Radiation Protection in Nuclear Medicine
advertisement
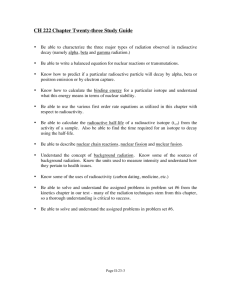
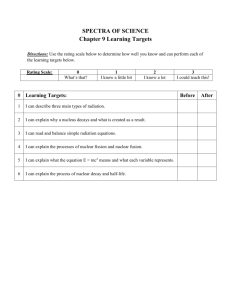
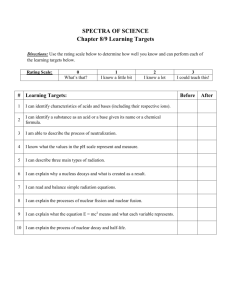
IAEA Training Material on Radiation Protection in Nuclear Medicine Part 3 Principles of radiation protection and the international framework Regulatory requirements Objective To become aware of the ICRP’s conceptual framework and the International Basic Safety Standards requirement (BSS) and related Safety Guides in radiation protection in medical field. Nuclear Medicine Part 3. Principles of Radiation Protection 2 Content Principles of Radiation Protection International Basic Safety Standards Regulatory Control Nuclear Medicine Part 3. Principles of Radiation Protection 3 IAEA Training Material on Radiation Protection in Nuclear Medicine Part 3. Module 3.1. Basic principles of radiation protection Do we need radiation protection in nuclear medicine? Nuclear Medicine Part 3. Principles of Radiation Protection 5 What can Radiation Do? Death Cancer Skin Burns Cataract Infertility Genetic effects Nuclear Medicine Part 3. Principles of Radiation Protection 6 What can Radiation Do? Deterministic effects death, skin burns, cataract, infertility Stochastic effects cancer, genetic effects Nuclear Medicine Part 3. Principles of Radiation Protection 7 EFFECT Stochastic effects Deterministic effects cataract infertility erythema epilation DOSE 500 mSv cataract 150 mSv for sterility (temporary-males) 2500 mSv for ovarian Nuclear Medicine Part 3. Principles of Radiation Protection 8 Objectives of Radiation Protection PREVENTION of deterministic effect LIMITING the probability of stochastic effect Nuclear Medicine Part 3. Principles of Radiation Protection 9 The Need for Protection Applies to all Dose Levels It is generally assumed that even very small doses of ionizing radiation can potentially be harmful (linear no threshold hypothesis) Therefore, persons must be protected from ionizing radiation at all dose levels Nuclear Medicine Part 3. Principles of Radiation Protection 10 Who should be Protected in Nuclear Medicine? Patient Members of his/her family Worker General public Nuclear Medicine Part 3. Principles of Radiation Protection 11 How should the people be protected? Optimize protection Justify the exposure Dose limitations Nuclear Medicine Part 3. Principles of Radiation Protection 12 This is the system of radiological protection as defined by the ICRP (International Commission on Radiological Protection) Nuclear Medicine Part 3. Principles of Radiation Protection 13 What is the ICRP? A non-governmental professional organization established in 1928 by the International Congress of Radiology Nuclear Medicine Part 3. Principles of Radiation Protection 14 What is the ICRP? A group of recognized leaders in the field of radiation protection concerned with the protection of humans from ionizing radiation official relationships with WHO, IAEA, ICRU convenes task groups of experts to address particular issues issues reports and recommendations Nuclear Medicine Part 3. Principles of Radiation Protection 15 Ionizing Radiation We live with 1-3 mSv/y Can kill 4000 mSv Is there a safe point? If not, how to deal with the problem? Nuclear Medicine Part 3. Principles of Radiation Protection 16 To protect the people taking into account the main objectives of radiation protection the system of protection should be based on: A. Individual-related system – dose limit (absolute maximum risk that society can accept), optimization B. Source-related system – limitation on source, source related constraints – basic protection + environmental + individual protection (by shielding, protective clothing...) Nuclear Medicine Part 3. Principles of Radiation Protection 17 A. B. Main site of protection Environment Nuclear Medicine Part 3. Principles of Radiation Protection 18 The ICRP Recommendations ICRP publication 103 - 2007 The recommended system of radiation protection is based upon 3 principles: Nuclear Medicine Benefit of a practice must offset the radiation detriment (justification) Exposures and likelihood of exposure should be kept as low as reasonably achievable, economic and social factors being taken into account (optimization) Dose limits should be set to ensure that no individual faces an unacceptable risk in normal circumstances Part 3. Principles of Radiation Protection 19 ICRP 103 Weighs all existing data to arrive at quantitative recommendations for risk, detriment, dose and dose rate weighting factors Considers exposure to humans only Considers exposure in three categories: occupational, medical, public Nuclear Medicine Part 3. Principles of Radiation Protection 20 IAEA BSS (2011) - glossary Occupational Exposure: “All exposures of workers incurred in the course of their work, with the exception of exposures excluded from the Standards and exposures from practices or sources exempted by the Standards.” Nuclear Medicine Part 3. Principles of Radiation Protection 21 IAEA BSS (2011) - glossary Medical Exposure: “Exposure incurred by patients as part of their own medical or dental diagnosis or treatment; by persons, other than those occupationally exposed, knowingly while voluntarily helping in the support and comfort of patients; and by volunteers in a programme of biomedical research involving their exposure.” Nuclear Medicine Part 3. Principles of Radiation Protection 22 IAEA BSS (2011) - glossary Public Exposure: “Exposure incurred by members of the public from radiation sources, excluding any occupational or medical exposure and the normal local natural background radiation but including exposure from authorized sources and practices and from intervention situations.” Nuclear Medicine Part 3. Principles of Radiation Protection 23 Justification No use of ionizing radiation is justified if there is no benefit All applications must be justified This implies to even the smallest exposures that are potentially harmful and the risk must be offset by a benefit Nuclear Medicine Part 3. Principles of Radiation Protection 24 Risk/Benefit Analysis Need to evaluate