2011-10-07-Unit-8-Belfast-Medical-Physics-Themography-X
advertisement

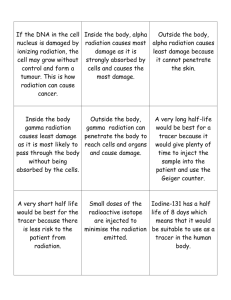
Unit 8 - Medical Physics Nikki Kelso Aims of this Session Production of and uses of thermographic images Introduce the production of & dangers of using x- rays Stochastic & Non Stochastic effects Somatic & Hereditary effects Uses of Radioisotopes & Nuclear Medicine Production & uses of Medical Ultrasound Magnetic Resonance Imaging (MRI) Thermography • Infra-red detectors pick up IR radiation • Amount of radiation increases with temperature therefore thermography allows you to visualise variations in temperature • computer algorithms used to interpret data and produce a usable image Why is this Useful? Certain pathologies cause temperature differentials Thermography detects these with high sensitivity & accuracy Non – invasive NO Ionising Radiation used Types of Diagnosis Sports injuries Breast cancer screening Monitoring of post operative infection What we do in Radiology Departments Plain film radiography Contrast studies Computerised Tomography Radioisotope imaging Ultrasound Magnetic resonance imaging Bone density measurement Positron emission tomography X Rays • Discovered in 1895 by Roentgen • “X” Rays because he didn’t know what they were! • An ionising radiation at a higher level on EM spectrum • Higher frequency or shorter wavelength X-ray Production X rays, the risks and dangers. Ionising Radiation – potentially damaging Damage is influenced by: amount of body tissue irradiated type of body tissue irradiated dose received dose rate Risk minimised using “ALARA” principle Precautionary Measures Legislation Ionising Radiation Regulations 1999 IR(ME)R 2000 In Practice we use radiation protection ALARA principle Staff Protection Not place themselves in the primary beam Use of the inverse square law Use of lead glass panels Use of lead rubber coats/thyroid shields/lead glasses Limit of time spent in fluoroscopy: especially during pregnancy QA of the equipment Dose monitoring Patient Protection Correct exposure factors QA done daily on equipment Collimation of the primary beam Correct focus/film distance Use of appropriate lead rubber protection where appropriate ie gonads/eyes/thyroid Appropriate examination Well trained staff X Ray Effects Stochastic – no threshold for damage Non stochastic – a quantifiable threshold Effects can take place in somatic cells or be passed on (hereditary) Stochastic Effects Probability of the effect of radiation which can be either radiation induced cancers or genetic effects. No safe dose limit Statistically generated Lower doses of radiation Non Stochastic Effects Also called deterministic effects There is usually a threshold below which the effect will not occur Examples are erythema (skin reddening) or epilation (hair loss) Doses are large eg following radiotherapy or as a result of a radiation accident (Chernobyl) Damage caused by radiation SOMATIC caused to the individual GENETIC passed onto future generations How are effects measured? • Sievert is unit of measurement – equivalent to a deposit of 1 joule of energy per kilogram mass of tissue • Relates dose absorbed in tissue to biological damage caused – “effective” dose • This will depend on the type of radiation • Typical background radiation results in an effective dose of 2.4 mSv/year Examples of Doses We’re all exposed to background radiation Chest Skull = few days = few weeks Spine/Abdo = Few months or a year CT Chest = few years Additional risk of cancer per exam 1 in 1,000 to 1 in 1,000,000 Risk of cancer 1 in 3 Image production • Basic form uses photographic film • Denser structures attenuate the x-rays • When film is exposed to x rays it turns black • Image is contrast between two • Contrast can be manipulated using exposure factors and other aids such as contrast media Variations in Contrast Using contrast media Factors affecting contrast Transmission – x-ray photons that pass through the patient unchanged. Absorbtion – x-ray photons that transfer their energy to the patient. Absorbtion is proportional to the degree of attenuation – thickness, density & atomic number Scatter – radiation that changes direction or is modified by decrease in energy as it passes through a body Attenuation – process that x-rays lose power as it travels through matter Plain film radiography Mobile Radiography Mobile unit can be moved to patients bedside, A&E