three dimensional magnetic resonance imaging
advertisement
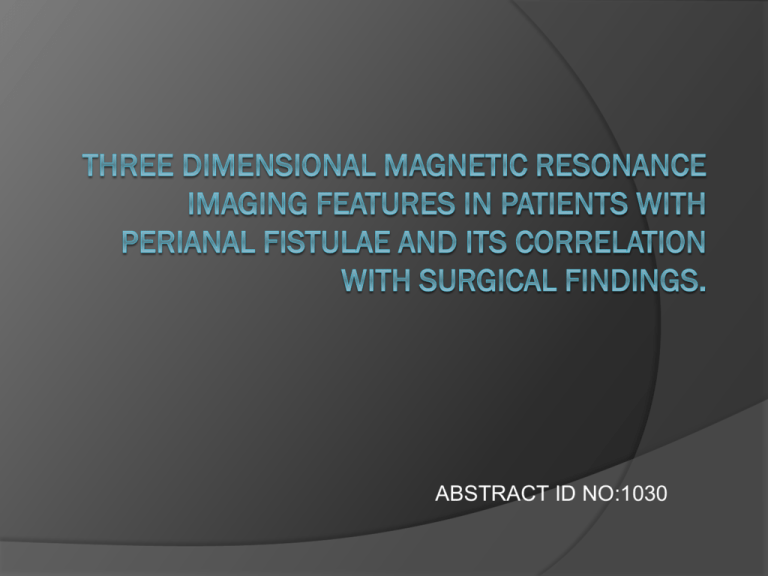
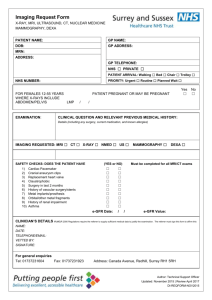
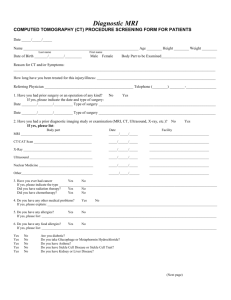
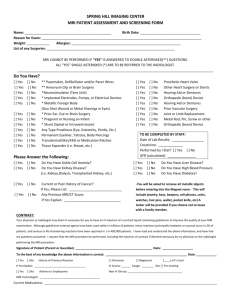
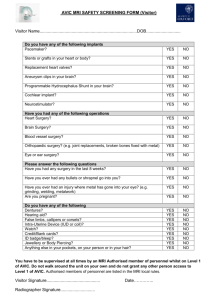
ABSTRACT ID NO:1030 Why this study? Imaging techniques for perianal fistula usually consist of two-dimensional sequences like axial and sagittal T2 ,STIR coronal and post-contrast T1 weighted fat saturated images. Less number of studies have concentrated on 3D sequences and its correlation with surgery The following study uses threedimensional sequences i.e.,syngo SPACE SPACE enables acquisition of high resolution 3D datasets within a clinically acceptable timeframe and without SAR(specific absorption rate) limitations. This study answers whether there is concordance between MRI and surgical findings. It also investigates whether MRI can provide more information that could be missed in surgery and can replace or add to surgical findings as gold standard SPACE - Sampling Perfection with Application optimized Contrasts using different flip angle Evolution, Siemens Medical Solutions, Erlangen, Germany Aims and objectives To assess the three-dimensional magnetic resonance imaging features in patients with perianal fistulae. To correlate MR imaging features with intra-operative surgical findings. Research Question What is the concordance between 3 dimensional MR imaging and surgical findings for perianal fistulae? Materials and Methods Descriptive correlative study Duration of 2 years from June 2012 to May 2014 Sample size n=46 Inclusion Criteria Patients clinically diagnosed as having perianal fistulae. Exclusion criteria Patients having contra-indication to MR imaging like pacemakers, surgical clips, metallic implants. Patients refusing consent or unwilling to undergo MR imaging. Study design Patients referred for MRI with clinical diagnosis of perianal fistulae (n=46) MRI done using SPACE (T2-SPACE-3D for anatomy; T2-SPACE-STIR for track delineation and extension ) No prior preparation No contrast Image evaluation by by radiologist experienced in reading pelvic MR images Parameters studied were primary track(Parks classification),Internal and external opening,,Collections,,Supralevator extension,,Horseshoeing ,St James Hospital University Grading. Findings recorded on a form with formula simulating the standard fistula paper of St. Mark’s Hospital fistula surgery form with some modifications and given to the patient. Surgeon was not blinded to MR findings Surgery on same group of patients Surgeon would record same parameters confirmed with surgery in a similar fistula surgery form Correlation Parameters studied Primary track(Parks classification) Internal and external opening, Collections, Supralevator extension, Horseshoeing if any St James University Hospital Grading Imaging technique 1.5 Tesla MRI unit (MAGNETOM Avanto) Sequences – 2D T2 sagittal T2 weighted SPACE(TR- 1500 milli sec,TE141 milli sec, acquisition time-5 to 6 min, slice thickness-0.9mm) T2 -SPACE -STIR(short tau inversion recovery)(TR-2500 milli sec,TE-127 milli sec,TI-160 milli sec, acquisition time-6 to 7 min, slice thickness-1.2mm) No IV gadolinium PROFORMA Statistical Analysis Surgical findings were taken as the reference standard against which the MR imaging findings were compared. Outcomes were expressed in percentages. Kappa statistics was used for the agreement between MRI and surgery on classification of fistulas with respect to primary track, external and internal opening. Extra yield was expressed in percentages. The