the benefits of radiation - an easy task in the case of nuclear medicine Radiation is the diagnostic and therapeutic agent Assessment of the risks requires the knowledge of the dose received by persons Nuclear Medicine Part 3. Principles of Radiation Protection 25 Optimization When radiation is to be used then the exposure should be optimized to minimize any possibility of detriment. Optimization is “doing the best you can under the prevailing conditions” Need to be familiar with techniques and options to optimize the application of ionizing radiation - this is really the main objective of the present course Nuclear Medicine Part 3. Principles of Radiation Protection 26 Optimization (contd..) Must take into account the resources available - this includes economic circumstances Often a tricky question - where shall we stop, how much shielding should we really use? Governed by the optimization principle Nuclear Medicine Part 3. Principles of Radiation Protection 27 Optimization Principle As Low As Reasonably Achievable This means radiation exposure should be limited as much as possible keeping in mind the risk-benefit relation of radiation and its applications. For example, it is unreasonable to refuse an X-ray after a bone fracture because statistically this may shorten your life expectancy by one day. The benefits of the Xray with its diagnostic value by far outweigh the risk associated with the radiation exposure. Nuclear Medicine Part 3. Principles of Radiation Protection 28 …very much in line with the rest of real life Both justification and optimization are part of all strategies when handling potentially harmful substances or dealing with risks: there must be a benefit the risk should be kept as low as possible Same for household chemicals, drugs, traffic, travel, sports, …. Nuclear Medicine Part 3. Principles of Radiation Protection 29 A comment on the optimization principle (As Low As Reasonably Achievable) Issues which are often subject of discussion: L … what is a low dose? R … what is reasonable? Nuclear Medicine Part 3. Principles of Radiation Protection 30 What is Low? Nuclear Medicine It can be very costly to consider every dose level explicitly Discussions are ongoing about dose levels below ‘regulatory concern’ A potential starting point are doses from natural background which are inevitable and one can assume organisms have adapted to them Part 3. Principles of Radiation Protection 31 Average annual doses in mSv from natural sources in European countries Nuclear Medicine Part 3. Principles of Radiation Protection 33 What is Radon (222Rn)? It is a radioactive gas that exists everywhere in the atmosphere It is a member of the 238U series It is formed by the decay of 226Ra Nuclear Medicine Part 3. Principles of Radiation Protection 34 What is Radon (222Rn)? Half-life 3.82 days It is an alpha emitter decaying to 218Po 218Po is also an alpha emitter (T½ 3 min) Other important decay products are 214Po (a, T½ 0.164 msec) and 214Bi (b, T½ 19.9 min) Nuclear Medicine Part 3. Principles of Radiation Protection 35 Why is Radon a Problem? The hazard arises from the inhalation of its decay products which are not gaseous Most of the decay products become attached to aerosols in the atmosphere and are deposited in the conducting airways and in the lung during respiration. Nuclear Medicine Part 3. Principles of Radiation Protection 36 Other important contributions to natural exposure: Potassium-40 40K constitutes 120 parts per million of stable potassium which is an essential trace element in every human body 40K has a half-life of 1.28 x 109 years, decaying by beta emission (Emax 1.3 MeV) An 80 kg adult male contains about 180 g of potassium -> 18 mg of 40K This gives an annual internal effective dose of 170 µSv Nuclear Medicine Part 3. Principles of Radiation Protection 37 The cosmic rays contribution to the background radiation varies markedly with altitude. Note, that at cruising altitude in a Boeing 747 the dose rate is approximately 5 µSv/h Nuclear Medicine Part 3. Principles of Radiation Protection 38 Example of Radiation Exposure to Aircrew to Cosmic Radiation Exposure of New Zealand aircrew International Routes 1000 hours per year, with 90% of the time at an altitude of 12 km 6.5 mSv annual dose from cosmic radiation Domestic Routes 1000 hours per year, with 70% of the time at an altitude of 11 km 3.5 mSv annual dose from cosmic radiation Adapted from L Collins 2000 Nuclear Medicine Part 3. Principles of Radiation Protection 39 Average Background Doses UNSCEAR 2008 Report WORLDWIDE AVERAGE DOSES Source Effective dose Typical range (mSv per year) (mSv per year) External exposure Cosmic rays Terrestrial gamma rays 0.4 0.5 0.3-1.0 0.3-0.6 1.2 0.3 0.2-10 0.2-0.8 2.4 1–10 Internal exposure Inhalation Ingestion Total Nuclear Medicine Part 3. Principles of Radiation Protection 40 What is ‘Reasonable’? Depends on ‘prevailing conditions’ including economic cultural Should be based on a risk/benefit analysis of the practice Nuclear Medicine Part 3. Principles of Radiation Protection 41 Dose Limitation No dose limitation for medical exposure of the patient - it is always assumed that the benefits for the patient outweigh the risks Limits need to be applied for public and occupational exposures Nuclear Medicine Part 3. Principles of Radiation Protection 42 Limits and Constraints Dose limits are one of the three principles of protection as introduced by ICRP and BSS. Fixed dose limits are recommended by ICRP and often enforced by a national legal process (Radiation Protection Legislation). Dose constraints are used in an optimization process to guide planning. Constraints and the importance thereof may be subject to change to achieve the optimum solution to a problem (Best practice guidelines). Nuclear Medicine Part 3. Principles of Radiation Protection 43 Optimization and Dose Limitation It is NOT the aim to get close to the limit values - the aim is to get as low as reasonably achievable Is part of risk management Keeps the risks of dealing with ionizing radiation of the same order as other risks Nuclear