Auscultation
advertisement

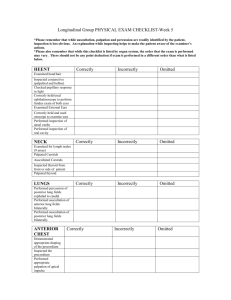
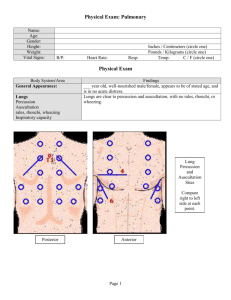
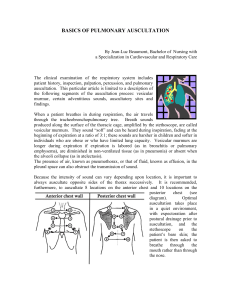
Auscultation Auscultation • By the time you listen, you should know what to hear • If you don’t hear what you expect, explain it • Don’t leave the bedside till you know what you are hearing • Never auscultate from the wrong side of the bed Auscultation • Use the diaphragm for high pitched sounds and murmurs • Use the bell for low pitched sounds and murmurs • Sequence of auscultation – – – – – – upper right sternal border (URSB) upper left sternal border (ULSB) lower left sternal border (LLSB) apex apex - left lateral decubitus position lower left sternal border (LLSB)- sitting, leaning forward, held expiration Auscultation Grading of Murmurs: Grade 1 - only a staff man can hear Grade 2 - audible to a resident Grade 3 - audible to a medical student Grade 4 - associated with a thrill or palpable heart sound Grade 5 - audible with the stethoscope partially off the chest Grade 6 - audible at the bed-side Characteristics of a “functional” murmur • • • • Short and soft SEM Normal S1 and S2 Normal cardiac impulse No evidence for any hemodynamic abnormality Auscultation • Use the diaphragm for high pitched sounds and murmurs • Use the bell for low pitched sounds and murmurs • Sequence of auscultation – – – – – – upper right sternal border (URSB) upper left sternal border (ULSB) lower left sternal border (LLSB) apex apex - left lateral decubitus position lower left sternal border (LLSB)- sitting, leaning forward, held expiration Auscultation Grading of Murmurs: Grade 1 - only a staff man can hear Grade 2 - audible to a resident Grade 3 - audible to a medical student Grade 4 - associated with a thrill or palpable heart sound Grade 5 - audible with the stethoscope partially off the chest Grade 6 - audible at the bed-side Assessing Murmurs Grading of Murmurs: Grade 1 - only a staff man can hear Grade 2 - audible to a resident Grade 3 - audible to a medical student Grade 4 - associated with a thrill or palpable heart sound Grade 5 - audible with the stethoscope partially off the chest Grade 6 - audible at the bedside Functional Murmur: • short and soft SEM • Normal S1 and S2 • Normal cardiac impulse • No evidence for hemodynamic abnormality Innocent Murmurs • Common in asymptomatic adults • Characterized by – Grade I – II @ LSB – Systolic ejection pattern S1 S2 – Normal intensity & splitting of second sound (S2) – No other abnormal sounds or murmurs – No evidence of LVH, and no with Valsalva Common Murmurs and Timing (click on murmur to play) Systolic Murmurs • Aortic stenosis • Mitral insufficiency • Mitral valve prolapse • Tricuspid insufficiency Diastolic Murmurs • Aortic insufficiency • Mitral stenosis S1 S2 S1 Auscultation “Aortic area” • 2nd left intercostal space (URSB) – compare S1 to S2-S1 should be softer. If the same, think Mitral Stenosis – identify ejection murmur-time the peak intensity in relation to systole – identify ejection click if present Auscultation “Pulmonary Area” • 2nd right intercostal space (ULSB) – listen for split S2 (A2/P2) – identify the intensities of A2 and P2 – time split S2 with respiration – – – – normally widens with inspiration, closes with expiration wide split S2-RBBB, RV volume overload,PS, RV failure wide fixed split = ASD paradoxical split = LBBB, severe AS, severe LV dysfunction, pacemaker Auscultation Differential diagnosis of split S2 • A2/P2 • A2/Pericardial knock • A2/OS Sometimes 3 components heard • A2/P2/OS • A2/P2/PK Exclude S3 • Lower pitched • Heard with bell • At apex • In left decubitus position Auscultation Left Sternal Border • Listen for early diastolic murmurs (AR/PR) • Press firmly with diaphragm • Listen upright with forced expiration • Listen on hands and knees Auscultation “Mitral Area” (LLSB) • Listen for intensity of S1 – Soft-LV dysfunction, first degree heart block, preclosure with sudden severe AR/MR – Loud-MS, sympathetic stimulation – Variable- Complete heart block with AV dissociation, Wenkebach • Identify splitting of S1 – M1/T1, M1/EC(aortic or pulmonary) , M1/Non-EC (MVP), S4/M1 Auscultation “Mitral Area” (LLSB) • Identify quality,timing and intensity of systolic murmurs – ejection quality vs regurgitant quality – pansystolic vs early or mid to late systolic murmer Auscultation Apex – Listen for S3 and S4 – Consider differential diagnosis of S3 • A2-wide P2, A2-OS, A2-PK, A2-S3 – Identify diastolic rumble – Determine radiation of murmur e.g.. MR to axilla AuscultationTiming of A2 to OS Interval Say Prrr Timing Severity Other seconds of MS HS’s 0.06 Severe Pada .07-.08 Pata .08-.09 Modsevere Mod Papa 0.10 Mild Tuhuh .12 PK 0.1-0.110 A2-S3 0.12-0.18 Clinical Signs of LV Dysfunction • Hypotension • Pulsus alternans • Reduced volume carotid • LV apical enlargement/displace ment • Sustained apex - to S2 • Soft S1 • Paradoxically split S2 • S3 gallop (not S4 = impaired LV compliance) • Mitral regurgitation • Pulmonary congestion – rales Clinical Signs of RV Dysfunction • With Pulmonary HPT – Loud P2/palpable – PR murmer – RV lift • Common findings RV S4 RV S3 • Without Pulmonary HPT – Soft P2 – No PR – +/- RV lift TR CV wave murmer JVP A wave Pulsatile liver + HJR Edema + Kussmaul’s Causes of RV Dysfunction • LV failure • Pulmonary HPT – 1 – 2 • RV infarction • Pericardial Disease – tamponade – constriction