Journal Club Presentation
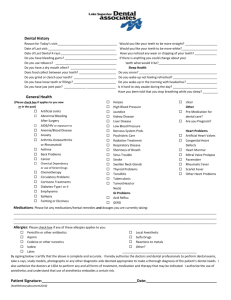
advertisement
+ Management of the Medically Compromised Patient Erica Phillips July 6, 2012 + What we’ll cover today . . . Hemophilia Hepatitis Sickle Cell Anemia HIV/AIDS Leukemia + Goals of Treatment Achieve optimal oral health for patient. Develop a working relationship with patient’s PCP. Minimize complications. Aggressive prevention. + Hemophilia a disorder of hemostasis resulting from a deficiency of a procoagulation factor. X-linked recessive affecting 1/7500 males. Female carriers may have low baseline activity and should be evaluated before dental tx. Hemophilia A: -Factor VIII deficiency (Antihemophilic Factor) -most common type. Hemophilia B (Christmas Disease): -Factor IX deficiency -1/4 as prevalent as Hemophilia A. Hemophilia C: -Factor XI deficiency or Rosenthal’s disease. -autosomal recessive trait. M=F. -Ashkenazi Jews most often affected. Other deficiencies ( II, V, VII and XIII ) are rare and autosomal recessive. + Coagulation Cascade + Hemophilia A & B: Severity Severity Factor % Present Characteristics Mild 5-50% Bleed infrequently and only with surgery or injury. Moderate 1-5% 4-6 bleeding episodes per year, can be spontaneous. Severe <1% -Spontaneous bleeding episodes 2-4x/month in joints, muscles and skin. -hemarthroses can lead to chronic musculoskeletal disease, painful arthritis. -hemorrhagic pseudocysts in jaws accompanied by pain, stiffness, limited ROM. + Hemophilia Treatment: Replacement of Deficient Factor Hemophilia A: For routine hemorrhaging in joints, soft tissues or oral bleeding, a one time correction of 40-50% Factor VIII will stop bleeding. Desmopressin: DDAVP (1-deamino-8-D-arginine vasopressin) is a synthetic analogue of vasopressin used for minor hemorrhagic episodes. Causes increase in Factor VIII and VWF. Caution with DDAVP: long-term use can cause tachyphylaxis. May also be associated with hyponatremia, water retention, and seizures (must monitor electroytes). Hemophilia B: Minimum of 40% correction of purified Factor IX concentrate. + Hemophilia: Administration of Treatment Clotting factor is measured in International Activity Units. Regimen depends on severity of disease, number of bleeding episodes, and physician’s recommendations. Therapy is either “on-demand” (after a bleeding episode) or prophylactic at regularly scheduled intervals. Prophylactic treatment is standard of care for those with severe hemophilia. If pt has catheter placed for venous access, may consider antibiotic therapy (not currently recommended by CDC). + Von Willebrand Disease abnormal VWF (either quantity or quality) in plasma, platelets, megakaryocytes and endothelial cells. important for platelet adhesion to subendothelium via collagen (formation of platelet plug). Symptoms include: Bleeding from skin and mucosa Bruising Epistaxis prolonged bleeding after surgery Menorrhagia Tx: DDAVP. If no response, may try exogenous VWF concentrate. + Von Willebrand Factor + Treatment of Hemophilia: Complicating Factors Inhibitors: antibodies that neutralize the coagulation factor administered. Low-responders have peak levels of inhibitors <5 Bethesda Units. Treat with factor concentrate. High responders have peak titers >5 BU and require bypassing products (prothrombin complex concentrate or recombinant factor VIIa). Arthritis and degenerative joint disease secondary to recurrent bleeding. Blood-borne viral infection (b/c of blood or blood products used in tx), especially HBV and HCV. + Hemophilia: Dental Management Important for Med Hx: type of disorder, severity, frequency and tx of episodes, and inhibitor status. Notice unusual bleeding! As the patient’s dentist, you may be the first to make the diagnosis. Mouth lacerations and persistent oral bleeding are common in children. Dental providers should schedule evaluations and interventions on planned infusion days. Those treated with on-demand regimens require planning for replacement therapy in preparation for specific procedures. Effort should be made to do as much as possible in one appointment to avoid multiple costly infusions. Discussion with hematologist: type of anesthetic to be used, invasiveness of procedure, amount of bleeding anticipated, time involved in oral wound healing. Pharmacological Management + Adjunctive Pharmacological Management for Dental Services Antifibrinolytic agents: prevent clot lysis in oral cavity. Aminocaproic acid (Amicar) and Tranexamic Acid (Cyklokapron). Taken orally immediately before dental treatment and then every 6-8 hours for approximately one week. Side effects of antifibrinolytics: headache, nausea, dry mouth. May increase risk of thrombosis in those with renal or urinary tract bleeding, evidence of DIC or prolonged use of replacement therapy in high responders. + Pain