Medicine Part 3. Principles of Radiation Protection 44 IAEA Training Material on Radiation Protection in Nuclear Medicine Part 3. Module 3.2. International Basic Safety Standards THE INTERNATIONAL ATOMIC ENERGY AGENCY IAEA was established in 1957 and has the following functions: - Safeguards (verification of peaceful uses) - Technology (fostering the transfer of) - Safety Nuclear Medicine Part 3. Principles of Radiation Protection 46 To service international conventions IAEA RADIATION SAFETY FUNCTIONS Article III.A.6 of its Statute To establish standards of radiation safety Nuclear Medicine To provide for the application of these standards Part 3. Principles of Radiation Protection 47 BASIC SAFETY STANDARDS 1996 The purpose of the Standards is to establish basic requirements for protection against the risk associated with exposure to ionizing radiation and for the safety of radiation sources that may deliver such exposure. The Standards lay down basic principles and indicate the different aspects that should be covered by an effective radiation protection programme 2011 Nuclear Medicine The Standards are aimed to serve as a practical guide for public authorities and services, employers and workers, specialized radiation protection bodies, enterprises and safety and health committees. Part 3. Principles of Radiation Protection 48 History First Basic Safety Standards Revised Basic Safety Standards Revised and Joint with FAO, ILO, OECD/NEA, WHO ICRP published revised recommendations Consultants, Senior experts meetings, ad hoc working groups, technical committees 6th draft circulated to all member states 7th Draft approved by IAEA Board of Governors Publication of Interim Version S.S.115I Formal approval by co-sponsoring organizations Publication of S.S.115 Interim Revised BSS Tentative New BSS Publication Nuclear Medicine Part 3. Principles of Radiation Protection 1962 1967 1982 1991 1991, 1992, 1993 March 1994 Sept 1994 1994 1994-1996 1996 2011 2012/2013 49 BSS Jointly sponsored by: THE FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS (FAO) THE INTERNATIONAL ATOMIC ENERGY AGENCY (IAEA) THE INTERNATIONAL LABOUR ORGANIZATION (ILO) THE NUCLEAR ENERGY AGENCY OF THE OECD (NEA) THE PAN AMERICAN HEALTH ORGANIZATION (PAHO) AND THE WORLD HEALTH ORGANIZATION (WHO) Nuclear Medicine Part 3. Principles of Radiation Protection 50 The IAEA’s International Standards are based on estimates on radiation health effects made by the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) and radiation protection recommendations of the International Commission on Radiological Protection (ICRP) Nuclear Medicine Part 3. Principles of Radiation Protection 51 THE SCIENTIFIC BASIS OF THE STANDARDS Non-governmental ICRP Principles Recommendations Governmental UNSCEAR IAEA Effects Standards Nuclear Medicine Part 3. Principles of Radiation Protection 52 THE INTERNATIONAL GOVERNMENTAL CONSENSUS ON THE HEALTH EFFECTS OF RADIATION UNSCEAR The United Nations Scientific Committee on the Effects of Atomic Radiation Nuclear Medicine Part 3. Principles of Radiation Protection 53 What is UNSCEAR? UNSCEAR is a committee of the UN General Assembly. It was established in 1955 Nuclear Medicine Part 3. Principles of Radiation Protection 54 How UNSCEAR Works? MOLECULAR BIOLOGY JUDGMENT ON PLAUSIBILITY AND ESTIMATES RADIOEPIDEMIOLOGY Nuclear Medicine RADIOBIOLOGY Part 3. Principles of Radiation Protection 55 UNSCEAR provides estimates of the health effects of exposure to ionizing radiation Such as…… Nuclear Medicine Part 3. Principles of Radiation Protection 56 Life-time risk of dying from radiation induced cancer ≈ 5% per sievert UNSCEAR has recently (2008) further assessed the cancer risk from radiation exposures. For a population of all ages and both genders, the lifetime risk of dying from radiation induced cancer after an acute dose of 1000 mSv is about 9% for men and 13% for women or 11% as a mean. Applying a DDREF of 2, these data confirm the 10 years old ICRP estimate. Nuclear Medicine Part 3. Principles of Radiation Protection 57 ICRP The International Commission of Radiological Protection (ICRP) makes recommendations relating to radiation protection Nuclear Medicine Part 3. Principles of Radiation Protection 58 Recommendations of the ICRP Prepared typically by a task group which includes other experts Approved by the full commission Published in the journal “Annals of the ICRP” Have no legal status themselves however, are typically the foundation onto which national legislation is built Nuclear Medicine Part 3. Principles of Radiation Protection 59 Finally, on the basis of UNSCEAR estimates and ICRP recommendations, the IAEA establishes international standards on radiation and nuclear safety Nuclear Medicine Part 3. Principles of Radiation Protection 60 Hierarchy of IAEA Documents Safety Fundamentals Safety Standards Approved by IAEA Board of Governors Nuclear Medicine Part 3. Principles of Radiation Protection 61 Hierarchy of IAEA Documents Supported by Safety Fundamentals and Standards Safety Guides Safety Practices TECDOCs Technical Reports Proceedings Nuclear Medicine Part 3. Principles of Radiation Protection 62 Nuclear Medicine Part 3. Principles of Radiation Protection 63 Layout OF BSS (2011) INTRODUCTION: Background, objective, scope, Structure GENERAL-REQUIREMENTS FOR PROTECTION AND SAFETY Definitions, Interpretation, Application of the principles of Radiation protection Responsibilities Management requirements Scope PLANNED EXPOSURE SITUATIONS Generic requirements Public exposure EMERGENCY EXPOSURE SITUATIONS Occupational exposure EXISTING EXPOSURE SITUATIONS Medical exposure SCHEDULES Nuclear Medicine Part 3. Principles of Radiation Protection 64 • • • • • • • • • Nuclear Medicine Definitions Interpretation Resolution of conflicts Entry into force Application of the principles of radiation protection Responsibilities of the government Responsibilities of the regulatory body Responsibilities for protection and safety Management requirements Part 3. Principles of Radiation Protection 65 System of protection and safety The standards