Pediatric Associates of Auburn Team Members
advertisement

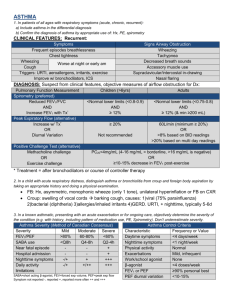
Chapter Quality Network (CQN) Asthma Pilot Project Team Progress Presentation State Name: Alabama Practice Name: Pediatric Associates of Auburn Team Members: Wes Stubblefield, M.D., F.A.A.P., Dianne Carlton, Erica Bentley, L.P.N. Version 2.0 CQN Asthma Project Practice Key Driver Diagram Key Drivers GLOBAL CQN AIM We will build a sustainable quality improvement infrastructure within our practice to achieve measurable improvements in asthma outcomes Specific Aim From fall 2009 to fall 2010, we will achieve measurable improvements in asthma outcomes by implementing the NHLBI guidelines and making CQN’s key practice changes Measures/Goals Outcome Measures: >90% of patients well controlled Process Measures >90% of patients have “optimal” asthma care (all of the following) assessment of asthma control using a validated instrument stepwise approach to identify treatment options and adjust therapy written asthma action plan patients >6 mos. Of age with flu shot (or flu shot recommendation) >90% of practice’s asthma patients have at least an annual assessment using a structured encounter form Engaging Your QI Team and Your Practice *The QI team and practice is active and engaged in improving practice processes and patient outcomes Using a Registry to Manage Your Asthma Population *Identify each asthma patient at every visit *Identify needed services for each patient *Recall patients for follow-up Using a Planned Care Approach to Ensure Reliable Asthma Care in the Office * CQN Encounter Form * Care team is aware of patient needs and work together to ensure all needed services are completed Developing an Approach to Employing Protocols * Standardize Care Processes * Practice wide asthma guidelines implemented Providing Self management Support * Realized patient and care team relationship Interventions Form a 3-5 person interdisciplinary QI Team Formally communicate to entire practice the importance and goal of this project Meet regularly to work on improvement All physicians and team members complete QI Basics on EQIPP Collect and enter baseline data Generate performance data monthly Communicate with the state chapter and leaders within the organization Turn in all necessary data and forms Attend all necessary meetings and phone conferences Select and install a registry tool Determine staff workflow to support registry use Populate registry with patient data Routinely maintain registry data Use registry to manage patient care & support population management Select template tool from registry or create a flow sheet Determine workflow to support use of encounter form at time of visit Use encounter form with all asthma patients Ensure registry updated each time encounter form used Monitor use of encounter form Select & customize evidence-based protocols for your office Determine staff workflow to support protocol, including standing orders Use protocols with all patients Monitor use of protocols Obtain patient education materials Determine staff workflow to support SMS Provide training to staff in SMS Assess and set patient goals and degree of control collaboratively Document & Monitor patient progress toward goals Link with community resources Progress Summary Since Learning Session 1 1. Beginning with LS1, implemented study on a limited basis with one provider and expanded to all asthmatic office patients with all providers. 2. Developed reliable process for identifying asthmatic patients and distributing encounter forms in office flow. 3. Increased identification of asthmatic patients through use of encounter form and spirometry per guidelines. 4. Increased evidence-based guideline treatment of asthmatic patients by using NLHBI stepwise approach to therapy. 5. Improved outcomes with increased flu shot recommendations for all asthmatic patients and regular use of spirometry in follow up. 6. Improved follow up reliability with identification and missed visit calls. % of Patients with AAP Spirometry within 1-2 years F/U appt recommended Optimal Asthma Care PDSA Cycle – Follow up PDSA Title: Plan: Recommend follow up to all study patients per guidelines, expanded to all asthma patients with all providers. Do: Asthma patient tagged in EHR. Each visit, symptoms/medications reviewed by L.P.N. and M.D. and follow up recommended as appropriate or per guidelines. Study: Noted that some patients were not keeping scheduled appointments for follow up. Implemented “no show” strategy, front office staff to notify M.D. and L.P.N. if patient missed appointment. L.P.N. contacted family personally to stress the importance of keeping scheduled appointments and reschedule. Noted improvement with keeping appointments as expected. Act: At follow up visit, asthma action plan reviewed, follow up spirometry scheduled or performed, if indicated. Asthma action plan modified as needed. PDSA Ramps P D P D P D P D S A S A S A TEST 4 What:: AAP to all asthmatic patients Who (population): all asthmatic pts Who (executes): Nurse hands out form, MD completes Where: Triage/Exam Room When: 45 days S A TEST 4 What:: Spirometry f/u per guidelines in addition to initial spirometry for diagnosis Who (population): All asthmatics Who (executes): MD orders, nurse performs Where: Exam room or Lab When: 45 days P D P D S A TEST 3 What:: AAP to all identified pts Who (population): All identified pts Who (executes): MD Where: Exam room When: 30 days S A TEST 3 What:: Spirometry to asthmatics per guidelines Who (population): All asthmatic patients Who (executes): MD orders, nurse peforms Where: Exam room or Lab When:30 days P D P D P D S A S A S A TEST 2 What:: Provide spirometry per guidelines (current or new diagnosis only) Who (population): Limited population Who (executes): MD orders, nurse performs Where: Exam room or Lab When: 15 days TEST 2 What:: Distribute AAP to all identified pts Who (population): Alll identified pts Who (executes): Nursing staff Where: Triage Area When: 15 days P D P D S A S A S A Asthma Action Plan (AAP) TEST 1 What:: Identify pts needing current spirometry Who (population): Limited population Who (executes): MD review of chart Where: Exam room, EHR When: Immediately Spirometry TEST 3 What:: EHR tagging of asthmatic patients to follow up Who (population): all asthmatic patients Who (executes): Front Desk Where: Front Desk When: 45 days TEST 2 What:: Expanding follow up to call asthmatic patients Who (population): all asthmatic patients Who (executes): MD Where: Exam room When: 15 days P D TEST 1 What:: Identifiy asthmatic patients for study Who (population): Limited population Who (executes): MD/Nurse Where: Office flow, MD work area When: Immediately TEST 4 What:: Call back for missed appts Who (population): All identified pts Who (executes): MD orders through EHR Front desk performs Where: Exam room, front desk When: 60 days TEST 1 What:: Recommended f/u to study patients per guidelines Who (population): Study patients only Who (executes): MD Where: Exam room When: Immediately Follow up Office Visit Prework During Office Visit ASTHMA Asthma PATIENTS patients INDENTIFIED identified by BYEHR EHR FLASHER PATIENT CHECKS IN AT FRONT DESK – LPN REVIEWS PATIENT HISTORY - I.E., EXPOSURE TO CIGARETTE SMOKE, FLU SHOT STATUS, MEDICATION LIST PEDIATRIC ASSOCIATES OF AUBURN LPN GIVES ASTHMA ENCOUNTER FORM TO PARENT M.D. REVIEWS ENCOUNTER FORM – COMPLETES ENCOUNTER FORM IN EHR REVIEWS HISTORY OF PROGRESS OR FAILURES WITH CURRENT TREATMENT. M.D. PROVIDES EDUCATION & ASSESSES NEED FOR SPIROMETRY AND/OR ALTERNATE MEDICATION PLAN LPN PERFORMS SPIROMETRY IF ORDERED Post Visit Activities ANY NEW OR UNIDENTIFIED PATIENTS ARE IDENTIFIED DURING TRIAGE BY LPN AND GIVEN ASTHMA ENCOUNTER FORM FRONT DESK CHECKS FOR F/U INSTRUCTIONS AT CHECKOUT FOR ALL ASTHMA PATIENTS – F/U SCHEDULED AS INDICATED BY M.D. NEW/UNIDENTIFIED ASTHMA PATIENTS CHARTS ARE FLAGGED IN EHR ENCOUNTER FORMS PLACED ON M.D.’S DESK M.D. ENTERS DATA IN TO EQUIPP – SENDS FORM TO FRONT OFFICE FOR SCAN IN TO CHART FRONT OFFICE NOTIFIES LPN AND M.D OF ANY ASTHMA PATIENT MISSED APPTS M.D. REVIEWS PATIENT CHART – LPN CONTACTS PARENTS TO RESCHEDULE FOLLOW UP APPT M.D. REVIEWS SPIROMETRY RESULTS – ADJUSTS MEDS AS NEEDED – ADVISES F/U AS PER RESULTS CQN Encounter Form Key Learnings Obviously, although we felt we performed quality asthma care, our experience through this project tells us otherwise. However, with a little work and some direction through the collaborative, we were able to increase our optimal asthma care into the goal range. Our data have not shown significant increases in our well controlled patients and admission rates yet, but we plan to see that increase over the next few months. Barriers and Successes • Barriers: – Being a small office, implementing any change is usually quick, but requires increased time for the staff. We have very little extra staff to handle increased workload (3 non-clinical staff including office manager). • Successes: – We feel that we have integrated this project into our workflow such that, even when busy, we are able to complete our forms. – We were also able to integrate the CQN form into EHR. Future Plans • Identify all prior asthmatic patients through practice management software and ICD-9 review. • Implement registry through RMD. • More formalized asthma education, e.g. spacer teaching, MDI teaching, DPI teaching • Formalized staff training • More integration of project with EHR (starting with encounter form – Thanks Partners in Peds!!)