Control for Hemophiliacs: Sedation, nitrous oxide and hypnotics for anxiety. Avoid aspirin or Ibuprofen. Use acetaminophen (Tylenol) for acute pain. Narcotics may be required for severe pain. IM injections are contraindicated b/c of risk of hematoma. PDL injections okay if factor replacement being given. If no replacement therapy or anti-fibrinolytic agents, can still infiltrate. For highly vascular areas, replacement levels should be at least 30-40%. Blocks: caution required. The IAN and PSAN are surrounded by loose, connective, highly vascularized tissue. Can get dissecting hematoma, may cause airway obstruction and a lifethreatening bleed. Requirement is minimum of 40% factor correction with blocks. Must aspirate! If blood in aspirate, may need to give further give factor replacement and must notify hematologist immediately after procedure. + Hemophilia & Dental Procedures Prevention: OHI, brushing, flossing, topical fluoride, systemic fluoride, dietary counseling, professional exams. Rubber cup prophy and supragingival scaling can be done without replacement therapy. Control minor bleeds with moistened gauze pressure, topical bovine thrombin, microfibrillar collagen, local fibrin glue. Periodontal Tx: Initial supragingival scaling followed by 1-2 week healing period so that gingival edema/hyperemia will decrease. Then can remove calculus and irritants with less bleeding. Subgingival scaling: consider replacement therapy, depending on amount of bleeding expected and severity of deficiency. + Hemophilia & Dental Procedures Restorative: Thin rubber dam essential for isolation and to protect soft tissues from laceration. Avoid lacerating the gingiva with the clamp or frame. Can use wedges and matrix bands as normal (wedge protects the papilla). Caution with high speed suction and intraoral radiographs to avoid sublingual bleeds. Pulpal therapy: Indirect pulp cap to avoid exposure. If exposure occurs, can use cotton pellet to control bleeding. Pulpotomy or pulpectomy is preferable to extraction. + Hemophilia & Extractions: Simple exo of erupted permanent teeth and multirooted primary teeth: 30-40% factor correction within 1 hour of dental tx. Antifibrinolytic tx immediately before or after procedure and continues for 5-10 days. Clear liquid diet for first 72 hours, then soft pureed diet for a week. . At day 10 can start normal diet. No straws, metal utensils, pacifiers or bottles. Surgical exo of impacted, partially erupted or unerupted teeth: higher factor activity level targeted. May want factor replacement post op. antifibrinolytic therapy started immediately before or after procedure, continue for 7-10 days. + Hemophilia & Extractions: Simple exo of single rooted primary teeth: evaluate root development to decide if replacement therapy required. If only partially formed root, antifibrinolytic plus local hemostatic agents may be enough. Bleeding from exfoliation of primary teeth: direct finger and gauze pressure for several minutes. Topical agents. Antifibrinolytics if bleeding slow and continuously. Rarely need RT, usually when gingival tissue is repeatedly traumatized during exfoliation. + Hemophilia & Extractions: Local hemostasis after exo: topical hemostatic agents: thrombin, microfibrillar collagen, or fibrin glue on wound. Direct pressure with gauze. Stomadhesive dressing protects from oral environment. Avoid sutures, unless they will really enhance healing and in this case, use resorbable kind. + Hemophilia & Extractions: Surgical complications: bleeds may occur 3-4 days post op when clot breaks down. Typical clot is dark red, protrudes from surgical site, covering several teeth. Abnormal clot should be removed after RT given, area cleaned to isolate source of bleed, repack and use AF agents. + Hemophilia and Orthodontics: early intervention can help prevent need for more complex tx later on. Interceptive or full-banded ortho can be done. Avoid sharp edges and wires when placing and adapting bands. Preformed bands and brackets can bond directly to teeth and avoid contact with gingiva. Use longer-acting wires and springs b/c needs less adjusting. oral hygiene very important to avoid inflammation of gingiva. Water irrigating device helpful for homecare. + Infection that produces inflammation of liver cells. Most cases resolve after acute infection, esp A and E. Prodromal (early phase): lethargy, loss of appetite, nausea, vomiting, abdominal pain, jaundice, hepatomegaly or splenomegaly. Jaundice is clinically apparent when bilirubin levels in plasma are >2.5mg/100 mL). Convalescent phase: symptoms disappear, hepatomegaly and abnormal liver function may persist for up to four months. > 4 million Americans are chronic virus carriers (low levels of the virus > 6 months). Can become chronic active virus after decades, leading