that contain the most relevant and timely core health information about a patient, and to send these electronically from one caregiver to another. It contains various sections such as patient demographics, insurance information, diagnosis and problem list, medications, allergies and care plan. These represent a "snapshot" of a patient's health data that can be useful or possibly lifesaving, if available at the time of clinical encounter. Clinical Document Architecture - an XML based markup standard intended to specify the encoding, structure and semantics of clinical documents for exchange Under the Information Technology Management Reform Act (Public Law 104-106), the Secretary of Commerce approves standards and guidelines that are developed by the National Institute of Standards and Technology (NIST) for Federal computer systems. These standards and guidelines are issued by NIST as Federal Information Processing Standards (FIPS) for use government-wide. NIST develops FIPS when there are compelling Federal government requirements such as for security and interoperability and there are no acceptable industry standards or solutions. The American National Standards Institute (ANSI) Healthcare Information Technology Standards Panel; a body created in 2005 in an effort to promote interoperability and harmonization of healthcare information technology through standards that would serve as a cooperative partnership between the public and private sectors. Health Level Seven International (HL7) is a not-for-profit, ANSI-accredited standards developing organization dedicated to providing a comprehensive framework and related standards for the exchange, integration, sharing, and retrieval of electronic health information that supports clinical practice and the management, delivery and evaluation of health services. Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Source http://wiki.siframework.org/ ToC+Glossary+of+Terms http://wiki.siframework.org/ ToC+Glossary+of+Terms http://wiki.siframework.org/ ToC+Glossary+of+Terms http://www.itl.nist.gov/fipsp ubs/geninfo.htm http://wiki.siframework.org/ ToC+Glossary+of+Terms http://www.hl7.org/about Page 28 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Acronym LOINC OIP SNOMED-CT Definition of Acronym Source Logical Observation Identifiers Names and Codes (LOINC) is a database and universal standard for identifying medical laboratory observations. It was developed and is maintained by the Regenstrief Institute, a US non-profit medical research organization, in 1994. LOINC was created in response to the demand for an electronic database for clinical care and management and is publicly available at no cost. http://wiki.siframework.org/ ToC+Glossary+of+Terms ONC Initiative Partner (commonly referred to as OIP) is any organization involved in the following ONC programs: State HIE Programs, Beacon Communities, Challenge Grantees, Standards and Interoperability (S&I) Framework. Systemized Nomenclature of Medicine - is a systematically organized computer processable collection of medical terminology covering most areas of clinical information such as diseases, findings, procedures, microorganisms, pharmaceuticals etc. http://wiki.siframework.org/ ToC+Glossary+of+Terms http://wiki.siframework.org/ ToC+Glossary+of+Terms 7. Appendix C – Recommended Value Sets This appendix contains recommended value sets drawn from work with the Health IT Standards Committee, Beacon Communities, and State HIE programs. These value sets have also been drawn from the Consolidated CDA Guide and its supporting value sets. The following rules apply in the use of these value sets: Wherever possible, this guidance will adhere to the recommendations of the Health IT Standards Committee on vocabularies and controlled terminologies. In those cases where a value set that aligns to these recommendations cannot be found, an alternative value set is proposed that may use a different vocabulary. Implementers from the ONC Beacon Communities and ONC State HIE Programs (sometimes referred to as ONC Initiative Partners, or OIPs) have provided value set recommendations in some areas where implementers wish to provide a set of most commonly used codes In almost all cases, the value set adopted has been aligned to the Consolidated CDA Guide. Advance Directive Type Recommended Value Set In alignment with the CDA Consolidation Guide, the Transitions of Care Initiative recommends the following value set for coding Advance Directive types. Code 52765003 61420007 71388002 78823007 Name Intubation Tube Feedings Other Directive Life Support Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 29 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Code 89666000 225204009 281789004 304251008 Name CPR IV Fluid and Support Antibiotics Resuscitation Allergy/Adverse Event Food and Other Allergens Value Set The value set for coding Food and other allergens in a care transition is to use any ingredient name drawn from the FDA Structured Product Labeling (SPL) subset NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Allergy/Adverse Event Reaction Value Set Any problem drawn from the VA/KP Problem List Subset of SNOMED CT may be used. This set of SNOMED terms and codes is freely reusable worldwide without licensing or intellectual property restrictions. http://evs.nci.nih.gov/ftp1/FDA/ProblemList/ NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Allergy/Adverse Event Type Value Set The value set used to code for allergy and/or adverse event type in a care transition uses the following list of SNOMED-CT concept codes, which describe the type of product and intolerance suffered by the patient: Concept Name Propensity to adverse reactions (disorder) Propensity to adverse reactions to substance (disorder) Propensity to adverse reactions to drug (disorder) Propensity to adverse reactions to food (disorder) Allergy to substance (disorder) Drug allergy (disorder) Drug intolerance (disorder) Food intolerance (disorder) Propensity to adverse reactions (disorder) Concept Code (SNOMED-CT) 420134006 418038007 419511003 418471000 419199007 416098002 59037007 235719002 420134006 NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Care Transition – Body Site Value Set The value set for representing a Body Site in a care transition contains values descending from the SNOMED-CT Anatomical Structure (91723000) hierarchy or Acquired body structure (body structure) (280115004) or Anatomical site notations for tumor staging (body structure) (258331007) or Body structure, altered from its Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 30 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology original anatomical structure (morphologic abnormality) (118956008) or Physical anatomical entity (body structure) (91722005) This indicates the anatomical site. The Body Site value set can be accessed directly from NLM UMLS at the following location: http://www.nlm.nih.gov/research/umls/Snomed/snomed_main.html NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Care Transition – Contact Type Value Set For a care transition, the value set to use for identifying family relationships is the HL7 RoleClassCode. This represents the type of individual support provided, such as immediate emergency contacts, next of kin, family relations, guardians, agents, et cetera HL7 RoleClass Code PRS NOK CAREGIVER AGNT GUAR ECON Usage Note personal relationship next of kin caregiver agent guarantor emergency contact Care Transition – Country Value Set The value set for coding a country is to use any ISO 3166-1 Codes for the representation of names of countries and their subdivisions: Part 1 Countries. The codes are available here: http://www.iso.org/iso/country_codes/iso_3166_code_lists.htm NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Care Transition – Medication Brand Name Value Set The value set for a Medication Brand Name in a care transition uses any RxNorm normal forms for concepts type of Brand Name or Brand Name Packs. The Brand name concepts can be found in the RxNORM file RXCONSO.RRF selecting all terms where SAB=RXNORM (selecting the normal forms), and TTY=BN (selecting the brand names) or TTY=BPCK (selecting the brand name packs) NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Care Transition - Medication Clinical Drug Name Value Set The value set for a Medication Clinical Drug Name in a care transition uses any RxNorm normal forms for concepts type of Ingredient Name or Generic Packs. Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 31 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology The ingredient name concepts can be found in the RxNORM file RXCONSO.RRF selecting all terms where SAB=RXNORM (selecting the normal forms), and TTY=IN (selecting the ingredient names) or TTY=GPCK (selecting the generic packs) NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Care Transition - Medication Drug Class Value Set The value set for a care transition is to use any NDF-RT Code drawn from the following NDF-RT SPL Subsets: Mechanism of Action Physiologic Effect Structural Class These subsets can be accessed at the following location: http://evs.nci.nih.gov/ftp1/FDA/ndfrt/ NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Care Transition – Patient Class Value Set NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Concept Code Concept Name EMER Emergency IMP Inpatient Encounter AMB Ambulatory Definition A patient encounter that takes place at a dedicated healthcare service delivery location where the patient receives immediate evaluation and treatment, provided until the patient can be discharged or responsibility for the patient's care is transferred elsewhere (for example, the patient could be admitted as an inpatient or transferred to another facility.) A patient encounter where a patient is admitted by a hospital or equivalent facility, assigned to a location where patients generally stay at least overnight and provided with room, board, and continuous nursing service A comprehensive term for healthcare provided in a healthcare facility (e.g., a practitioners office, clinic setting, or hospital) on a nonresident basis. The term ambulatory usually implies that the patient has come to the location and is not assigned to a bed. Sometimes referred to as an outpatient encounter Care Transition – Postal Code Value Set The value set for a postal code in a care transition is to use any United States Postal Service (USPS) postal code. The codes are available here: http://zip4.usps.com/zip4/welcome.jsp NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 32 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Care Transition - Problem Value Set The Health IT Standards Committee recommends the use of SNOMED-CT to capture problems. It is expected, howver, that during a care transition, there may be multiple codes used from different terminologies, including ICD-9 and ICD-10. The value set specified for Problems in a care transition is based off SNOMED-CT and includes ICD-9 and ICD-10 codes for common problems. For SNOMED-CT, the value set is limited to terms descending from the Clinical Findings (404684003) or Situation with Explicit Context (243796009) hierarchies. This value set is not intended to be comprehensive but represents the recommendations for specific codes that are common to an active problem list. Implementers should note that a list of ICD-9, ICD-10 and SNOMED-CT codes are provided for commonly used problems. Figure 1: Care Transition – Problem Value Set Table Problem Name Acute Respiratory Failure Asthma Chronic Kidney Disease Congestive Heart Failure COPD Cystic Fibrosis Depression screening Diabetes Diabetes Diabetes Problem Codes Code Set 518.84 ICD-9 493.0, 493.1, 493.2, 493.8, 493.9, 495.8 585.1-6 428 496 277.00, 277.01, 277.02, 277.03, 277.09 V79.0 250, 250.0, 250.00, 250.01, 250.02, 250.03, 250.10, 250.11, 250.12, 250.13, 250.20, 250.21, 250.22, 250.23, 250.30, 250.31, 250.32, 250.33, 250.4, 250.40, 250.41, 250.42, 250.43, 250.50, 250.51, 250.52, 250.53, 250.60, 250.61, 250.62, 250.63, 250.7, 250.70, 250.71, 250.72, 250.73, 250.8, 250.80, 250.81, 250.82, 250.83, 250.9, 250.90, 250.91, 250.92, 250.93, 357.2, 362.0, 362.01, 362.02, 362.03, 362.04, 362.05, 362.06, 362.07, 366.41, 648.0, 648.00, 648.01, 648.02, 648.03, 648.04 31, E10.36, E11.36, E11.9, E13, E13.32, E13.33, E13.34, E13.35, E13.43, O24.42 111552007, 111558006, 11530004, 123763000, 127013003, 127014009, 190321005, 190328004, 190330002, 190331003, 190336008, 190353001, 190361006, 190368000, 190369008, 190371008, 190372001, 190383005, 190389009, 190390000, 190392008, 190406000, 190407009, 190410002, 190411003, 190412005, 190416001, 190417004, 190418009, 190419001, 190422004, 193184006, 197605007, 198609003, 199223000, 199227004, 199229001, 199230006, 199231005, 199234002, 201250006, 201251005, 201252003, 23045005, 230572002, 230577008, 237599002, 237600004, 237601000, 237604008, 237613005, 237618001, 237619009, 237627000, 25907005, 26298008, 267379000, 267380002, 2751001, 275918005, 28032008, 28453007, 290002008, 309426007, 310387003, 311366001, 312912001, 313435000, 313436004, 314537004, 314771006, 314772004, 314893005, 314902007, 314903002, 33559001, 34140002, 359611005, 359638003, 359642000, 360546002, 371087003, 38542009, 39058009, 39181008, 408539000, 408540003, 413183008, 414890007, 414906009, Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 ICD-9 ICD-9 ICD-9 ICD-9 ICD-9 ICD-9 ICD-9 ICD-10 SNOMEDCT Page 33 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Problem Name Diabetes (Exclusion) Diabetic Retinopathy Diabetic Retinopathy Diabetic Retinopathy Emphysema Gestational Diabetes Gestational Diabetes Gestational Diabetes Hypertension Hyperlipidemia Ischemic Vascular Disease Microalbuminuria Nephropathy Nephropathy Nephropathy Problem Codes 420414003, 420422005, 421750000, 421847006, 421895002, 422183001, 422228004, 422275004, 423263001, 424736006, 424989000, 425159004, 425442003, 426705001, 426875007, 427089005, 428896009, 42954008, 44054006, 4627003, 46635009, 50620007, 51002006, 5368009, 54181000, 57886004, 59079001, 5969009, 70694009, 73211009, 74263009, 75524006, 75682002, 76751001, 81531005, 81830002, 8801005, 91352004, 9859006 648.8, 249, 251.8, 962 E10.3, E10.31, E10.311, E10.319, E11.31, E11.311, E11.319, E11.32, E11.321, E11.329, E11.33, E11.331, E11.339, E11.34, E11.341, E11.349 193349004, 193350004, 232020009, 232021008, 232022001, 232023006, 25093002, 25412000, 311782002, 312903003, 312904009, 312905005, 312906006, 312907002, 312908007, 312909004, 312912001, 314010006, 314011005, 314014002, 314015001, 390834004, 399625000, 399862001, 399863006, 399864000, 399865004, 399866003, 399868002, 399869005, 399870006, 399871005, 399872003, 399873008, 399874002, 399875001, 399876000, 399877009, 408409007, 408410002, 408411003, 408412005, 408413000, 408414006, 408415007, 408416008, 414892004, 414894003, 414908005, 414910007, 417677008, 420486006, 420789003, 421779007, 422034002, 4855003, 59276001, 62585004 362.01, 362.02, 362.03, 362.04, 362.05, 362.06 491.20-491.22, 518.20, 506.4, 518.1, 998.81, 958.7 648.8, 648.80, 648.81, 648.82, 648.83, 648.84 R73.02, R73.09 11687002, 420491007, 420738003, 420989005, 421223006, 421389009, 421443003, 422155003, 46894009, 71546005, 75022004 401.-405.XX 272.X 411, 413, 414.0, 414.2, 414.8, 414.9, 429.2, 433-434, 440.1, 440.2, 440.4, 444, 445 791.0 250.4, 250.40, 250.41, 250.42, 250.43, 403, 403.0, 403.00, 403.01, 403.1, 403.10, 403.11, 403.9, 403.90, 403.91, 404, 404.0, 404.00, 404.01, 404.02, 404.03, 404.1, 404.10, 404.11, 404.12, 404.13, 404.9, 404.90, 404.91, 404.92, 404.93, 405.01, 405.11, 405.91, 580, 580.0, 580.4, 580.8, 580.81, 580.89, 580.9, 581, 581.0, 581.1, 581.2, 581.3, 581.8, 581.81, 581.89, 581.9, 582, 582.0, 582.1, 582.2, 582.4, 582.8, 582.81, 582.89, 582.9, 583, 583.0, 583.1, 583.2, 583.4, 583.6, 583.7, 583.8, 583.81, 583.89, 583.9, 584, 584.5, 584.6, 584.7, 584.8, 584.9, 585, 585.1, 585.2, 585.3, 585.4, 585.5, 585.6, 585.9, 586, 587, 588, 588.0, 588.1, 588.8, 588.81, 588.89, 588.9, 753.0, 753.1, 753.10, 753.11, 753.12, 753.13, 753.14, 753.15, 753.16, 753.17, 753.19, 791.0, V42.0, V45.1, V45.11, V45.12, V56, V56.0, V56.1, V56.2, V56.3, V56.31, V56.32, V56.8 G56, G56.8, G56.80, G56.81, G56.82, G56.9, G56.90, G56.91, G56.92, G57, G57.8, G57.80, G57.81, G57.82, G57.9, G57.90, G57.91, G57.92, G58, G58.0, G58.7, G58.8, G58.9, G59, G61, G61.0, G61.1, G61.8, G61.81, G61.89, G61.9, G62, G62.0, G62.9 193003, 290006, 1426004, 1592005, 1776003, 2900003, 3321001, 4292005, 4390004, 4451004, 4495005, 4576001, 4676006, 5397007, Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Code Set ICD-9 ICD-10 SNOMEDCT ICD-9 ICD-9 ICD-9 ICD-10 SNOMEDCT ICD-9 ICD-9 ICD-9 ICD-9 ICD-9 ICD-10 SNOMEDCT Page 34 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Problem Name Problem Codes 5753006, 6134000, 7703001, 7724006, 8199003, 8436004, 8468007, 8964003, 8996006, 9918001, 10123006, 10697004, 10833000, 11013005, 11026009, 11109001, 11659006, 12897005, 13010001, 13335004, 13530005, 13886001, 13889008, 14178006, 14343001, 14669001, 14853005, 14973001, 15842009, 16147005, 16297002, 16507009, 16652001, 16756008, 16934004, 17121006, 17380002, 17901006, 18417009, 18796000, 