are based on the following safety principles Principle 1: Responsibility for safety Principle 2: Role of government Principle 3: Leadership and management for safety Principle 4: Justification of facilities and activities Principle 5: Optimization of protection Principle 6: Limitation of risks to individuals Principle 7: Protection of present and future generations Principle 8: Prevention of accidents Principle 9: Emergency preparedness and response Principle 10: Protective actions to reduce existing or unregulated radiation risks The three general principles of radiation protection, which concern justification, optimization of protection and application of dose limits, are expressed in Safety Principles 4, 5, 6 Nuclear Medicine Part 3. Principles of Radiation Protection 66 QUALIFIED EXPERTS 2.21. The government shall ensure that requirements are established for: (b) the formal recognition of qualified experts; Nuclear Medicine Part 3. Principles of Radiation Protection 67 Nuclear Medicine Specifies who are the responsible organisations and individuals, including the Regulatory Authority. Defines the administrative requirements, including licensing and registration. Uses the dose limitation system introduced in ICRP report 60.. Part 3. Principles of Radiation Protection 68 OBJECTIVE (1.38) ” These Standards establish requirements for the protection of people and the environment from harmful effects of ionizing radiation and for the safety of radiation sources”. Nuclear Medicine Part 3. Principles of Radiation Protection 69 SCOPE (1.45) These Standards apply to human activities involving radiation exposure that are: (i) Carried out in a State which chooses to adopt these Standards or which requests any of the Sponsoring Organizations to provide for the application of these Standards; (ii) Undertaken by States with the assistance of the Food and Agriculture Organization of the United Nations, the International Atomic Energy Agency, the International Labour Organization, the Pan American Health Organization, the United Nations Environment Programme or the World Health Organization, in the light of relevant national rules and regulations; (iii) Carried out by the IAEA or involving the use of materials, services, equipment, facilities and non-published information made available by the IAEA or at its request or under its control or supervision; or (iv) Carried out under any bilateral or multilateral arrangement whereby the parties request the IAEA to provide for the application of these Standards Nuclear Medicine Part 3. Principles of Radiation Protection 70 PRACTICE Any human activity that introduces additional sources of exposure or additional exposure pathways, or modifies the network of exposure pathways from existing sources, so as to increase the exposure or the likelihood of exposure of people or the number of people exposed Nuclear Medicine Part 3. Principles of Radiation Protection 71 PRACTICES Very broad definition (a) production of sources and use of radiation and radioactive substances for medical, industrial, veterinary, agricultural, education, training and research purposes (b) nuclear fuel cycle (c) exposure to natural sources specified by Regulatory Authority as requiring control (d) anything else specified by Regulatory Authority. Nuclear medicine is a practice Nuclear Medicine Part 3. Principles of Radiation Protection 72 PRACTICE Existing Annual Dose Pre- existing annual dose expected additional annual dose attributable to the source CONTROL Introduction, operation and decommissioning of a practice Nuclear Medicine Part 3. Principles of Radiation Protection Post-existing annual dose Time 73 Safety measure Any action that might be taken, condition that might be applied or procedure that might be followed to fulfil the basic requirements of Safety Requirements. Protective action An action for the purposes of avoiding or reducing doses that might otherwise be received in an emergency exposure situation or an existing exposure situation. Nuclear Medicine Part 3. Principles of Radiation Protection 74 SITUATIONS REQUIRING INTERVENTION •emergency exposure situations requiring protective actions •chronic exposure situations requiring remedial actions Nuclear Medicine Part 3. Principles of Radiation Protection 75 Remedial Action The removal of a source or the reduction of its magnitude (in terms of activity or amount) for the purposes of preventing or reducing exposures that might otherwise occur in an existing exposure situation Nuclear Medicine Part 3. Principles of Radiation Protection 76 INTERVENTION Existing annual dose CONTROL Averted annual dose by the intervention Pre-intervention existing annual dose Time Intervention Nuclear Medicine Post-intervention existing annual dose Part 3. Principles of Radiation Protection 77 EXCLUSIONS Exposures deemed to be unamenable to control are excluded from the scope of these Standards, e.g. 40K in the body, cosmic radiation at earth’s surface and unmodified concentrations of radionuclides in most raw materials. Nuclear Medicine Part 3. Principles of Radiation Protection 78 EXEMPTION CRITERIA (a) Radiation risks arising from the practice or a source within a practice are sufficiently low as not to warrant regulatory control, with no appreciable likelihood of situations that could lead to a failure to meet the general criterion for exemption; or (b) Regulatory control of the practice or the source would yield no net benefit, in that no reasonable control measures would achieve a worthwhile return in terms of reduction of individual doses or of health risks. Nuclear Medicine Part 3. Principles of Radiation Protection 79 EXEMPTION Practice or source may be exempted if - effective dose < 10mSv in a year or - The determination by a regulatory body that a source or practice need not be subject to some or all aspects of regulatory control on the basis that the exposure and the potential exposure due to the source or practice are too small to warrant the application of those aspects or that this is the optimum option for protection irrespective of the actual level of