to hepatocellular necrosis. In those with chronic active hepatitis, 20% get cirrhosis, and 1-5% develop a primary hepatocellular carcinoma. + Functions of the Liver Bile secretion (fat absorption) Converts sugar to glycogen Excretes bilirubin (waste product of hemoglobin). Synthesis of coagulation factors Drug metabolism When impaired: look out for bleeding issues and impaired drug metabolism! + HAV Between 125,000 and 200,000 new cases of Hep A occur annually in U.S. (47% of acute hepatitis cases reported). Picornavirus – RNA virus that replicates in liver, excreted in bile and shed in stool. Spread by fecal-oral route. Common sources are contaminated water, restaurants, raw shellfish, daycare centers. May present as acute fever with jaundice, anorexia, nausea, malaise, lymphadenopathy, night sweats. 10% are asymptomatic. Infants and children will present with mild non-specific symptoms without jaundice. no carrier state. IgG or IgM anti-HAV indicates past infection and lifelong immunity to HAV. Vaccine (inactivated virus) available since 1996 in the U.S. Can also give HAV Ig within 2 weeks of exposure. + HBV 140,000-320,000 reported annually in U.S. (27% of acute Hep infections). Hepadnavirus -replicates in hepatocytes and stem cells. Transmitted by parenteral, percutaneous or mucous membrane inoculation. Vertical transmission from mom to baby possible. Most infections occur in young adults. 10% occur in infants and young children. 70-90% are asymptomatic in acute phase. Chronic HBV develops in over 25% carriers. Can progress to cirhossis or liver cancer. Lab tests: Antibody to Heb B surface antigen: indicates resolution of natural infection or successful vaccination (long term immunity). Antibody to core antigen (IgG or IgM anti-HBc): indicates recent infection. Anbitbody to Hep Be antigen (“early” antigen from cleavage of core antigen) indicates infectivity. Recombinant DNA vaccine recommended for healthcare workers. Universal vaccination of infants. Post exposure immunoprophylaxis of infants born to HBsAg-positive women. Hep D Fulminant hepatitis when infection coexists with Hep B. (Requires Hep B outer coat proteins) to superinfect. + HCV The most common bloodborne infection in the U.S. 3.5-4 million Americans have chronic infection. Flavivirus – parenterally transmitted. Vertical transmission from mother to child possible: accounts for 5% of HCV cases. 60-70% asymptomatic in acute phase. 70-85% develop chronic hepatitis. No immunization available. leading cause of liver transplants in U.S. Dx: anti-HCV in serum. + Hepatitis Tx Acute phase: bed rest, fluids, nutritious high calorie diet. No alcohol or drugs that are metabolized by liver. Monitor viral antigens and ALT levels for 6 months to test whether infection has resolved. Chronic hepatitis: Interferon (IFN) alpha-2b, 3x/week for 6 months -1 year. Can normalize ALT levels and lower risk of hepatocellular carcinoma Only 10-30% achieve long term remission. Lamivudine (nucleoside analog active against HBV) or ribavirin (against HCV). Corticosteroids for fulminant infection. Liver transplant for cirrhosis. + Oral Manifestations of Hepatitis Abnormal bleeding: abnormal clotting factor synthesis, inadequate fibrin stabilization, excessive fibrinolysis, thrombocytopenia. Rarely, hepatocellular carcinoma will metastasize to jaw. Will present as hemorrhagic expanding masses in premolar and ramus areas of mandible. + Dental Management of Hepatitis: For pts with active hepatitis: Urgent (absolutely necessary) dental work only. Minimize aerosols and avoid drugs that are metabolized in liver. For surgery: preop prothrombin time and bleeding time should be obtained. Obtain platelet count, confirm that INR is under 3.5. For pts who are carriers: Standard universal precautions Consult with physicians: liver function lab tests to assess hemostasis issues and metabolic problems. No elective tx if signs or symptoms of hepatitis. Refer to physician. If recovered, no tx modifications necessary + Drugs metabolized primarily by liver: Local Anesthetics: Lidocaine (xylocaine), mepivicaine (carbocaine), prilocaine (citanest), Bupivicaine (marcaine). Analgesics: Aspririn, Acetominophen, Codeine, Ibuprofen, Meperidine. Sedatives: Diazepam, Barbiturates. Antibiotics: Ampicillin, Tetracycline, Metronidazole, Vancomycin. May be used unless hepatic disease is severe, but in limited amounts Diminished dosages should be considered when: aminotransferases > 4x normal Serum bilirubin > 35 μM/L or 2 mg/dL. Serum albumin levels < 35 mg/L Signs of ascities and encephalophathy, prolonged bleeding time. + Sickle Cell Anemia Autosomal recessive More common in those of African descent and also Italians, Middle Eastern, Greek and Indians. The mutation confers advantage against infection with P. falciparum (malaria). 