entire statistical analysis was conducted using IBM SPSS 20.0 version and graphs were drawn using Microsoft Excel. IMAGES NORMAL ANATOMY 1-Apposed anal mucosa; 2-Internal sphincter; 3-External sphincter(pubococcyg eus part of levator ani); 4-Iliococcygeus part of levator ani; 5-Right Ischioanal fossa; 6-Supralevator plane. Simple Intersphincteric fistula(arrow) (Grade 1 St James University Hospital Classification) Oblique Axial reformats of T2-3D-SPACESTIR showing Simple Intersphincteric fistula (arrow)(Grade 1 St James University Hospital Classification) Oblique Axial reformat of 3D-SPACE T2 weighted image showing Intersphincteric fistula(thick arrow) with a secondary track(thin arrow) (Grade 2 St James University Hospital Classification) (a) (b) Oblique Coronal reformats of (a)3D SPACE T2 weighted image (b) T23D SPACE STIR showing simple trans-sphincteric fistula(arrow) (Grade 3 St James University Hospital Classification) Oblique Coronal reformat of 3D-T2-SPACE-STIR image showing Trans-sphincteric fistula (thick arrow)with a secondary track(thin arrow)(Grade 4 St James University Hospital Classification) Oblique Coronal reformat of 3D-T2-SPACE image showing extrasphincteric fistula(thick arrow) with supralevator extension(curved arrow) and horse-shoe component(thin arrow)(Grade 5 St James University Hospital Classification) Oblique Coronal reformat of 3D-T2-SPACE-STIR image showing extrasphincteric fistula(arrow) with supralevator extension. ( Grade 5 St James University Hospital Classification ) Oblique Coronal(a) and Axial (b) reformats of 3D-T2-SPACE-STIR showing extrasphincteric fistula(thick arrow) with supralevator extension(thin arrow) with anterior supralevator horseshoeing(notched arrow). Oblique Axial reformat of 3D-T2-SPACE-STIR image showing Posterior supralevator horseshoeing(arrow) Oblique Axial(a) and coronal(b) reformats of 3D-T2-SPACE image showing extrasphincteric supralevator fistula with posterior supralevator horseshoeing(arrow) Oblique coronal reformat of 3D-T2-SPACE image showing superficial type of fistula (arrow) Results Age and gender distribution FREQUENCY PERCENT (%) MALES 44 4.3 FEMALES 2 95.7 TOTAL 46 100.0 Intersphincteric 4.40% 10.90% Superficial PRIMARY TRACKS FREQUENCY PERCENT (%) INTERSPHINCTERIC 21 45.6 SUPERFICIAL 12 26.1 TRANS-SPHINCTERIC 6 13 EXTRA-SPHINCTERIC 5 10.9 OTHERS 2 4.4 TOTAL 46 100.0 13% 26.10% 45.60% Trans-sphincteric Extrasphincteric Others Primary tracks PRIMARY TRACKS FREQUENCY PERCENT (%) INTERSPHINCTERIC 21 45.6 SUPERFICIAL 12 26.1 TRANS-SPHINCTERIC 6 13 EXTRA-SPHINCTERIC 5 10.9 OTHERS 2 4.4 TOTAL 46 100.0 Primary tracks Agreement with Surgery Total Frequency Percent (%) Yes 41 89.1 No 5 10.9 46 100.0 Kappa value for agreement between surgery and MRI with respect to primary track was 0.81(almost perfect agreement) Internal opening and External opening Internal opening Frequency Percent (%) External opening Agreement with Yes 44 Frequency Percent (%) Yes 45 97.8 No 1 2.2 46 100.0 95.6 Agreement with Surgery Surgery No 2 4.4 Total cases Total cases 46 100.0 Kappa value for agreement between surgery and MRI with respect to internal and external opening was 0.47 and 0.49 respectively (moderate agreement) Agreement with respect to each type Track No of cases No of cases No of cases detected in detected in MRI misclassified or surgery Agreement missed on MRI Intersphincteric 21 21 0 100% of cases Trans-sphincteric 6 6 0 100% of cases Extrasphincteric 5 5 0 100% of cases Superficial 12 7 5 58% of cases Total 46 41 5 Frequencies of secondary tracks,collections,horseshoeing Secondary tracks Frequency