the doses or risks. Nuclear Medicine Part 3. Principles of Radiation Protection 80 GENERIC REQUIREMENTS 3.10. The government or the regulatory body shall determine which practices or sources within practices are to be exempted from some or all of the requirements of these Standards, including the requirements for notification, registration or licensing, using as the basis for this determination the criteria for exemption specified in Schedule I or any exemption levels specified by the regulatory body on the basis of these criteria • registration authorization • licensing Each application for authorization requires assessment of the nature, likelihood and magnitude of the expected exposures due to the source and shall take all necessary measures for protection and safety. The regulatory body shall approve which sources, including materials and objects, within notified or authorized practices may be cleared from further regulatory control. Nuclear Medicine Part 3. Principles of Radiation Protection 81 GENERIC REQUIREMENTS FOR PLANNED EXPOSURE SITUATIONS Requirement 6: Graded approach Requirement 7: Notification and authorization Requirement 8: Exemption and Clearance Requirement 9: Responsibilities of registrants and licensees in planned exposures Requirement 10: Justification of practices Requirement 11: Optimization of protection and safety Requirement 12: Dose limits Nuclear Medicine Part 3. Principles of Radiation Protection 82 Graded Approach The application of the requirements of these Standards in planned exposure situations shall be commensurate with the characteristics of the practice or the source within a practice, and with the magnitude and likelihood of the exposures. 3.6. The application of the requirements of these Standards shall conform to any requirements specified by the regulatory body, in accordance with a graded approach; however, not all the requirements of these Standards are relevant for every practice or source, nor for all the actions specified in para. 3.5. Nuclear Medicine Part 3. Principles of Radiation Protection 83 Requirement 7 Notification Authorization (Registration/Licensing) Nuclear Medicine Part 3. Principles of Radiation Protection 84 Notification BSS 3.7.” Any person or organization intending to carry out any of the actions specified in para. 3.5 shall submit a notification to the regulatory body of such an intention”. “Notification is required for consumer products only with respect to manufacture, assembly, maintenance, import, distribution and, in some cases, disposal.” Nuclear Medicine Part 3. Principles of Radiation Protection 85 Authorized Legal Persons: Registrants and Licensees BSS 3.13. “Registrants and licensees shall bear the responsibility for setting up and implementing the technical and organizational measures that are necessary for protection and safety for the practices and sources for which they are authorized”. “Registrants and licensees may designate suitably qualified persons to carry out tasks relating to these responsibilities, but they shall retain the prime responsibility for protection and safety.” Nuclear Medicine Part 3. Principles of Radiation Protection 86 Authorization: Registration or Licensing BSS 3.8. Any person or organization intending to carry out any of the actions specified in para. 3.5 shall, unless notification alone is sufficient, apply to the regulatory body for authorization17, which shall take the form of either registration18 or licensing. 3.9. Any person or organization applying for authorization: (a) Shall submit to the regulatory body the relevant information necessary to support the application; (b) Shall refrain from carrying out any of the actions specified in para. 3.5 until the registration or licence has been granted; (c) Shall assess the nature, likelihood and magnitude of the expected exposures due to the source and shall take all necessary measures for protection and safety; (d) Shall, if there is a possibility for an exposure to be greater than a level as specified by the regulatory body, have a safety assessment made and submitted to the regulatory body as part of the application; (e) Shall, as required by the regulatory body, have an appropriate prospective assessment made for radiological environmental impacts, commensurate with the radiation risks associated with the facility or activity. This applies to nuclear medicine Nuclear Medicine Part 3. Principles of Radiation Protection 87 Responsibilities Main responsibilities: registrants and licensees employers Subsidiary include: suppliers workers health professionals qualified experts Nuclear Medicine Part 3. Principles of Radiation Protection 88 Responsibilities of registrants and licensees in planned exposure situations BSS 3.13. Registrants and licensees shall bear the responsibility for setting up and implementing the technical and organizational measures that are necessary for protection and safety for the practices and sources for which they are authorized. Registrants and licensees may designate suitably qualified persons to carry out tasks relating to these responsibilities, but they shall retain the prime responsibility for protection and safety. Registrants and licensees shall document the names and and responsibilities of persons designated to ensure compliance with the requirements of these Standards. Nuclear Medicine Part 3. Principles of Radiation Protection 89 Responsibilities Emergency Situations Occupational Exposure Medical Exposure Public Exposure Safety of Sources Nuclear Medicine Part 3. Principles of Radiation Protection 90 Requirement 10: Justification of practices The government or the regulatory body shall ensure that only justified practices are authorized. 