1/600 African Americans have sickle cell anemia. Valine for glutamic acid substitution in beta chain of Hemoglobin forms Hemoglobin S instead of Hb A decreased oxygen capacity, cell rigidity and membrane damage and sickling of cells under lower oxygen tension. Results in erythrostasis, increased blood viscosity, reduced blood flow, hypoxia, vascular occlusion. Clinical signs include jaundice, pallor, dactylitis, leg ulcers, organomegaly, cardiac failure, ocular damage, stroke, bone pain, abdominal pain, delays in growth and development. + Sickle Cell Crisis: Precipitated by acidosis, hypoxia, hypothermia, hypotension, stress, hypovolemia, dehydration,trauma, fever and infection. decreased RBC production severe joint and abdominal pain, fever, ischemia and infarction of organs. Deterioration of cardiac, pulmonary and renal fxn. + Oral Manifestations of SCA: Radiographic changes: generalized radiolucencies. loss of trabeculation, more prominent lamellar striations. “stepladder” appearance of bone b/t teeth. prominent lamina dura Hyperplasia of marrow spaces because of increased erythropoetic demands. Generalized osteoporosis of mandible – thinning of inferior border. Frontal bossing and “hair on end” appearance of cortical regions of skull radiographs. Retrusion of mandible due to decreased bone growth. Hypomineralized teeth or delayed eruption of teeth. Infarcts in jaw due to vaso-occlusion: osteomyelitis, pulpal necrosis, ischemic necrosis in mandible, and peripheral neuropathy( Dental pain with no pathology). Pale oral mucosa Jaundice (from excessive erythrocyte destruction leading to hyperbilirubinemia). + “Hair on End” Enlarged marrow spaces + Medical Management of SCA: Daily folic acid supplements to prevent crisis. Penicillin prophylaxis for first 5 years of life. Hydroxyurea +/- erythropoietin to induce formation of HbF (and prevent HbS). When crisis occurs: High doses of folic acid Analgesics Hydration Blood transfusions. Bone Marrow Transplantation: moderate success in treating SCA (25%) but increased mortality. + Dental Management of SCA: Can receive routine dental care during non-crisis periods. During a sickle cell crisis, emergency tx only. Short appointments to lower stress. Avoid long/complicated procedures. Aggressive prevention to lower chance of infection, especially when patient has spleen defects. Currently a debate over need for prophylactic abx. Avoid tissue irritation leading to bacteremias. For major surgical procedures: prophylactic penicillin to prevent wound infection or osteomyelitis. Restoration of teeth is preferable to exo. Pulpectomy okay as long as tooth is noninfected. If infected and persistent, extract. OHI essential. Orthodontics may be helpful for skeletal changes. Careful monitoring required. Use of epinephrine is controversial (some believe it may impair blood flow and cause vascular occlusion). Use of nitrous oxide okay. Avoid diffusion hypoxia at end of procedure. At least 50% oxygen should be provided. Avoid dehydration – fluid intake important, esp during IV sedation. Pain control: acetaminophen and small doses of codeine are acceptable. Avoid aspirin (salicylates) in high doses b/c acid effect may cause crisis. IV sedation: caution required. Avoid barbiturates and narcotics (supress respiratory center). Can use Diazepam. GA : if Hb < 7g/dL and hematocrit <20%, transfusion may be required. Peds pts are less likely to have post-transfusion complications. + HIV/AIDS Worldwide as of 2007, 2.5 million children were infected with HIV. lymphocytes and macrophages contain greatest # of CD4 surface glycoproteins that attach to viral surface proteins (GP120) and enhance host cell invasion and infection. has a viral enzyme reverse transcriptase that incorporates viral RNA into the host nuclear DNA, leads to death of CD4 cells. results in opportunistic infections, malignancies (Kaposi sarcoma and lymphoma) and autoimmune diseases. + HIV medical management: Depends on CD4 count (indicates immune status) and viral load (indicates acceleration of disease). approximately 30% of newborns of untreated HIV-infected mothers can acquire the HIV virus thru vertical transmission. Medicating the mother with antiretrovirals such as AZT can decrease rate of transmission by 70%. + Children with HIV: Only 75% of untreated babies survive to age 5, with 50% of them having severe symptoms. Clinical findings in infants and children with AIDS are similar to those of adults. Early manifestations: interstitial pneumonitis weight loss failure to thrive hepatomegaly and/or splenomegaly generalized lymphadenopathy chronic diarrhea. Also common in children are recurrent and severe bacterial infections. + Oral Manifestations of HIV: Fungal Infections Candida albicans is most common HIV-associated infection in the