dept or theatre Can be mains or battery powered Can produce images as good as purpose built units. Digital imaging Images stored on computer No films Image manipulation Multiple viewing Storage Volume Physical principles remain the same But because its Windows based “C” arm for angiography Ultrasound Ultrasound uses sound waves to produce images Becoming highly skilled Increasingly specialised Images are very dependent on the ultrasonographers skill Ultrasound images Ultrasound images Computerised Tomography CT explained Tomography tomos – slice graphia – describing Where digital geometry processing is used to generate a three-dimensional image of the internals of an object from a large series of two dimensional x-ray images taken around a single axis of rotation. CT in practice Data is obtained digitally Algorithms allow manipulation of data Windowing is process of using a variety of Hounsfield Units Setting a top and bottom of range allows various tissue types to be imaged Can “get rid” of what you are not interested in Magnetic Resonance Imaging The latest imaging tool Images are similar in appearance to CT but produced without radiation Technology utilises radio waves and a huge magnet to produce images The magnet must be kept cool to allow superconductivity. It has to be cooled with liquid helium to -270 degrees. MR scanner MR Precautions Not everybody can have an MRI scan Metal implants eg cardiac pacemakers, aneurysm clips Tattoos Metallic foreign bodies Pregnant women claustrophobics MRI Images CT versus MR Principles of data collection are the same MR is Non Ionising Better at imaging softer tissue Which Modality to use What are you attempting to image? What level of information do you wish to obtain? How do you wish to manipulate it? What protection measures need to be considered? Radioisotope Imaging What is an isotope? Nuclei of atoms consist of protons and neutrons. The number of protons is called the atomic number The number of protons and neutrons is called the mass number All the atoms of one element with the same atomic number but different mass number are called isotopes Radioisotopes Isotopes behave chemically the same some of the radioisotopes will be radioactive ie emit radiation By attaching these radioactive isotopes to certain pharmaceuticals we can use the emitted radiation to produce images Most commonly used isotope is Technetium99m because it decays by gamma emission What is Radioactivity? Certain elements have isotopes which are unstable The unstable atoms emit particles or energy The particles or energy are radiation The process is unpredictable It is measured in Becquerels – 1 Bq is one “decay” event per second Radiation Types Alpha – helium nuclei stopped by paper Beta – electron, can be stopped by light metal Gamma – EM photon, requires dense material to absorb Half Life The time taken for half of the atoms of a given sample to decay Stays the same for a given isotope regardless of the actual quantity Expressed as a unit of time Can be validated using experimentation and computer modeling Uses for Isotopes Nuclear Medicine Branch of imaging science which uses unsealed radioactive sources Gamma sources are isotope of choice How does it work? Radioactive isotopes are labelled with pharmaceuticals Now known as radiopharmaceuticals Introduced into the body Pharmaceuticals influence tissue type which absorbs isotope Gamma emission is detected by a gamma camera Image is digitally produced Gamma Camera Detects individual Gamma photons Builds up an image over a period of several minutes Useful to show biological (metabolic) processes eg infections/secondary boney cancer deposits Why do we use Nuclear Medicine? Radiopharmaceuticals do not cause much harm in proportion to benefit derived Body will excrete material Radioactivity is short lived – matter of hours Can be used to image anatomy and physiology Can be integrated with other modalities (PET) Production Most useful isotopes are not natural Must be produced by reactors Side product of used nuclear fuel Used uranium fuel has a content of molybdenum99 Easily extracted Technetium99 is a daughter product A few micrograms of molybdenum99 will produce enough technetium 99 to image 10,000 patients Radioisotope/NM Images Positron Emission Tomography latest radiology tool to image patients Cyclotron – particle accelerator 3-30 MeV Positron Emission Tomography PET QUESTIONS?