3.16. The government or the regulatory body, as appropriate, shall ensure that provision19 is made for the justification of any type of practice20 and for review of the justification, as necessary, and shall ensure that only justified practices are authorized Nuclear Medicine Part 3. Principles of Radiation Protection 91 Requirement 11: Optimization of protection and safety The government or regulatory body shall establish and enforce requirements for the optimization of protection and safety, and registrants and licensees shall ensure that protection and safety is optimized. Nuclear Medicine Part 3. Principles of Radiation Protection 92 Requirement 12: Dose limits The government or the regulatory body shall establish dose limits for occupational exposure and public exposure, and registrants and licensees shall apply these limits. Nuclear Medicine Part 3. Principles of Radiation Protection 93 DOSE LIMITATION 3.26 “The government or the regulatory body shall establish and the regulatory body shall enforce compliance with the dose limits specified in Schedule III for occupational exposures and public exposures in planned exposure situations.” Nuclear Medicine Part 3. Principles of Radiation Protection 94 RADIATION PROTECTION REQUIREMENTS FOR MEDICAL EXPOSURES Justification of medical exposures positive net benefit Optimization of Protection and Safety Constraints for medical exposures of various types guidance levels for medical exposure. Nuclear Medicine Part 3. Principles of Radiation Protection 95 REQUIREMENTS FOR MEDICAL EXPOSURES Justification of Medical Exposures 3.154 “Medical exposures shall be justified by weighing the expected diagnostic or therapeutic benefits42 that they yield against the radiation detriment that they might cause, with account taken of the benefits and the risks of available alternative techniques that do not involve medical exposure”. Nuclear Medicine Part 3. Principles of Radiation Protection 96 REQUIREMENTS FOR MEDICAL EXPOSURES Optimization of Protection And Safety “Registrants and licensees and radiological medical practitioners shall ensure that protection and safety is optimized for each medical exposure.” Nuclear Medicine Part 3. Principles of Radiation Protection 97 Quality assurance for medical exposures 3.169. Registrants and licensees, in applying the requirements of these Standards in respect of management systems, shall establish a comprehensive programme of quality assurance for medical exposures with the active participation of medical physicists, radiological medical practitioners, medical radiation technologists and, for complex nuclear medicine facilities, radiopharmacists and radiochemists, and in conjunction with other health professionals as appropriate. Principles established by the World Health Organization, the Pan American Health Organization and relevant professional bodies shall be taken into account. Nuclear Medicine Part 3. Principles of Radiation Protection 98 REQUIREMENTS FOR MEDICAL EXPOSURES Dose Constraints 3.172. “Registrants and licensees shall ensure that relevant dose constraints (para. 3.148(a)(i)) are used in the optimization of protection and safety in any procedure in which an individual acts as a carer or comforter” Nuclear Medicine Part 3. Principles of Radiation Protection 99 MANAGEMENT REQUIREMENTS Protection and safety elements of the management system Safety culture Human Nuclear Medicine Factors Part 3. Principles of Radiation Protection 100 Protection and safety elements of the management system 2.47. The principal parties shall demonstrate commitment to protection and safety at the highest levels within the organizations for which they are responsible. 2.49. The principal parties shall ensure that protection and safety elements of the management system are commensurate with the complexity of and the radiation risks associated with the activity. 2.50. The principal parties shall be able to demonstrate the effective fulfilment of the requirements for the protection and safety in the management system. Nuclear Medicine Part 3. Principles of Radiation Protection 101 Management Requirements SAFETY CULTURE 2.51. The principal parties shall promote and maintain a safety culture by: (a) Promoting individual and collective commitment to protection and safety at all levels of the organization; (b) Ensuring a common understanding of the key aspects of safety culture within the organization; (c) Providing the means by which the organization supports individuals and teams in carrying out their tasks safely and successfully, with account taken of the interactions between individuals, technology and the organization; (d) Encouraging the participation of workers and their representatives and other relevant persons in the development and implementation of policies, rules and procedures dealing with protection and safety; (e) Ensuring accountability of the organization and of individuals at all levels for protection and safety; (f) Encouraging open communication with regard to protection and safety within the organization and with relevant parties, as appropriate; (g) Encouraging a questioning and learning attitude and discouraging complacency with regard to protection and safety; (h) Providing means by which the organization continually seeks to develop and strengthen its safety culture. Nuclear Medicine Part 3. Principles of Radiation Protection 102 Management Requirements HUMAN FACTORS 2.52. The principal parties and other parties having specified responsibilities in relation to protection and safety, as appropriate, shall take into account human factors and shall support good performance and good practices to prevent human and organizational failures by: Sound ergonomic principles Appropriate equipment, safety systems and procedural requirements Nuclear Medicine Part 3. Principles of Radiation Protection 103 Safety Assessments A review of the aspects of design and operation of a source which are relevant to the protection of persons or the safety of the source, including the analysis of the provisions for safety and protection established in the design and operation of the source and the analysis of risks associated with normal conditions and accident situations. Nuclear Medicine Part 3. Principles of Radiation Protection 104 Requirement 13: Safety assessment BSS 3.31.: “Safety assessments shall be conducted at different stages, including the stages of siting, design, manufacture, construction, assembly, commissioning, operation, maintenance