mouth. May lead to esophageal or disseminated candidiasis. Four oral types of C. albicans are pseudomembranous, hyperplastic, erythematousand angular cheilotic. Pseudomembranous type: removable creamy white or yellow plaques on palate, buccal mucosa, or dorsum of tongue. Red bleeding surface underneath. Hyperplastic type: white plaques on buccal mucosa, not easily removed. Erythematous (atrophic) type: red spotty areas on palate, dorsum of tongue and buccal mucosa. Angular cheilitis: fissures radiating from commissures of mouth, associated with small white plaques. Treat all types with topical antifungals (clotrimazole or nystatin) and systemic antifungals (ketoconazole, fluconazole, amphotericin B), and Peridex. + Oral Manifestations of HIV: Viral and Bacterial Infections HPV: oral warts with raised cauliflower-like appearance or flat circumscribed look. HSV: painful ulcerations, most commonly on palate or tongue. VZV. Oral ulcerations, usually with skin lesions on one side of face. EBV: Oral hairy leukoplakia shows as white, smooth, corrugated or folded lesion that does not rub off, often on lateral tongue. Mycobacterium avium-intracellulare and klebsiella pneumonia. Follow atypical course or unusual response to treatment in HIV pts. + Oral Manifestations of HIV: Neoplasms Kaposi sarcoma: most common malignancy in AIDS. Intraoral lesions can occur alone or along with skin, visceral and LN lesions. Red, blue or purple, flat or raised, one or multiple. Most common oral site is hard palate. Lymphomas, esp NHL. Firm painless swelling in mouth may be first manifestation. Mean survival from time of dx is 6 months. OSSC also more common in HIV population. + Oral Manifestations of HIV: Idiopathic Lesions oral ulcers of unknown etiology are increasing in frequency. Appearance is apthous, well-circumscribed with erythematous margins. Sometimes they are large, painful and necrotic. Salivary gland swelling, usually of parotids, with xerostomia. + Oral Manifestations of HIV: Gingivitis and Periodontitis May be first sign of HIV infection. No response to standard periodontal therapy. Rapid progression to advanced disease. Spontaneous bleeding. Treatment is aggressive curettage, Peridex 3x/day and abx. + Leukemia proliferation of abnormal leukocytes (blasts) in bone marrow and dissemination of these cells in peripheral blood and other organs. Leukemia is classified according to morphology of predominant abnormal WBC in the bone marrow. Can be acute or chronic. ALL, AML, CML, CLL (not seen in children) 6550 new cases of cancer dx each year in kids < 15 in U.S. Acute leukemia is most common malignancy in children. + Leukemia: Clinical Manifestations Hematopoietic abnormalities: anemia, thrombocytopenia, granulocytopenia. irritability, lethargy persistent fever vague bone pain, easy brusing. Pallor, petechhiae, cutaneous bruises tachycardia adenopathy, hepatosplenomegaly, gingival bleeding infections. + Acute Leukemia 1/3 of all childhood malignancies. 80% are lymphocytic (ALL). Chronic leukemia in kids is rare (<2% all cases). Peak incidence of ALL is b/t age 3-6. Cause unknown. Radiation, chemical agents, genetics implicated. Genetic risks: -chromosomal abnormalities (Down Syndrome, Bloom syndrome) -pt with an identical twin with leukemia -some immunologic disorders. + Treatment of Acute Leukemia: Goal of tx is remission: <5% blasts. Minimal Residual Disease: <.1% blasts. Better prognosis. ANLL: < 1 yr of intense tx, with profound bone marrow hypoplasia. ALL: less intense tx, duration of tx is 2.5-3.5 yrs. + Treatment of Leukemia: Phases Induction phase: combo of anti-leukemic drugs at staggered intervals for 4 weeks. Maintains regenerative potential of non-malignant hematopoietic cells within the bone marrow. 95% of ALL pts in remission after 4 weeks. Consolidation phase: consolidates remission and intensifies prophylactic CNS tx. Intrathecal dose of chemo in lumbar spine has replaced cranial irradiation except for high risk ALL pts. Interim maintenance: monthly appointment, outpt. Relatively non-toxic agents. Delayed intensification: to intensive therapy after a short period of less intense therapy. Improves survival for ALL. Maintenance therapy: 2 yrs for girls, 3 yrs for boys. + ALL prognosis: Overall survival of ALL in kids is 80%: due to improved drugs, combo therapy, radiation, diagnostic techniques, general supportive care. Those with best response to therapy are between ages 1-10 with a WBC <50,000/cc. If < 1 yr old or > 10 yrs, EFS is much lower after five years and more intensive treatments needed. Early response to induction of chemo is strong predictor of outcome for ALL. + Acute Myelogenous Leukemia (AML) Types: Acute myelocytic leukemia (older children and adolescents), Acute myelomonocytic leukemia (infants and young children), Acute