19351000, 20341008, 20483002, 20917003, 21764004, 21952001, 22011005, 22702000, 22846003, 23697004, 23754003, 24790002, 25646005, 25765006, 25821008, 26235008, 26367008, 27174002, 28196006, 28545001, 28770003, 28918009, 29908007, 30124006, 30275001, 30295007, 31005002, 32093003, 32278006, 32659003, 32916005, 33561005, 33763006, 34165000, 35455006, 35546006, 36171008, 36184004, 36225005, 36388008, 36402006, 36473002, 36568005, 36689008, 36891003, 37133005, 37183000, 37891007, 38481006, 39018007, 39291006, 39734002, 40095003, 40233000, 40488004, 40894000, 41305006, 41729002, 41962002, 42399005, 42496002, 42927005, 43064006, 43258006, 43629001, 43738009, 44323002, 44513007, 44730006, 45281005, 45456005, 45646000, 45743004, 45812003, 45816000, 46177005, 46395002, 48061001, 48631008, 48638002, 48655003, 48713002, 48796009, 49008000, 49220004, 49809007, 50581000, 50909009, 51055000, 51292008, 51677000, 52042003, 52254009, 52342006, 52777008, 52845002, 53378008, 53556002, 54155004, 54181000, 54480007, 54781007, 54879000, 54967001, 55006001, 55536001, 55655006, 55856005, 56108007, 56346006, 57088004, 57469000, 57557005, 57684003, 57965003, 58276006, 58574008, 58797008, 59400006, 59530001, 59758007, 59780005, 60989005, 61474001, 61598006, 61680002, 61852001, 62216007, 62240004, 63510008, 64323009, 65127006, 65443008, 66993009, 67132008, 68815009, 69718008, 70092007, 71064009, 71110009, 71275003, 71909003, 72613009, 73030000, 73286009, 73305009, 74594005, 75030003, 75150001, 75652008, 75712001, 76224000, 76521009, 76910007, 77186001, 77624000, 77945009, 78209002, 78311009, 78544004, 79385002, 80902009, 81363003, 81896006, 81986001, 81987005, 82525005, 83563007, 83850008, 83866005, 84121007, 85020001, 85487008, 85901000, 86210009, 86234004, 86235003, 86249007, 86463003, 86564006, 87571007, 88102009, 88380005, 88531004, 90241004, 90493000, 90688005, 90708001, 91003006, 92165001, 92624000, 92921005, 92975004, 93290000, 93425004, 94889006, 95444008, 95474000, 95568003, 95570007, 95571006, 95572004, 95575002, 95577005, 95578000, 95579008, 95580006, 95582003, 95889002, 102455002, 105999006, 106000008, 109477002, 110996009, 111395007, 111403005, 111404004, 111406002, 111407006, 112066009, 118951003, 123609007, 123610002, 123611003, 123612005, 123752003, 123753008, 123755001, 124147007, 126874009, 126880001, 126881002, 127013003, 128996006, 129128006, 168041003, 187144000, 188250002, 188251003, 194774006, 194780003, 194781004, 197577008, 197589005, 197590001, 197591002, 197593004, 197594005, 197595006, 197596007, 197597003, 197598008, 197599000, 197600002, 197601003, 197603000, 197605007, 197606008, 197607004, 197627003, 197628008, 197629000, Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Code Set Page 35 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Problem Name Problem Codes 197650009, 197659005, 197660000, 197661001, 197663003, 197664009, 197670003, 197671004, 197679002, 197688006, 197707007, 197708002, 197712008, 197738008, 197739000, 197752005, 197753000, 197801000, 197802007, 197813005, 197817006, 197820003, 198841006, 198842004, 198843009, 198844003, 198845002, 198846001, 198949009, 199110003, 199132007, 199134008, 199135009, 199136005, 199137001, 200117009, 200118004, 204938007, 204941003, 204942005, 204949001, 204950001, 204957003, 204962002, 204980006, 204984002, 204985001, 210197003, 210207004, 210811000, 213231008, 226309007, 230970001, 236367002, 236369004, 236374007, 236376009, 236377000, 236380004, 236381000, 236382007, 236383002, 236384008, 236385009, 236395002, 236402009, 236403004, 236404005, 236405006, 236406007, 236423003, 236424009, 236425005, 236428007, 236429004, 236430009, 236431008, 236432001, 236433006, 236434000, 236435004, 236436003, 236437007, 236438002, 236439005, 236441006, 236442004, 236443009, 236444003, 236445002, 236448000, 236452000, 236453005, 236454004, 236455003, 236456002, 236457006, 236460004, 236461000, 236463002, 236464008, 236467001, 236469003, 236470002, 236471003, 236472005, 236474006, 236475007, 236477004, 236478009, 236479001, 236480003, 236481004, 236482006, 236483001, 236484007, 236485008, 236486009, 236487000, 236488005, 236490006, 236491005, 236492003, 236493008, 236495001, 236498004, 236499007, 236500003, 236502006, 236503001, 236504007, 236505008, 236506009, 236507000, 236508005, 236511006, 236514003, 236515002, 236516001, 236517005, 236518000, 236519008, 236520002, 236521003, 236522005, 236523000, 236526008, 236527004, 236528009, 236530006, 236531005, 236532003, 236534002, 236535001, 236569000, 236570004, 236583003, 236584009, 236586006, 236587002, 236590008, 236592000, 236614007, 236708007, 236710009, 236713006, 237230004, 239932005, 240317003, 253860008, 253862000, 253864004, 253865003, 253866002, 253867006, 253869009, 253872002, 253875000, 253876004, 253881008, 253883006, 253886003, 254914004, 254915003, 254916002, 254919009, 254920003, 254922006, 254923001, 254924007, 262612001, 262891006, 262893009, 262894003, 262900003, 266549004, 266556005, 267430007, 268232000, 268234004, 268854008, 269257004, 269301005, 269489006, 270494003, 270517006, 271387005, 271432005, 274401005, 275408006, 275510005, 276583007, 276584001, 276585000, 276586004, 276627004, 277010001, 277011002, 278531007, 282348002, 282664001, 283905005, 288004005, 289923007, 298127003, 301814009, 302233006, 302849000, 302910002, 302922004, 307309005, 307532008, 307604008, 307618001, 309426007, 309785008, 310387003, 311366001, 311496007, 359563005, 361146001, 361147005, 361264003, 363224005, 363234001, 363287001, 363288006, 363518003, 367540006, 370488005, 370493008, 370494002, 371011007, 371019009, 371020003, 373421000, 373422007, 373584008, 373585009, 373599008, 399094007, 399190000, 399340005, 405573009, 405584002, 420279001, 421893009, 422593004, 423322005, 423533009, 423919000, 425369003, 425384007, 425414000, 425455002, 426136000, 427555000, 427649000, 428255004, 428720002, 429224003, 429489008, 430535006, 431480000, 431501001, 431855005, 431856006, 431857002, 432294000, 432461000, 433036004, 433144002, 433146000, 433229006, 438783006, 439990003, 440018001, 441815006 Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Code Set Page 36 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Problem Name Obesity Polycystic ovaries Polycystic ovaries 278 256.4 E28.2 Polycystic ovaries 69878008 Pregnancy (normal) Problem Codes Code Set ICD-9 ICD-9 ICD-10 SNOMEDCT 630, 631, 632, 633.00, 633.01, 633.10, 633.11, 633.20, 633.21, 633.80, 633.81, 633.90, 633.91, 634.00, 634.01, 634.02, 634.10, 634.11, 634.12, 634.20, 634.21, 634.22, 34.30, 634.31, 634.32, 634.40, 634.41, 634.42, 634.50, 634.51, 634.52, 634.60, 634.61, 634.62, 634.70, 634.71, 634.72, 634.80, 634.81, 634.82, 634.90, 634.91, 634.92, 635.00, 635.01, 635.02, 635.10, 635.11, 635.12, 635.20, 635.21, 635.22, 635.30, 635.31, 635.32, 635.40, 635.41, 635.42, 635.50, 635.51, 635.52, 635.60, 635.61, 635.62, 635.70, 635.71, 635.72, 635.80, 635.81, 635.82, 635.90, 635.91, 635.92, 636.00, 636.01, 636.02, 636.10, 636.11, 636.12, 636.20, 636.21, 636.22, 636.30, 636.31, 636.32, 636.40, 636.41, 636.42, 636.50, 636.51, 636.52, 636.60, 636.61, 636.62, 636.70, 636.71, 636.72, 636.80, 636.81, 636.82, 636.90, 636.91, 636.92, 637.00, 637.01, 637.02, 637.10, 637.11, 637.12, 637.20, 637.21, 637.22, 637.30, 637.31, 637.32, 637.40, 637.41, 637.42, 637.50, 637.51, 637.52, 637.60, 637.61, 637.62, 637.70, 637.71, 637.72, 637.80, 637.81, 637.82, 637.90, 637.91, 637.92, 638.0, 638.1, 638.2, 638.3, 638.4, 638.5, 638.6, 638.7, 638.8, 638.9, 639.0, 639.1, 639.2, 639.3, 639.4, 639.5, 639.6, 639.8, 639.9, 640.00, 640.01, 640.03, 640.80, 640.81, 640.83, 640.90, 640.91, 640.93, 641.00, 641.01, 641.03, 641.10, 641.11, 641.13, 641.20, 641.21, 641.23, 641.30, 641.31, 641.33, 641.80, 641.81, 641.83, 641.90, 641.91, 641.93, 642.00, 642.01, 642.02, 642.03, 642.04, 642.10, 642.11, 642.12, 642.13, 642.14, 642.20, 642.21, 642.22, 642.23, 642.24, 642.30, 642.31, 642.32, 642.33, 642.34, 642.40, 642.41, 642.42, 642.43, 642.44, 642.50, 642.51, 642.52, 642.53, 642.54, 642.60, 642.61, 642.62, 642.63, 642.64, 642.70, 642.71, 642.72, 642.73, 642.74, 642.90, 642.91, 642.92, 642.93, 642.94, 643.00, 643.01, 643.03, 643.10, 643.11, 643.13, 643.20, 643.21, 643.23, 643.80, 643.81, 643.83, 643.90, 643.91, 643.93, 644.00, 644.03, 644.10, 644.13, 644.20, 644.21, 645.10, 645.11, 642.13, 645.20, 645.21, 645.23, 646.00, 646.01, 646.03, 646.10, 646.11, 646.12, 646.13, 646.14, 646.20, 646.21, 646.22, 646.23, 646.24, 646.30, 646.31, 646.33, 646.40, 646.41, 646.42, 646.43, 646.44, 646.50, 646.51, 646.52, 646.53, 646.54, 646.60, 646.61, 646.62, 646.63, 646.64, 646.70, 646.71, 646.73, 646.80, 