and decommissioning (or closure) of facilities or parts thereof, as appropriate, so as: (a) To identify the ways in which exposures could be incurred, account being taken of the effects of external events as well as of events directly involving the sources and associated equipment; (b) To determine the expected magnitudes and likelihood of exposures in normal operation and, to the extent reasonable and practicable, make an assessment of potential exposures; (c) To assess the adequacy of the provisions for protection and safety. Nuclear Medicine Part 3. Principles of Radiation Protection 105 Requirement 14: Monitoring for Verification of Compliance “Registrants and licensees and employers shall conduct monitoring to verify compliance with the requirements for protection and safety”. BSS 3.37. “The regulatory body shall establish requirements that monitoring and measurements be performed to verify compliance with the requirements for protection and safety. The regulatory body shall be responsible for the review and approval of monitoring and measurement programmes of registrants and licensees”. Nuclear Medicine Part 3. Principles of Radiation Protection 106 Records BSS 2.40, (d): “Records are maintained of the results of monitoring and verification of compliance, as required by the regulatory body, including records of the tests and calibrations carried out in accordance with these Standards.” Nuclear Medicine Part 3. Principles of Radiation Protection 107 (Nuclear) Security The prevention and detection of, and response to, theft, sabotage, unauthorized access, illegal transfer or other malicious acts involving nuclear material, other radioactive material or their associated facilities Nuclear Medicine Part 3. Principles of Radiation Protection 108 Requirement 15: Prevention and mitigation of accidents 1. 2. 3. 4. Defense in Depth Good Engineering Practice Accident prevention Emergency preparedness and response Nuclear Medicine Part 3. Principles of Radiation Protection 109 Nuclear Medicine Part 3. Principles of Radiation Protection 110 EXPOSURES Similar definitions to ICRP Nuclear Medicine Occupational Exposure Public Exposure Medical Exposure Part 3. Principles of Radiation Protection 111 Requirement 21: Responsibilities of employers, registrants and licensees for the protection of workers Employers, registrants and licensees shall be responsible for the protection of workers against occupational exposure. Employers, registrants and licensees shall ensure that protection and safety is optimized and that the dose limits for occupational exposure are not exceeded. 3.74. For workers who are engaged in activities in which they are or could be subject to occupational exposure in planned exposure situations, employers, registrants and licensees shall be responsible for: (a) Protection of workers against occupational exposure; (b) Compliance with other relevant requirements of these Standards. Nuclear Medicine Part 3. Principles of Radiation Protection 112 Occupational – Schedule III Dose Limits: An effective dose of 20mSv per year averaged over five consecutive years An effective dose of 50mSv in any single year An equivalent dose to lens of eye of 20mSv in a year averages over 5 consecutive years (100mSv in 5 years and of 50mSv in any single year An equivalent dose to extremities or skin of 500mSv in a year. For apprentices (16-18 years of age): An effective dose of 6mSv in a year An effective dose to the lens of eye of 20 mSv in a year An equivalent dose to extremities or skin of 150mSv in a year. Nuclear Medicine Part 3. Principles of Radiation Protection 113 Occupational Female workers should notify pregnancy Notification of an employer of a suspected pregnancy or of breast-feeding cannot be a requirement on a female worker in these Standards. However, it is important that all female workers understand the importance of making such notifications so that their working conditions may be modified accordingly. Working conditions shall be adapted to ensure that the embryo and fetus are afforded the same broad level of protection as for members of the public. Nuclear Medicine Part 3. Principles of Radiation Protection 114 Occupational CLASSIFICATION OF AREAS Controlled areas - 3.88. Registrants and licensees shall designate as a controlled area any area31 in which specific measures for protection and safety are or could be required for: (a) Controlling exposures or preventing the spread of contamination in normal operation; (b) Preventing or limiting the likelihood and magnitude of exposures in anticipated operational occurrences and accident conditions. Supervised areas - Registrants and licensees shall designate as a supervised area any area not already designated as a controlled area but for which occupational exposure conditions need to be kept under review, even though specific measures for protection and safety are not normally needed. Nuclear Medicine Part 3. Principles of Radiation Protection 115 Responsibilities of registrants and licensees for Medical Exposure Registrants and licensees shall ensure that no person incurs a medical exposure unless there has been an appropriate referral, responsibility has been assumed for ensuring protection and safety, and the person subject to exposure has been informed as appropriate of the expected benefits and risks. (d) For therapeutic uses of radiation, the requirements of these Standards for calibration, dosimetry and quality assurance, including the acceptance and commissioning of medical radiological equipment, as specified in paras 3.166, 3.167(c), 3.169 and 3.170, are fulfilled by or under the supervision of a medical physicist;; Nuclear Medicine Part 3. Principles of Radiation Protection 116 Medical Exposure Justification – by weighing diagnostic or therapeutic benefit against radiation detriment, taking into account available alternative techniques. Optimization – all other requirements – plus safety oriented requirements – minimum patient exposure consistent with acceptable image quality and clinical purpose Guidance levels – for diagnostic