promyelocytic leukemia (uncommon, older children), erythroleukemia (rare), megakaryocytic leukemia (rare) Prognosis for AML: 50% survival at 3 yrs from dx for those children undergoing chemotherapy. Higher survival rates in those who have received an allogeneic stem cell transplant addition to chemo. Tx for AML is more intrusive: causes profound bone marrow suppression, prolonged severe neutropenia, long hospitalizations and severe mucositis. + Leukemia: Oral Manifestations 29% of children with leukemia have oral manifestations. -more common in acute rather than chronic leukemia, and more common in AML than ALL. attributed to anemia, granulocytopenia, and thrombocytopenia. Regional lymphadenopathy most common finding. Leukostasis can cause tissue anoxia, necrosis and ulcerations that can become infected by opportunistic microorganisms in pts with neutropenia. Severe thrombocytopenia leading to spontaneous bleeds petechiae or ecchymoses of oral mucosa or bleeding from gingival sulcus. Poor oral hygiene can exacerbate local irritation and gingival bleeding. Leukemic cells infiltrate tissue, cause gingival hypertrophy (esp in AML). Teeth may loosen if PDL undergoes necrosis. Occasional CN palsies, chin and lip paresthesias, odontalgia, jaw pain, loose or extruded teeth, gangrenous stomatitis. + Ecchymoses Petichia + Leukemia: Oral Radiographs Skeletal lesions: generalized osteoporosis (enlarged Haversian canals and Volkmann canals). Osteolytic lesions: from focal hemorrhages and necrosis causing loss of trabecular bone. destruction of crypts of developing teeth loss of lamina dura, widened PDL, displaced teeth and tooth buds. + Displacement of Molar in child with AML + Dental Management of Leukemia: Goals of Initial Exam: to prevent or stabilize any oral pathology that may cause further infection. The most most frequently documented source of sepsis in immunocompromised cancer patients is the mouth. educate the parents and patient about the importance of oral care for preventing or minimizing complications during oncological treatment Inform parents of possible sequelae in the mouth from oncological treatment. Information to obtain from physician: primary dx, anticipated clinical course and prognosis, present and future therapeutic modalities, present general state of health, present hematological status. + Blood Cell #s: Platelet levels: Norm is b/t 150,000-400,000. If >75K, can proceed normally but have hemostatic tactics available in case needed (thrombin, gelfoam, etc) If b/t 40-75K, can do routine preventive and restorative, including infiltrations. Bleeding time will be prolonged. May consider pre and post-op platelet transfusion. Hemorrhage from gingival sulcus (with activities like toothbrushing): will occur when platelets are < 40K and pt has poor OH, unhealthy periodontium or local irritation. Defer elective care, and coordinate with patient’s physician in case of dental emergency regarding hemostasis strategies.. If < 20K, spontaneous hemorrhage of introral tissues may occur. No dental tx should be done without prophylactic platelet transfusion. Absolute neutrophil count (ANC) indicates ability to suppress/eliminate infection. >1000/cc: no antibiotic prophylaxis needed. If b/t 500-1000, defer elective procedures that could cause significant bacteremia. Abx prophylaxis needed for emergency procedures. If <200, pt is at significant risk for sepsis. + Leukemia: Dental Treatment Planning Ideally all pts should have an oral exam and treatment of oral disease prior to oncologic therapy to prevent complications once the patient is immunocompromised. Discuss dental tx and schedule with physician. Defer all elective procedures if child is not yet in first remission or is in relapse. If pt is in remission but still undergoing chemo: can do routine prevention restorations and surgery. Timing depends on specific agents and time of administration. Same day as dental procedure: get CBC and platelet count (r/o risk of hemorrhage or infection). If in remission for >2 yrs and not taking chemo, can treat normally without pre-appointment blood work up. + Prevention is Key! Prevention and treatment of oral inflammation, hemorrhage and infection are essential. Corticosteroids or neutropenia may mask the signs of periodontal inflammation or infection Comprehensive oral hygiene and compliance are key. soft nylon or electric brush for teeth and tongue 2-3x/day, even with thrombocytopenia, as long as it doesn’t cause significant hemorrhage. If mucositis makes fluoride or brushing painful, can use foam or super soft brush instead. flossing need is assessed on individual basis – okay if patient has been trained. Toothpicks and irrigants may cause tissue irritation. scaling and subgingival curetattage to remove significant local irritants. Remove