646.81, 646.82, 646.83, 646.84, 646.90, 646.91, 646.93, 647.00, 647.01, 647.02, 647.03, 647.04, 647.10, 647.11, 647.12, 647.13, 647.14, 647.20, 647.21, 647.22, 647.23, 647.24, 647.30, 647.31, 647.32, 647.33, 647.34, 647.40, 647.41, 647.42, 647.43, 647.44, 647.50, 647.51, 647.52, 647.53, 647.54, 647.60, 647.61, 647.62, 647.63, 647.64, 647.80, 647.81, 647.82, 647.83, 647.84, 647.90, 647.91, 647.92, 647.93, 647.94, 648.00, 648.01, 648.02, 648.03, 648.04, 648.10, 648.11, 648.12, 648.13, 648.14, 648.20, 648.21, 648.22, 648.23, 648.24, 648.30, 648.31, 648.32, 648.33, 648.34, 648.40, 648.41, 648.42, 648.43, 648.44, 648.50, 648.51, 648.52, 648.53, 648.54, 648.60, 648.61, 648.62, 648.63, 648.64, 648.70, 648.71, 648.72, 648.73, 648.74, 648.80, 648.81, 648.82, 648.83, 648.84, 648.90, 648.91, 648.92, 648.93, 648.94, 649.00, 649.01, 649.02, 649.03, 649.04, 649.10, 649.11, 649.12, 649.13, 649.14, 649.20, 649.21, 649.22, 649.23, 649.24, 649.30, 649.31, 649.32, 649.33, 649.34, 649.40, Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 ICD-9 Page 37 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Problem Name Problem Codes 649.41, 649.42, 649.43, 649.44, 649.50, 649.51, 649.53, 649.60, 649.61, 649.62, 649.63, 649.64, 649.70, 649.71, 649.73, 650, 651.00, 651.01, 651.03, 651.10, 651.11, 651.13, 651.20, 651.21, 651.23, 651.30, 651.31, 651.33, 651.40, 651.41, 651.43, 651.50, 651.51, 651.53, 651.60, 651.61, 651.63, 651.70, 651.71, 651.73, 651.80, 651.81, 651.83, 651.90, 651.91, 651.93, 652.00, 652.01, 652.03, 652.10, 652.11, 652.13, 652.20, 652.21, 652.23, 652.30, 652.31, 652.33, 652.40, 652.41, 652.43, 652.50, 652.51, 652.53, 652.60, 652.61, 652.63, 652.70, 652.71, 652.73, 652.80, 652.81, 652.83, 652.90, 652.91, 652.93, 653.00, 653.01, 653.03, 653.10, 653.11, 653.13, 653.20, 653.21, 653.23, 653.30, 653.31, 653.33, 653.40, 653.41, 653.43, 653.50, 653.51, 653.53, 653.60, 653.61, 653.63, 653.70, 653.71, 653.73, 653.80, 653.81, 653.83, 653.90, 653.91, 653.93, 654.00, 654.01, 654.02, 654.03, 654.04, 654.10, 654.11, 654.12, 654.13, 654.14, 654.20, 654.21, 654.23, 654.30, 654.31, 654.32, 654.33, 654.34, 654.40, 654.41, 654.42, 654.43, 654.44, 654.50, 654.51, 654.52, 654.53, 654.54, 654.60, 654.61, 654.62, 654.63, 654.64, 654.70, 654.71, 654.72, 654.73, 654.74, 654.80, 654.81, 654.82, 654.83, 654.84, 654.90, 654.91, 654.92, 654.93, 654.94, 655.00, 655.01, 655.03, 655.10, 655.11, 655.13, 655.20, 655.21, 655.23, 655.30, 655.31, 655.33, 655.40, 655.41, 655.43, 655.50, 655.51, 655.53, 655.60, 655.61, 655.63, 655.70, 655.71, 655.73, 655.80, 655.81, 655.83, 655.90, 655.91, 655.93, 656.00, 656.01, 656.03, 656.10, 656.11, 656.13, 656.20, 656.21, 656.23, 656.30, 656.31, 656.33, 656.40, 656.41, 656.43, 656.50, 656.51, 656.53, 656.60, 656.61, 656.63, 656.70, 656.71, 656.73, 656.80, 656.81, 656.83, 656.90, 656.91, 656.93, 657.00, 657.01, 657.03, 658.00, 658.01, 658.03, 658.10, 658.11, 658.13, 658.20, 658.21, 658.23, 658.30, 658.31, 658.33, 658.40, 658.41, 658.43, 658.80, 658.81, 658.83, 658.90, 658.91, 658.93, 659.00, 659.01, 659.03, 659.10, 659.11, 659.13, 659.20, 659.21, 659.23, 659.30, 659.31, 659.33, 659.40, 659.41, 659.43, 659.50, 659.51, 659.53, 659.60, 659.61, 659.63, 659.70, 659.71, 659.73, 659.80, 659.81, 659.83, 659.90, 659.91, 659.93, 660.00, 660.01, 660.03, 660.10, 660.11, 660.13, 660.20, 660.21, 660.23, 660.30, 660.31, 660.33, 660.40, 660.41, 660.43, 660.50, 660.51, 660.53, 660.60, 660.61, 660.63, 660.70, 660.71, 660.73, 660.80, 660.81, 660.83, 660.90, 660.91, 660.93, 661.00, 661.01, 661.03, 661.10, 661.11, 661.13, 661.20, 661.21, 661.23, 661.30, 661.31, 661.33, 661.40, 661.41, 661.43, 661.90, 661.91, 661.93, 662.00, 662.01, 662.03, 662.10, 662.11, 662.13, 662.20, 662.21, 662.23, 662.30, 662.31, 662.33, 663.00, 663.01, 663.03, 663.10, 663.11, 663.13, 663.20, 663.21, 663.23, 663.30, 663.31, 663.33, 663.40, 663.41, 663.43, 663.50, 663.51, 663.53, 663.60, 663.61, 663.63, 663.80, 663.81, 663.83, 663.90, 663.91, 663.93, 664.00, 664.01, 664.04, 664.10, 664.11, 664.14, 664.20, 664.21, 664.24, 664.30, 664.31, 664.34, 664.40, 664.41, 664.44, 664.50, 664.51, 664.54, 664.60, 664.61, 664.64, 664.80, 664.81, 664.84, 664.90, 664.91, 664.94, 665.00, 665.01, 665.03, 665.10, 665.11, 665.20, 665.22, 665.24, 665.30, 665.31, 665.34, 665.40, 665.41, 665.44, 665.50, 665.51, 665.54, 665.60, 665.61, 665.64, 665.70, 665.71, 665.72, 665.74, 665.80, 665.81, 665.82, 665.83, 665.84, 665.90, 665.91, 665.92, 665.93, 665.94, 666.00, 666.02, 666.04, 666.10, 666.12, 666.14, 666.20, 666.22, 666.24, 666.30, 666.32, 666.34, 667.00, 667.02, 667.04, 667.10, 667.12, 667.14, 668.00, 668.01, 668.02, 668.03, 668.04, 668.10, 668.11, 668.12, 668.13, 668.14, 668.20, 668.21, 668.22, 668.23, 668.24, 668.80, Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Code Set Page 38 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Problem Name PregProblem nancy (normal) Steroid Induced Diabetes Steroid Induced Diabetes Steroid Induced Diabetes Steroid Induced Diabetes Tobacco Use Problem Codes 668.81, 668.82, 668.83, 668.84, 668.90, 668.91, 668.92, 668.93, 668.94, 669.00, 669.01, 669.02, 669.03, 669.04, 669.10, 669.11, 669.12, 669.13, 669.14, 669.20, 669.21, 669.22, 669.23, 669.24, 669.30, 669.32, 669.34, 669.40, 669.41, 669.42, 669.43, 669.44, 669.50, 669.51, 669.60, 669.61, 669.70, 669.71, 669.80, 669.81, 669.82, 669.83, 669.84, 669.90, 669.91, 669.92, 669.93, 669.94, 670.00, 670.02, 670.04, 670.10, 670.12, 670.14, 670.20, 670.22, 670.24, 670.30, 670.32, 670.34, 670.80, 670.82, 670.84, 671.00, 671.01, 671.02, 671.03, 671.04, 671.10, 671.11, 671.12, 671.13, 671.14, 671.20, 671.21, 671.22, 671.23, 671.24, 671.30, 671.31, 671.33, 671.40, 671.42, 671.44, 671.50, 671.51, 671.52, 671.53, 671.54, 671.80, 671.81, 671.82, 671.83, 671.84, 671.90, 671.91, 671.92, 671.93, 671.94, 672.00, 672.02, 672.04, 673.00, 673.01, 673.02, 673.03, 673.04, 673.10, 673.11, 673.12, 673.13, 673.14, 673.20, 673.21, 673.22, 673.23, 673.24, 673.30, 673.31, 673.32, 673.33, 673.34, 673.80, 673.81, 673.82, 673.83, 673.84, 674.00, 674.01, 674.02, 674.03, 674.04, 674.10, 674.12, 674.14, 674.20, 674.22, 674.24, 674.30, 674.32, 674.34, 674.40, 674.42, 674.44, 674.50, 674.51, 674.52, 674.53, 674.54, 674.80, 674.82, 674.84, 674.90, 674.92, 674.94, 675.00, 675.01, 675.02, 675.03, 675.04, 675.10, 675.11, 675.12, 675.13, 675.14, 675.20, 675.21, 675.22, 675.23, 675.24, 675.80, 675.81, 675.82, 675.83, 675.84, 675.90, 675.91, 675.92, 675.93, 675.94, 676.00, 676.01, 676.02, 676.03, 676.04, 676.10, 676.11, 676.12, 676.13, 676.14, 676.20, 676.21, 676.22, 676.23, 676.24, 676.30, 676.31, 676.32, 676.33, 676.34, 676.40, 676.41, 676.42, 676.43, 676.44, 676.50, 676.51, 676.52, 676.53, 676.54, 676.60, 676.61, 676.62, 676.63, 676.64, 676.80, 676.81, 676.82, 676.83, 676.84, 676.90, 676.91, 676.92, 676.93, 676.94, V22.0, V22.1, V22.2, V23.0, V23.1, V23.2, V23.3, V23.41, V23.49, V23.5, V23.7, V23.81, V23.82, V23.83, V23.84, V23.85, V23.86, V23.89, V23.9, V28.0, V28.1, V28.2, V28.3, V28.4, V28.5, V28.6, V28.81, V28.82, V28.89, V28.9 16356006, 198624007, 198626009, 198627000, 239101008, 289908002, 31601007, 34801009, 38720006, 41991004, 43990006, 44782008, 60000008, 60810003, 64254006, 65147003, 69532007, 79290002, 79586000, 80997009, 82661006, 87605005, 90968009, 9899009 249, 249.0 249.00, 249.01, 249.1, 249.10, 249.11, 249.2, 249.20, 249.21, 249.3, 249.30, 249.31, 249.4, 249.40, 249.41, 249.5, 249.50, 249.51, 249.6, 249.60, 249.61, 249.7, 249.70, 249.71, 249.8, 249.80, 249.81, 249.9, 249.90, 249.91, 251.8, 962.0 E08, E10, T38 190416008, 190447002, 53126001 305.1, 649.0x, 989.84 Code Set SNOMEDCT ICD-9 ICD-9 ICD-10 SNOMEDCT ICD-9 Care Transition – Provider Role Value Set The value set for a Provider Role in a care transition uses the HL7 2.5.1 vocabulary specified in the Consolidated CDA Guide for Provider Role. Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 39 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Care Transition – Provider Type Value Set The value set for a Provider Type in a care transition uses the National Uniform Claim Committee (NUCC) Health Care Provider Taxonomy. This Provider Type value set classifies providers according to the type of license or accreditation they hold or the service they provide. The value set can be located here: http://www.nucc.org/index.php?option=com_content&task=view&id=14&Itemid=40 A list of the most common provider types is provided below. At this time, the concept codes are not available from NUCC and this table outlines the high level “Provider Type” classification only: Provider Type Concept Name Behavioral Health & Social Service Providers Chiropractic Providers Dental Providers Dietary and Nutritional Service Providers Emergency Medical Service Providers Eye and Vision Service Providers Nursing Service Providers Pharmacy Service Providers (Individuals) Allopathic & Osteopathic Physicians Podiatric Medicine and Surgery Providers Respiratory, Developmental, Rehabilitative and Restorative Service Providers Definition Broad classification aggregating providers who are trained and educated to perform services related to behavioral health, mental health, and counseling and may be licensed or practice within the scope or licensure or training A provider qualified by a Doctor of Chiropractic (D.C.) licensed by the State and who practices chiropractic medicine -that discipline within the healing arts which deals with the nervous system and its relationship to the spinal column and its interrelationship with other body systems Broad category to identify practitioners who render services related the practice of dentistry. Dentistry is defined as the evaluation, diagnosis, prevention and/or treatment (nonsurgical, surgical or related procedures) of diseases, disorders and/or conditions of the oral cavity, maxillofacial area and/or the adjacent and associated structures and their impact on the human body; provided by a dentist, within the scope of his/her education, training and experience, in accordance with the ethics of the profession and applicable law Broad category defining practitioners who help prevent and treat illness by promoting healthy eating habits, scientifically evaluating diets and suggesting modifications. They may also assess the nutritional needs of patients, develop and implement nutritional care plans Broad category for individuals who complete additional training and education in the area of pre-hospital emergency services and are licensed and/or practice within the scope of that training Broad category grouping individuals who renders services related to the human eye and visual systems, but are not an allopathic or osteopathic physicians Providers who are trained and educated to perform and administer services related to health promotion, disease prevention, acute and chronic care, spiritual guidance and comfort for healing and health, restoration of health and health maintenance across the life span A broad category grouping providers who render services relating to the preparation and dispensing of drugs A broad category grouping state licensed providers in allopathic or osteopathic medicine whose scope of practice is determined by education Broad category grouping licensed providers who renders services related to the human foot A provider who is trained and educated to perform services related to respiratory care, physical therapy, occupational therapy, developmental therapy, rehabilitation and restorative services and may be licensed, certified Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 40 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Provider Type Concept Name Speech, Language and Hearing Providers Agencies Ambulatory Health Care Facilities Hospitals Laboratories Managed Care Organizations Nursing & Custodial Care Facilities Residential Treatment Facilities Suppliers Physician Assistants & Advanced Practice Nursing Providers Nursing Service Related Providers Definition or practice within the scope of training A provider who renders services to improve communicative skills of people with language, speech and hearing impairments A non-facility provider that renders outpatient outreach services that are not provided at a specific location. The licensure or registration is assigned to the agency rather than to the individual practitioners as would be the case in a group practice A facility or distinct part of one used for the diagnosis and treatment of outpatients. "Clinic/Center" is irregularly defined, sometimes being limited to organizations serving specialized treatment requirements or distinct patient/client groups (e.g., radiology, poor, and public health) A healthcare organization that has a governing body, an organized medical staff and professional staff and inpatient facilities and provides medical nursing and related services for ill and injured patients 24 hrs per day, seven days per week. For licensing purposes, each state has its own definition of hospital A room or building equipped for scientific experimentation, research, testing, or clinical studies of materials, fluids, or tissues obtained from patients Not Available Broad category identifying licensed facilities with inpatient beds specializing in nursing and custodial care Live in facilities where patients or clients, who because of their physical, mental, or emotional condition, are not able to live independently, and who receive treatment appropriate to their particular needs in a less restrictive environment than an inpatient facility. For example, an RTC may provide educational training and therapy for children with emotional disturbances or continuing care and therapy for people with severe mental handicaps Suppliers, pharmacies, and other healthcare providers who supply healthcare related products or medications and associated professional and administrative services A broad grouping of providers who are: 1) trained, educated, and certified to perform basic medical and minor surgical services (or to assist the physician in performance of more complex services) under general physician supervision; and 2) trained, educated at a post-graduate level, and certified to perform autonomous and specialized roles as nurse practitioners, midwives, nurse anesthetists, or clinical nurse specialists Providers not otherwise classified, who perform or administer services in or related to the delivery or research of healthcare services, disease, and restoration of health. An individual provider who is not represented in one of the identified categories but whose data may be needed for clinical, operational or administrative processes Care Transition – Relationship Value Set For a care transition, the value set to use for identifying family relationships is the HL7 RoleCode. A Personal Relationship in this value set records the role of a person in relation to another person. This value set is to be used when recording the relationships between different people who are not necessarily related by family ties, but also includes family relationships Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 41 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology HL7 RoleClass Code PRS NOK CAREGIVER AGNT GUAR ECON Usage Note personal relationship next of kin caregiver agent guarantor emergency contact Care Transition - Severity Value Set The value set for severity of an allergy, adverse event or problem in a care transition uses the following list of SNOMED-CT concept codes, that describes the severity being experienced: NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Concept Code 255604002 371923003 6736007 371924009 24484000 399166001 Concept Name (Fully Qualified SNOMED-CT Name) Mild (qualifier value) Mild to moderate (qualifier value) Moderate (severity modifier) (qualifier value) Moderate to severe (qualifier value) Severe (severity modifier) (qualifier value) Fatal (qualifier value) Definition Usage Notes Not Available Not Available Not Available Mild Mild to moderate Moderate Not Available Not Available Moderate to severe Severe Not Available Fatal Care Transition – State Value Set The value set for a coding a state value in a care transition is to use any FIPS 5-2 Codes (Identification of the States, the District of Columbia and the Outlying Areas of the United States, and Associated Areas Publication # 5-2, May, 1987). The codes are available here: http://www.itl.nist.gov/fipspubs/fip5-2.htm NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Health Insurance Subscriber Relationship Value Set NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Concept Code FAMDEP FSTUD HANDIC INJ PSTUD Concept Name Family dependent Full-time student Handicapped dependent Injured plaintiff Part-time student Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 42 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology SELF SPON STUD Self Sponsored dependent Student Health Insurance Type Value Set The current value set specified for Health Insurance Type supports Accredited Standards Committee (ASC) X12 Standards Release 004010. This value set uses the ACS X12 vocabulary for Insurance Type Code (ASC X12 Data Element 1336. NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change NOTE: Further updates of this value set will be needed in support