Percent (%) Present 13 28.3 Absent 33 71.7 Total 46 100.0 Collection Frequency Percent (%) Present 6 13 Absent 40 87 Total 46 100 Horseshoeing Frequency Percent (%) Present 4 8.7 Absent 42 91.3 Total 46 100 St James hospital grading St James Hospital Grading 17.40% grade 1 39.10% grade 2 grade 3 19.60% grade 4 grade 5 Others 6.50% 10.90% 6.50% Discussion Of 46 cases most common primary fistulous track was intersphincteric(45.6%) followed by superficial(26.1%),trans-sphincteric(13%) and extrasphincteric(10.9%). MRI correctly classified 41(89.1%) out of 46 cases with respect to the primary track.5 of superficial tracks were misclassified i.e., 2 as intersphincteric,2 trans-sphincteric,1 extrasphincteric. Probable causes can be due to time delay between MRI and surgery causing healing of intersphincteric, trans or extra-sphincteric component or findings could have been missed by surgeon It was less accurate with respect to superficial track where it misclassified 5 among 12 cases(58%). Internal opening In our study, MRI helped the surgeon in knowing the direction of internal opening which was not easily appreciable by perrectal examination, Thus facilitated probing of the tracts and avoided creation of false tracts or internal openings Two cases had internal opening on MRI, which were not revealed at surgery possibly could have partially healed because of conservative treatment External opening Even though clinical examination in lithotomy position could reveal external opening, MRI helped in confirming the presence of external opening and differentiated it from healed scars without any primary fistulous track. It correctly detected external openings in 45(97.8%) out of 46 cases Secondary tracks MRI accurately identified the secondary tracks in 13(28.3%) out of 46 cases. Any hyper intense tubular branch running away from primary track opening into anal canal or ending blindly were considered to be secondary tracks. This provided surgeon to look more keenly for extensions from primary track and excise/drain as much as possible without causing incontinence. Collections Collections were detected in 6(13%) cases. 3 of which were supralevator collections which were additional information given by MRI. Surgeons did not completely drain these collections because of the risk of incontinence. Horse shoeing Horse-shoeing was noted in 4(8.7%) cases. Track crossing to opposite side anterior or posterior to anal canal was detected accurately with MRI. Three of them were supralevator one of them infralevator. Two of them were anterior and other two posterior. Limitations of the study Sample size achieved was less because all patients who underwent MRI could not be followed up in surgery There was significant time delay between MRI and surgery in few of the patients. Contrast was not used in the study. Differentiation of abscesses from collections was difficult Chronic and fibrotic fistulous tracks could not be differentiated from active tracks as former do not show any enhancement with contrast T1 weighted images were not taken therefore, differentiation between hemorrhagic material and active granulation tissue was not possible as former will be hyper intense and latter would be hypo intense. As surgeon was not blinded to MR findings there was always problem of information and misclassification bias Conclusion 3-dimensional MRI is a reliable investigational tool in the evaluation of anorectal fistula and has high agreement with intra-operative findings. 3-dimensional MRI can be a useful investigation in the preoperative assessment of complex anorectal fistulae