orthodontic appliances. Lowers risk of hemorrhage and infection. warm saline rinses can help diminish leukemia-related gingivitis. Daily chlorhexidine for those with periodontal disease or poor oral hygiene, unless mucositis develops (will irritate mucosa b/c of high alcohol content). Dietary counseling. Fluoride treatments. + Pulpal Therapy and Leukemia: Pulp therapy on primary teeth: No studies have been done on the risks of pulp therapy, but many dentists prefer exodontia over pulp therapy b/c less risk of infection. Endodontics on permanent teeth: A non-vital symptomatic tooth should be treated endodontically at least 1 week before oncological treatment to assess success of procedure. If not enough time, exo. Exo if RCT can’t be done in single visit, with antibiotics after for 1 week. If tooth is asymptomatic, can delay endo until pt’s cell counts are more stable. not recommended for pts who have chronic suppression of granulocytes (they are susceptible to low-grade chronic inflammation). If in prolonged complete remission and no longer having chemotherapy, dentist may decide whether or not to do endodontic therapy on permanent tooth. + Surgery No definitive guidelines for abx prophylaxis for exo. Exo should be as atraumatic as possible. No sharp bony edges, adequate wound closure. Antibiotics if extracted tooth was infected. Must complete OS prior to administration of bisphosphonates to prevent BONJ and ORNJ. Loose primary teeth should be allowed to exfoliate naturally, but if pt won’t leave it alone, should be extracted to prevent bacteremia. Extract: non-restorable teeth, root tips, teeth with perio pockets > 6mm, symptomatic impacted teeth, acute infections, teeth with bone loss, furcation involvement, mobility. Debate over need to extract partially erupted 3rd molars – only those with periodontal involvement or pulpal involvement. Ideally exo 2 weeks before cancer therapy begins. + Leukemia and Orthodontics Poorly fitting appliances can abrade mucosa and increase risk of infection Appliances should be removed if pt has poor OH or if onco treatment will leave pt at risk for mucositis. Simple fixed appliances like a band and loop or lower lingual arch may be left in place if pt has good hygiene. Use orthodontic wax to minimize trauma. Removable appliances: pt must change soaking solution daily, must keep clean! + Sequelae of Treatment Trismus Radiation may cause fibrosis of masticatory muscles. Daily stretching exercises/physical therapy indicated. Should start BEFORE radiation therapy begins. Treatments for trismus include prosthetic devices, trigger point injections, muscle relaxants and analgesics. Ulcers associated with certain chemo agents: methotrexate, anthracycline, daunomycin and doxorubicin. Traumatic ulcers can come with granulocytopenia, especially seen on lateral tongue and buccal mucosa. Pain control: topical pain relievers. Bleeding control: topical thrombin or Avitene. Ulcers can be nidus for colonization by microorganisms – must monitor these lesions to prevent infections. + Leukemia and Candidiasis Common in leukemia patients due to: physical debilitation immunosuppression, prolonged abx use chemo poor oral hygiene. Tx: Nystatin, fluconazole. + Mucositis Occurs in 40-75% of children undergoing chemo/radiation. mild mucositis = mild erythema, no mucosal ulcerations, no pain. Can swallow. No local analgesia required. moderate mucositis: moderate erythema, multiple ulcerations with pain, may require analgesics. Swallowing may be painful. severe mucositis: erythema, multiple ulcerations, severe pain requiring analgesia, difficulty or inability to swallow. Pt care focuses on palliation and prevention of secondary symptoms such as infection. Nystatin rinse for C. albicans infection. No Chlorhexidine (painful). Soft toothbrush. Topical analgesics for pain management: hydrocortisone, Benadryl, viscous lidocaine, Palifermin, Amifostine. + Long term effects of chemo/radiation: rampant caries poor development of teeth: root agenesis, microdontia, root thinning shortening, enamel dysplasia. Xerostomia Post RT bone loss and periodontal disease Osteonecrosis from bisphosphates Post RT TMJ dysfunction/trismus. Altered bone growth and facial development Malocclusion + Radiation Protection: For those undergoing H&N radiation, Lead-lined stents and shields Protection of salivary glands Surgically moving gland away from site of radiation Cytoprotectants 3-D intensity modulated RT + After cancer tx ends: Goal is to maintain optimal oral health and impress upon pt and parents the importance of care See pt at least every 6 months. OH, diet and fluoride counseling. Lip care with lanolin based products. If chronic GVHD, xerostomia, trismus present, see more often. Pts with moderate/severe mucositis or chronic GVHD should be monitored