of the HIPAA 5010 transition. Concept Code 12 13 14 15 16 41 42 43 47 AP C1 CO CP D DB EP FF GP HM HN HS IN IP LC LD LI LT MA MB MC MH MI Concept Name Medicare Secondary Working Aged Beneficiary or Spouse with Employer Group Health Plan Medicare Secondary End-Stage Renal Disease Beneficiary in the 12 month coordination period with an employers group health plan Medicare Secondary, No-fault Insurance including Auto is Primary Medicare Secondary Workers Compensation Medicare Secondary Public Health Service (PHS)or Other Federal Agency Medicare Secondary Black Lung Medicare Secondary Veterans Administration Medicare Secondary Disabled Beneficiary Under Age 65 with Large Group Health Plan (LGHP) Medicare Secondary, Other Liability Insurance is Primary Auto Insurance Policy Commercial Consolidated Omnibus Budget Reconciliation Act (COBRA) Medicare Conditionally Primary Disability Disability Benefits Exclusive Provider Organization Family or Friends Group Policy Health Maintenance Organization (HMO) Health Maintenance Organization (HMO) - Medicare Risk Special Low Income Medicare Beneficiary Indemnity Individual Policy Long Term Care Long Term Policy Life Insurance Litigation Medicare Part A Medicare Part B Medicaid Medigap Part A Medigap Part B Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 43 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology Concept Code MP OT PE PL PP PR PS QM RP SP TF WC WU Concept Name Medicare Primary Other Property Insurance – Personal Personal Personal Payment (Cash - No Insurance) Preferred Provider Organization (PPO) Point of Service (POS) Qualified Medicare Beneficiary Property Insurance - Real Supplemental Policy Tax Equity Fiscal Responsibility Act (TEFRA) Workers Compensation Wrap Up Policy Ingredient Name Value Set The value set to identify an ingredient name within a care transition uses unique ingredient identifiers (UNIIs) for substances in drugs, biologics, foods, and devices. The value set can be located here: http://www.fda.gov/ForIndustry/DataStandards/StructuredProductLabeling/ucm162523.htm Immunizations Administered Vaccines Value Set Recommendation The Health IT Standards Committee recommends CVX Codes for vaccinations (acknowledging that vaccinations are treated as medications in some contexts and as a separate category in others). The value set for a care transition uses CVX codes to populate the Coded Product Name in the Immunizations Section of the care transition. This value set provides CVX codes common to a care transition: CVX Code 54 55 24 19 27 26 29 12 28 20 106 110 50 120 130 01 Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Immunization Description Adenovirus, type 4 Adenovirus, type 7 Anthrax BCG Botulinum antitoxin Cholera CMVIG Diphtheria antitoxin DT (pediatric) DTaP DTaP, 5 pertussis antigens DTaP-Hep B-IPV DTaP-Hib DTaP-Hib-IPV DTaP-IPV DTP Page 44 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology CVX Code 22 30 52 83 84 85 104 08 42 43 44 45 47 46 49 48 17 51 62 118 86 14 87 135 111 144 140 141 88 16 10 134 39 66 05 32 136 114 03 94 04 07 Immunization Description DTP-Hib HBIG Hep A, adult Hep A, ped/adol, 2 dose Hep A, ped/adol, 3 dose Hep A, unspecified formulation Hep A-Hep B Hep B, adolescent or pediatric Hep B, adolescent/high risk infant Hep B, adult Hep B, dialysis Hep B, unspecified formulation Hib (HbOC) Hib (PRP-D) Hib (PRP-OMP) Hib (PRP-T) Hib, unspecified formulation Hib-Hep B HPV, quadrivalent HPV, bivalent IG IG, unspecified formulation IGIV Influenza, high dose seasonal Influenza, live, intranasal Influenza, seasonal, intradermal, preservative free Influenza, seasonal, injectable, preservative free Influenza, seasonal, injectable Influenza, unspecified formulation Influenza, whole IPV Japanese Encephalitis IM Japanese encephalitis SC Lyme disease Measles Meningococcal MPSV4 Meningococcal MCV4O Meningococcal MCV4P MMR MMRV M/R Mumps Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 45 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology CVX Code Immunization Description Novel influenza-H1N1-09 Novel Influenza-H1N1-09, all formulations Novel Influenza-H1N1-09, nasal Novel influenza-H1N1-09, preservative-free OPV Plague Pneumococcal conjugate PCV 7 Pneumococcal conjugate PCV 13 Pneumococcal polysaccharide PPV23 Rabies, intramuscular injection Rabies, intradermal injection Rabies, unspecified formulation RIG Rotavirus, pentavalent Rotavirus, monovalent RSV-MAb RSV-IGIV Rubella Td (adult), adsorbed Td (adult) preservative free Tdap Tetanus toxoid, adsorbed TIG Typhoid, oral Typhoid, parenteral Typhoid, parenteral, AKD (U.S. military) Typhoid, unspecified formulation Typhoid, ViCPs Vaccinia immune globulin VZIG Varicella Yellow fever Zoster 127 128 125 126 02 23 100 133 33 18 40 90 34 116 119 93 71 06 09 113 115 35 13 25 41 53 91 101 79 36 21 37 121 Immunization Reason Value Set NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component with the following change Concept Code IMMUNE Concept Name Immunity MEDPREC Medical precaution Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Definition Testing has shown that the patient already has immunity to the agent targeted by the immunization The patient currently has a medical condition for which Page 46 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology OSTOCK Out of sToCk PATOBJ Patient objection PHILISOP Philosophical objection RELIG Religious objection VACEFF Vaccine efficacy concerns VACSAF Vaccine safety concerns the vaccine is contraindicated or for which precaution is warranted There was no supply of the product on hand to perform the service The patient or their guardian objects to receiving the vaccine The patient or their guardian objects to receiving the vaccine because of philosophical beliefs The patient or their guardian objects to receiving the vaccine on religious grounds The intended vaccine has expired or is otherwise believed to no longer be effective Example: Due to temperature exposure Medication Fill Status Value Set NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Concept Code Completed Concept Name Completed Aborted Aborted Definition An Act that has terminated normally after all of its constituents have been performed The Act has been terminated prior to the originally intended completion Medication Method of Delivery Value Set The Centers for Medicare and Medicaid Services (CMS) published to the Federal Register July 1, 2010 an Interim Final Rule (IFR) entitled, "Identification of Backward Compatible Version of Adopted Standard for E-Prescribing and the Medicare Prescription Drug Program (NCPDP SCRIPT 10.6)." The regulation names NCPDP SCRIPT 10.6 effective for use July 1, 2010 and continues to support NCPDP SCRIPT 8.1. Pursuant to this implementation guidance the value set for Medication Method of Delivery in a care transition can use NCPDP Script 10.6 to code values for delivery method. Medication Product Form Value Set This is the physical form of the product as presented to the individual. For example: tablet, capsule, liquid or ointment. The value set specified for a care transition is to use NCI concept code for pharmaceutical dosage form: C42636 NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Medication Route Value Set This indicates the method for the medication received by the individual (e.g., by mouth, intravenously, topically, etc). The value set specified for a care transition is to use NCI concept code for route of administration: C38114 Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 47 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Medication Type Value Set For an Active Medication List (as specified in the Transitions of Care Clinical Information Model ), the value set for Medication Type is based on SNOMED-CT. The following SNOMED-CT concept codes are used: NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Concept Name (Fully Qualified SNOMED-CT Name) Over the counter products (product) Prescription drug (product) Concept Code 329505003 73639000 Usage Note Over the counter products Prescription Drug Problem Status Value Set The Health IT Standards Committee recommends the use of SNOMED-CT to capture problems.For an Active Problem List (as specified in the Transitions of Care Clinical Information Model ), the value set for Problem Status is derived from SNOMED-CT. The following SNOMED-CT concept codes are used: Concept Code Concept Name (Fully Qualified SNOMED-CT Name) 413322009 Resolved 55561003 Active 73425007 Inactive 90734009 7087005 255227004 415684004 410516002 Chronic Intermittent Recurrent Rule out Ruled out Definition The problem has been resolved (as of the time reported) - the problem is one that still exists for the patient but is not currently a cause for concern (e.g., diabetes that is under control) The problem is currently active (as of the time reported) - the problem exists and is a current cause for concern The problem is currently inactive (as of the time reported) - the problem no longer exists as a problem for the patient as of the time of recording (it may reoccur, but that would be a new instance) Problem Type Value Set The Health IT Standards Committee recommends the use of SNOMED-CT to capture problems. For an Active Problem List (as specified in the Transitions of Care Clinical Information Model ), the value set for Problem Type is derived from SNOMED-CT. The following SNOMED-CT concept codes are used: Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 48 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology NOTE: This value set is adopted from HITSP C80 - Clinical Document and Message Terminology Component without change Concept Code 404684003 418799008 55607006 409586006 64572001 282291009 248536006 Concept Name (Fully Qualified SNOMED-CT Name) Clinical finding (finding) Finding reported by subject or history provider (finding) Problem (finding) Complaint (finding) Disease (disorder) Diagnosis interpretation (observable entity) Finding of functional performance and activity (finding) Definition Usage Note Finding Symptom Problem Complaint Condition Diagnosis Functional limitation 8. Appendix D – XML Samples for Discharge Instructions Sample CDA Header XML Schema http://xreg2.nist.gov:8080/hitspValidation/schema/cdar2c32/infrastructure/cda/C32_CDA.xsd"> <typeId root="2.16.840.1.113883.1.3" extension="POCD_HD000040"/> <templateId root="2.16.840.1.113883.10.20.1"/> <id root="6858a017-39c1-4153-bbd4-eaedac72a0e7"/> <code code="34133-9" displayName="Summarization of episode note" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC"/> <title> Continuity of Care Document from “HIE Name”</title> <effectiveTime value="20081120161000+1400"/> <confidentialityCode code="N" codeSystem="2.16.840.1.113883.5.25"/> <languageCode code="en-US"/> Sample RecordTarget XML Schema <recordTarget typeCode="RCT" contextControlCode="OP"> <patientRole> <id extension="#########"/> <addr use="HP"> <streetAddressLine>15 New Kidney St. </streetAddressLine> <city>Richmond</city> <state>VA</state> <postalCode>22222</postalCode> </addr> <telecom use="HP" value="tel:+1-703-555-1212"/> <telecom use="WP" value="tel:+1-703-555-2323"/> <patient> <name use="L"> <given qualifier="CL">Jane</given> Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 49 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology <given qualifier="CL">M</given> <family qualifier="BR">Snow</family> </name> <administrativeGenderCode code="F" displayName="Female" codeSystem="2.16.840.1.113883.5.1" codeSystemName="HL7 AdministrativeGenderCode"/> <birthTime value="19610821"/> </patient> </patientRole> </recordTarget> Sample Author XML Schema <author> <time value="20080731142500"/> <assignedAuthor> <id root="2.16.840.1.113883.4.6.1013905751"/> <addr> <streetAddressLine>612 Wharf Ave.</streetAddressLine> <city>Fairfax</city> <state>VA</state> <postalCode>20151</postalCode> </addr> <telecom use="HP" value="tel:+1-703-555-0033"/> <assignedPerson> <name> <prefix>Dr.</prefix> <given>John</given> <family>Lee</family> </name> </assignedPerson> <<representedOrganization> <id root="2.16.840.1.113883.X.XXX"/> <name>Hospital Name</name> <</representedOrganization> </assignedAuthor> </author> Sample Informant XML Schema <informant> <assignedEntity> <id extension="KP00017" root="2.16.840.1.113883.19.5"/> <addr> <streetAddressLine>21 North Ave.</streetAddressLine> <city>Burlington</city> <state>MA</state> <postalCode>02368</postalCode> <country>USA</country> </addr> <telecom value="tel:(555)555-1003"/> <assignedPerson> Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 50 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology <name> <given>Henry</given> <family>Seven</family> </name> </assignedPerson> </assignedEntity> </informant> <informant> <relatedEntity classCode='PROV'> <code code='208D00000X' codeSystem="2.16.840.1.113883.11.19465"/> <relatedPerson> <name> <given>Adam</given> <family>Everyman</family> </name> </relatedPerson> </relatedEntity> </informant> Sample Custodian XML Schema <custodian> <assignedCustodian> <representedCustodianOrganization> <id root="2.16.840.1.113883.X.X.XXXX"/> <name>Smith Medical Center</name> </representedCustodianOrganization> </assignedCustodian> </custodian> Sample Participant XML Schema <participant typeCode="IND" contextControlCode="OP"> <templateId root="2.16.840.1.113883.3.88.11.32.3"/> <time/> <associatedEntity classCode="PRS"> <code code="DAU" displayName="Daughter" codeSystem="2.16.840.1.113883.5.111" codeSystemName="HL7 RoleCode"/> <addr use="HP"> <streetAddressLine>612 Wharf Ave.</streetAddressLine> <city>Fairfax</city> <state>VA</state> <postalCode>20151</postalCode> </addr> <telecom use="HP" value="tel:+1-703-555-0033"/> <telecom use="WP" value="tel:+1-703-555-3434"/> <telecom value="mailto:Janet_Snow@email.com"/> <associatedPerson> <name> <given>Janet</given> <family>Snow</family> Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 51 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology <suffix/> </name> </associatedPerson> </associatedEntity> </participant> Sample DocumentationOf XML Schema <documentationOf> <serviceEvent classCode="PCPR"> <effectiveTime> <low value="20000101"/> <high value="20080731"/> </effectiveTime> <performer typeCode="PRF"> <templateId root="2.16.840.1.113883.3.88.11.32.4"/> <functionCode code="PP" displayName="Primary Care Provider" codeSystem="2.16.840.1.113883.12.443" codeSystemName="Provider Role"> <originalText>Primary Care Provider</originalText> </functionCode> <time> <low value="20020101"/> <high nullFlavor="UNK"/> </time> <assignedEntity> <id root="2.16.840.1.113883.4.6.1013905751" extension="Provider ID"/> <code code="280000000X" displayName="Hospitals" codeSystem="2.16.840.1.113883.6.101" codeSystemName="ProviderCodes"/> <addr use="WP"> <streetAddressLine>10 St. Sample Boulevard </streetAddressLine> <city>Example</city> <state>VA</state> <postalCode>11111</postalCode> </addr> <addr use="WP"> <streetAddressLine>123 West Cove Alley</streetAddressLine> <streetAddressLine>Suite #22</streetAddressLine> <city>Richmond</city> <state>VA</state> <postalCode>11111</postalCode> </addr> <telecom use="WP" value="tel:+1-888-555-1111"/> <telecom value="mailto:H.Cohen.MD@SFMC.com"/> <assignedPerson> <name> <prefix>Dr.</prefix> <given>Harry</given> <given>R</given> <family>Cohen</family> </name> </assignedPerson> Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 52 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology <representedOrganization> <id root="2.16.840.1.113883.4.6.2649871"/> <name>St. George Medical Center</name> </representedOrganization> <sdtc:patient> <sdtc:id root="78A150ED-B890-49dc-B716-5EC0027B3983" extension="11224433"/> </sdtc:patient> </assignedEntity> </performer> </serviceEvent> </documentationOf> Sample Advance Directives XML Schema <component> <section> <templateId root="2.16.840.1.113883.10.20.1.1"/> <code code="42348-3" displayName="Advance directives" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC"/> <title>Advance Directives</title> <text> <content ID="Direct-1"> Herein I, Jane Mertle Snow write this document as a directive regarding my medical care. In the following sections, put the initials of your name in the blank spaces by the choices you want. PART 1. My Durable Power of Attorney for Health Care _SMT__ I appoint this person to make decisions about my medical care if there ever comes a time when I cannot make those decisions myself. I want the person I have appointed, my doctors, my family and others to be guided by the decisions I have made in the parts of the form that follow. Name: Sarah Marie Thompson/Daughter Home telephone:301-555-1415 Work telephone: 301-555-1514 Address: 12 East Main New Market, MD 21774 If the person above cannot or will not make decisions for me, I appoint this person: Name: Bradley John Snow/Son Home telephone: 301-555-6677 Work telephone: 301-666-4545 Address: 3453 Hallow Way Baltimore, MD </content> </text> <entry typeCode="DRIV"> <observation classCode="OBS" moodCode="EVN"> <templateId root="2.16.840.1.113883.10.20.1.17 "/> <id root="ec78a751-5994-4910-ada5-ef402937837d"/> <code code="304251008" displayName="Resuscitation" codeSystem="2.16.840.1.113883.6.96" codeSystemName="SNOMED CT"> <originalText> <reference value="#Direct-1"/> </originalText> </code> <statusCode code="completed"/> <effectiveTime> <low value="20050101"/> <high nullFlavor="UNK"/> </effectiveTime> <value xsi:type="CD" code="304253006" displayName="Do Not Resuscitate" codeSystem="2.16.840.1.113883.6.96" codeSystemName="SNOMED CT"/> <participant typeCode="CST"> Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 53 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology <participantRole classCode="AGNT"> <addr use=""> <streetAddressLine/> <city/> <state/> <postalCode/> </addr> <telecom use="HP" value="tel:+1-301-555-1234"/> <playingEntity> <name> <given>Emily</given> <given>X.