Case Study 50
advertisement

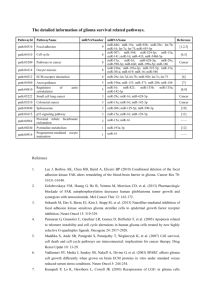
Case Study 50 Edward D. Plowey Case History The patient is a 2 year old girl with normal birth and developmental histories who presented with new onset seizures. A video EEG study confirmed complex partial seizures arising from the left frontal lobe. The patient underwent an MRI of the brain. Question 1 Describe the radiologic abnormality on the following MRI. T2 FLAIR T1 T1 post contrast Answer There is a 4 cm left cingulate gyrus lesion with heterogenous T2 FLAIR and T1 signal abnormalities involving the cortex and subcortical white matter. The FLAIR abnormality focally involves the corpus callosum and crosses the midline. The lesion is surrounded by subtle edema and exerts mild mass effect that expands the left cingulate gyrus and displaces the falx to the right but shows no significant effect on the left frontal horn. No clear contrast enhancement is seen. With involvement of the motor strip and the corpus callosum, the lesion was deemed unresectable. A stereotactic needle biopsy was performed. Question 2 What is the differential diagnosis of this non-enhancing flair lesion in a 2 year old child? Answer The differential diagnosis includes: dysembryoplastic neuroepithelial tumour ganglioglioma diffuse glioma, low grade Glioneuronal hamartoma The radiologic features are less favorable for pleomorphic xanthoastrocytoma and meningioangiomatosis. Question 3 Describe the findings and render a diagnosis for the following intraoperative consultation smear preparation. Answer The intraoperative smear preparation shows a glial neoplasm comprised of spindled cells with delicate bipolar cytoplasmic processes. The nuclear chromatin is coarsely granular. There is prominent gliovascular structuring. There are several entrapped normal-appearing neurons. However, high grade features (mitotic activity, endothelial hyperplasia, necrosis) are not seen. Intraoperative Consultation Diagnosis: A. Neoplastic. B. Low grade glioma. Question 4 Describe the findings on the H&E stained permanent sections of the stereotactic biopsy material. Click here to view virtual slide. Answer Histologic sections demonstrate a glial neoplasm with prominent gliovascular structuring around vessels of variable caliber. A couple of perivascular pseudorosettes are seen in the largest fragment. The glioma cells show spindle nuclei with granular chromatin. No mitotic figures are seen. Endothelial hyperplasia and necrosis are not seen. There are numerous entrapped mature neurons in the tumor. No binucleate neurons or phenotypically indeterminate cells are seen. Question 5 What immunostains will you order to further characterize this neoplasm? Answer GFAP (click hyperlink to view the virtual slide) EMA (click hyperlink to view the virtual slide) Ki67 (click hyperlink to view the virtual slide) Question 6 What further information to these immunostains convey? Answer A GFAP immunostain shows reactivity in tumor cell processes of perivascular pseudorosettes and in reactive glial processes. An EMA immunostain shows perivascular dot-like, microlumen-type immunoreactivity in some of the tumor cells. A Ki67 immunostain confirms a low proliferative index of less that 1%. Question 7 What is the final diagnosis? Answer Diagnosis: ANGIOCENTRIC GLIOMA, WHO GRADE 1. Discussion Angiocentric glioma is new and rare entity in the WHO Classification of Tumors of the Central Nervous System (2007). Angiocentric glioma usually follows a benign clinical course. Most reported cases have been treated with gross total or subtotal resection; a couple of cases have been treated with radiation. In some reported cases, excision of the lesion eliminated seizures. Only 1 reported case has shown recurrence and progression to a high grade glioma following resection. Wang et al. J Neuropathol Exp Neurol. 64:875-81, 2005. Preusser M et al. Am J Surg Pathol. 31:1709-18, 2007. The histogenesis of angiocentric glioma, which shows ependymal features, is unknown. One group of authors has suggested a radial glia origin (Preusser et al, 2007). Discussion Angiocentric glioma occurs mostly in pediatric patients and young adults, but has been reported in elderly adults, and is usually associated with medically intractable epilepsy. A similar case of a frontoparietal angiocentric glioma in a 2 year old child with seizures has been previously reported (J Child Neurol. 24:852-6, 2009. A recent retrospective study by Prayson (Pathology. 42:426-31, 2010) estimates that angiocentric glioma underlies approximately 2% of tumor-associated medically intractable seizures in pediatric patients. Given the non-resectable nature of the tumor in this case, the patient has undergone radiation therapy. A 3 month interval MRI evaluation demonstrated stable to a slight decrease in tumor size.