for malignant transformation to SCCa. Ortho tx may start after 2 year disease-free survivial (no more immunosupression). Keep in mind that there may have been developmental/morphological changes to jaws and teeth that need assessment. Consult with physician regarding pt’s use of bisphosphonates and their effect on tooth movement. Avoid elective surgical procedures in pts who have had bisphosphonates. Xerostomia: fluoride treatments recommended; sugar-free gum, humidifier in room at night, oral moisturizers. salivary stimulating drugs not approved for children. + Stem Cell Transplantation: Rescue therapy for pts undergoing aggressive tx for leukemia with chemotherapy and radiation. Pt will receive all of chemo/radiation in few days prior to transplant. Prolonged immunosupression following transplant. must have compatible donor (ideal is identical twin, sibling) tx failure: host rejection of transplanted organ and infection. Graft Versus Host Disease. + Oral Complications of BMT During conditioning phase (pre-op prep and 30 days after): Ulcers, gingival bleeding, mucositis, transient salivary gland dysfnction, oral pain, taste dysfunction, xerostomia. Opportunistic infection. To control bleeding: platelet transfusions, systemic Amicar, topical Avitene, powdered thrombin, pressure. pain control: topicals, LA, systemic analgesics. culture specimens from all lesions to check for infection and abx susceptibility. Engraftment and Hematopoietic Reconstitution: with return of BM fxn and rise of ANC, oral ulceration and mucositis can resolve. Usually begins 3-4 weeks post transplant. Oral fungal and herpetic infections most noticeable. Same oral care as post-cancer tx. Look out for GVHD, xerostomia and sensitivity to thermal stimuli. Immune Reconstitution/Late Post-transplantation: Effects due to chronic toxicity of the conditioning regimen: salivary gland dysfunction, craniofacial growth abnormalities (Esp if under age 6), viral infections, chronic GVHD and squamous cell carcinoma. + Graft v. Host Disease Immunocompetent donor cell and recipient cell interaction of antigens when pt has undergone a BMT. acute form: lymphoid system, skin, liver and GI tract involved. Can be severe and fatal. Chronic form: cutaneous and oral mucosal involvement. More transient and controlled. painful mucosal erythema, reticular or lichenoid eruptions, desquamation,ulceratiosn. salivary gland dysfunction: xerostomia, dysphagia, dysgeusia tx: High and low dose steroids (prednisone, dexamethasone), antithymocyte globulin, cyclosporine, azathioprine, methotrexate. Dexamethasone rinses for salivary gland dysfunction to prevent infections. GVHD also has a beneficial graft-versus-leukemia effect. Inverse relationship b/t GVHD and incidence of relapse. + Preparing patient for BMT: Pretransplant preparation: goal: prevent or relieve oral problems in pts receiving chemo or radiation therapy. All dental tx needs to be done prior to transplant b/c recovery from immunosupression can take up to a year or longer! Elective dentistry must be postponed until recovery has occurred. keep oral cavity clean, moist, free of infection. 4 weeks before transplant: clinical and radiographic oral exam. Inform pt of potential oral complications of transplant. OHI (brushing and flossing). Self-applied topical fluoride gel, Peridex rinse every 12 hours. S/RP, operative and oral surgery are done beforehand to eliminate and control infections. Treat pulpally or periodontally involved teeth, partially erupted or exfoliating primary teeth before admission. Ideally dental treatment is completed at last 2 weeks before admission. at minimum, make sure mouth is free of foci of acute infection and physical irritants. + On admission to hospital: Peridex: minimizes septic episodes in oral cavity when used with other chemotherapeutic agents. Can brush with toothbrush soaked in Peridex. do not eat or drink for 1 hour after Peridex. Apply surgilube to lips for dryness after rinsing. if platelet count is under 20K/cc, with gum bleeding, use Toothette instead of brush. Antifungal prophylaxis : fluconazole. Fungal activity should be monitored by hospital staff during each shift. + Solid Tumors approx half of cases of childhood malignancies. brain tumors Lymphoma Neuroblastoma Wilms tumor Osteosarcoma Rhabdomyosarcoma Most notable complications of these tumors are bleeding tendency and propensity to infection. Management is similar to that of patients with acute leukemia + Thank you! + Sources Consulted: McDonald and Avery’s Dentistry for the Child and Adolescent. 9th edition. Little, James et al. Dental Management of the Medically Compromised Patient. 7th ed. AAPD Guideline on Dental Management of the Pediatric Patient Receiving Chemotherapy, Hematopoietic Cell Transplantation and/or Radiation. Revised 2008.