</given> <family>Green</family> <suffix/> </name> </playingEntity> </participantRole> </participant> <entryRelationship typeCode="REFR"> <observation classCode="OBS" moodCode="EVN"> <templateId root="2.16.840.1.113883.10.20.1.37"/> <code code="33999-4" displayName="Status" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC"/> <statusCode code="completed"/> <value xsi:type="CE" code="425392003" displayName="Current and Verified" codeSystem="2.16.840.1.113883.6.96" codeSystemName="SNOMED CT"/> </observation> </entryRelationship> </observation> </entry> </section> </component> Sample Allergy XML Schema <component> <section> <templateId root="2.16.840.1.113883.10.20.1.2"/> <code code="48765-2" displayName="Allergies, adverse reactions, alerts" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC"/> <title>Allergies and Adverse Reactions</title> <text> <content ID="allergy_comment-1">No known allergies. </content> </text> <entry typeCode="DRIV"> <act classCode="ACT" moodCode="EVN"> <templateId root="2.16.840.1.113883.10.20.1.27"/> <templateId root="2.16.840.1.113883.3.88.11.32.6"/> <id root="36e3e930-7b14-11db-9fe1-0800200c9a66"/> <code nullFlavor="NA"/> <entryRelationship typeCode="SUBJ" inversionInd="true"> Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 54 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology <act classCode="ACT" moodCode="EVN"> <templateId root="2.16.840.1.113883.10.20.1.40"/> <templateId root="2.16.840.1.113883.3.88.11.32.12"/> <code code="48767-8" displayName="Annotation Comment" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC"/> <text> <reference value="#allergy_comment-1"/> </text> <statusCode code="completed"/> <author> <time value="20080101"/> <assignedAuthor> <id root="2.16.840.1.113883.4.6.1013905751"/> <assignedPerson> <name> <prefix>Dr.</prefix> <given>Randall</given> <family>Ford</family> </name> </assignedPerson> </assignedAuthor> </author> </act> </entryRelationship> </act> </entry> </section> </component> Sample Problems XML Schema <component> <section> <templateId root="2.16.840.1.113883.10.20.1.11"></templateId> <code code="11450-4" displayName="Problem list" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC" /> <title>Problem list</title> <text></text> <entry typeCode="DRIV"> <act classCode="ACT" moodCode="EVN"> <templateId root="2.16.840.1.113883.10.20.1.27" /> <id root="ec8a6ff8-ed4b-4f7e-82c3-e98e58b45de7" /> <code nullFlavor="UNK" /> <performer typeCode="PRF"> <time> <low value="20060601" /> <high value="20080924" /> </time> <assignedEntity> <id root="78A150ED-B890-49dc-B716-5EC0027B3982" extension="ProviderID" /> <code code="280000000X" displayName="Hospitals" codeSystem="2.16.840.1.113883.6.101" codeSystemName="ProviderCodes" /> Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 55 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology <addr use="WP"> <streetAddressLine>145 Applecross Road</streetAddressLine> <streetAddressLine></streetAddressLine> <city>Southern Pines</city> <state>NC</state> <postalCode>28388</postalCode> </addr> <assignedPerson> <name> <prefix>Dr. </prefix> <given>Shirley</given> <given /> <family>Jordan</family> </name> </assignedPerson> <representedOrganization> <name>Southern Pines Women's Health Center</name> </representedOrganization> <sdtc:patient xmlns:sdtc="urn:hl7-org:sdtc"> <sdtc:id root="78A150ED-ZZ23-49dc-B716-5EC0027B3983" extension="33445566" /> </sdtc:patient> </assignedEntity> </performer> <entryRelationship typeCode="SUBJ"> <observation classCode="OBS" moodCode="EVN"> <templateId root="2.16.840.1.113883.10.20.1.28" /> <id root="ab1791b0-5c71-11db-b0de-0800200c9a66" /> <code code="282291009" displayName="Diagnosis" codeSystem="2.16.840.1.113883.6.96" codeSystemName="SNOMED CT"></code> <text> <reference value="#prob-1" /> </text> <statusCode code="completed" /> <!--Problem Date--> <effectiveTime> <low value="20080915" /> <high nullFlavor="UNK" /> </effectiveTime> <!--Problem Code--> <value xsi:type="CD" code="174.0" displayName="Malignant neoplasm of female breast" codeSystem="2.16.840.1.113883.6.2" codeSystemName="ICD9" xmlns:xsi="http://www.w3.org/2001/XMLSchema-instance" /> <entryRelationship typeCode="REFR"> <observation classCode="OBS" moodCode="EVN"> <!--20.1.50 = problem status observation 20.1.57 = conformant status observation--> <templateId root="2.16.840.1.113883.10.20.1.50"></templateId> <code code="33999-4" displayName="Status" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC" /> <statusCode code="completed" /> <value xsi:type="CE" code="55561003" displayName="Active" codeSystem="2.16.840.1.113883.6.96" codeSystemName="SNOMED CT" Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 56 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology xmlns:xsi="http://www.w3.org/2001/XMLSchema-instance" /> </observation> </entryRelationship> </observation> </entryRelationship> </act> </entry> <entry typeCode="DRIV"> <!--Condition Module--> <act classCode="ACT" moodCode="EVN"> <!--TemplateId 20.1.27 = CCD Problem Act 11.32.7 = C32 Condition Module--> <templateId root="2.16.840.1.113883.10.20.1.27" /> <id root="ec8a6ff8-ed4b-4f7e-82c3-e98e58b45de7" /> <code nullFlavor="NA" /> <!--Primary Care Physician--> <performer typeCode="PRF"> <time> <low value="20060509"></low> <high value="20080801" /> </time> <assignedEntity> <id root="2.16.840.1.113883.4.6.15597815751" extension="Provider ID" /> <!-- OID is Dr. Orbit's NPI --> <code code="261QM2500X" displayName="Medical Specialty" codeSystem="2.16.840.1.113883.6.101" codeSystemName="ProviderCodes" /> <addr use="WP"> <streetAddressLine>155 Memorial Drive</streetAddressLine> <streetAddressLine></streetAddressLine> <city>Ironton</city> <state>OH</state> <postalCode>11111</postalCode> </addr> <telecom use="WP" value="tel:+1-888-555-5555" /> <assignedPerson> <name> <prefix>Dr</prefix> <given>George</given> <given>E.</given> <family>Orbit</family> </name> </assignedPerson> <representedOrganization> <name>Smith Regional Hospital</name> </representedOrganization> <sdtc:patient xmlns:sdtc="urn:hl7-org:sdtc"> <!--The ID is how the doctor identifies the patient's record. Patient's MRN under the provider producing the CCD/C32--> <sdtc:id root="78A150ED-ZZ12-49dc-B716-5EC0027B3983" extension="11223344" /> </sdtc:patient> </assignedEntity> </performer> Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 57 of 58 Last Updated on 11/15/2011 Office of the National Coordinator for Health Information Technology <entryRelationship typeCode="SUBJ"> <observation classCode="OBS" moodCode="EVN"> <!-- Problem observation template --> <templateId root="2.16.840.1.113883.10.20.1.28" /> <id root="ab1791b0-5c71-11db-b0de-0800200c9a66" /> <!--Problem Type (and description)--> <code code="418799008" displayName="Symptom" codeSystem="2.16.840.1.113883.6.96" codeSystemName="SNOMED CT"></code> <text> <reference value="#prob-1" /> </text> <statusCode code="completed" /> <!--Problem Date--> <effectiveTime> <low value="20080910" /> <high nullFlavor="UNK" /> </effectiveTime> <value xsi:type="CD" code="198.2" displayName="Skin, Skin of breast" codeSystem="2.16.840.1.113883.6.2" codeSystemName="ICD9" xmlns:xsi="http://www.w3.org/2001/XMLSchema-instance" /> <!--Problem Status--> <entryRelationship typeCode="REFR"> <observation classCode="OBS" moodCode="EVN"> <!--20.1.50 = problem status observation 20.1.57 = conformant status observation--> <templateId root="2.16.840.1.113883.10.20.1.50"></templateId> <code code="33999-4" displayName="Status" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC" /> <statusCode code="completed" /> <!--Problem Status--> <value xsi:type="CE" code="55561003" displayName="Active" codeSystem="2.16.840.1.113883.6.96" codeSystemName="SNOMED CT" xmlns:xsi="http://www.w3.org/2001/XMLSchema-instance" /> </observation> </entryRelationship> </observation> </entryRelationship> </act> </entry> </section> </component> Transitions of Care – Discharge Instructions Guide Created on 8/31/2011 Page 58 of 58 Last Updated on 11/15/2011