radiological procedures – for diagnostic nuclear medicine procedures Nuclear Medicine Part 3. Principles of Radiation Protection 117 Medical Exposure DOSE CONSTRAINTS DO NOT APPLY TO PATIENTS, BUT ARE APPLICABLE for individuals helping in care, support or comfort of patients, and visitors Release of patients after as per IAEA Safety Report 63 Nuclear Medicine Part 3. Principles of Radiation Protection 118 Medical Exposure DOSE CONSTRAINTS APPLICABLE for volunteers subject to exposure as part of a programme of biomedical research. Nuclear Medicine Part 3. Principles of Radiation Protection 119 Responsibilities for Public Exposure 3.125. Registrants and licensees in cooperation with suppliers and with providers of consumerproducts shall apply the requirements of these Standards and shall verify and demonstrate compliancewith them, as specified by the regulatory body, in relation to any public exposure delivered by a source for which they have responsibility. Nuclear Medicine Part 3. Principles of Radiation Protection 120 Public Exposure - Schedule III DOSE LIMITS • An effective dose of 1mSv in a year • In special circumstances, a higher value of effective dose in a single year could apply, provided that the average effective dose over five consecutive years does not exceed 1mSv per year • An equivalent dose to lens of the eye 15mSv in a year • An equivalent dose to skin of 50mSv in a year. Nuclear Medicine Part 3. Principles of Radiation Protection 121 Public Radioactive Waste (RADWASS) minimize segregate and treat control discharges. Source Monitoring, Environmental Monitoring Consumer Products Nuclear Medicine Part 3. Principles of Radiation Protection 122 Emergency Exposures emergency plans intervention level Nuclear Medicine Part 3. Principles of Radiation Protection 123 IAEA Training Material on Radiation Protection in Nuclear Medicine Part 3. Module 3.3. Regulatory Control Responsibilities of the regulatory bodies The government or regulatory body shall establish and enforce requirements for the optimization of protection and safety, and registrants and licensees shall ensure that protection and safety is optimized. The prime responsibility for safety must rest with the person or organization responsible for facilities and activities that give rise to radiation risks. Regulatory bodies have responsibility for Enforcement of regulatory requirements Nuclear Medicine Part 3. Principles of Radiation Protection 125 Responsibilities of the regulatory body The regulatory body shall establish or adopt regulations and guides for protection and safety and shall establish a system to ensure their implementation. 2.30. The regulatory body shall establish a regulatory system for protection and safety that includes [8]: (a) Notification and authorization; (b) Review and assessment of facilities and activities; (c) Inspection of facilities and activities; (d) Enforcement of regulatory requirements; (e) The regulatory functions relevant to emergency exposure situations and existing exposure situations; (f) Provision of information to, and consultation with, parties affected by its decisions and, as appropriate, the public and other interested parties. Nuclear Medicine Part 3. Principles of Radiation Protection 126 National Infrastructure (not exhaustive) LEGISLATION REGULATIONS REGULATORY BODY (INDEPENDENT) - Notification and Authorization - Inspection of facilities and activities - Enforcement of regulatory requirements GENERAL PROVISIONS / SERVICES - Environmental Monitoring - Intervention - Personal Dosimetry - Calibration - Information Exchange - Education andTraining Nuclear Medicine Part 3. Principles of Radiation Protection 127 Regulatory Authority (main characteristics and functions) ESTABLISHED BY THE GOVERNMENT Given: - Powers - Resources - Independence (effective) To: Nuclear Medicine - Receive Notifications - Carry out assessments - Issue Authorizations/Licenses - Inspect - Enforce Part 3. Principles of Radiation Protection 128 Authorization BSS 3.9: “Any person or organization applying for authorization: (a) Shall submit to the regulatory body the relevant information necessary to support the application; (b) Shall refrain from carrying out any of the actions specified in para. 3.5 until the registration or licence has been granted; (c) Shall assess the nature, likelihood and magnitude of the expected exposures due to the source and shall take all necessary measures for protection and safety; (d) Shall, if there is a possibility for an exposure to be greater than a level as specified by the regulatory body, have a safety assessment made and submitted to the regulatory body as part of the application; (e) Shall, as required by the regulatory body, have an appropriate prospective assessment made for radiological environmental impacts, commensurate with the radiation risks associated with the facility or activity”. Nuclear Medicine Part 3. Principles of Radiation Protection 129 Authorization The authorization should be renewed periodically. Periods should be based on safety criteria and established by the Regulatory Authority. The Regulatory Authority may consider suspending or revoking an authorization when the licensees are in serious breach of the requirements of the BSS or the national regulations and laws. Nuclear Medicine Part 3. Principles of Radiation Protection 130 Authorization The following activities related to Nuclear Medicine should be Authorized: • import, distribution, sale or transfer of radioactive substances •installation and maintenance of nuclear medicine equipment • disposal of radioactive waste Nuclear Medicine Part 3. Principles of Radiation Protection 131 Application for Authorization Type of Authorization • New • Amendment to existing authorization • Renewal of authorization Purpose of Application • Constructions • Import/Purchase • Use/Begin operation Nuclear Medicine Part 3. Principles of Radiation Protection 132 Application for Authorization General information: • Name and address of organization • Name and information about qualified experts - RPO - Medical Physicist • Responsible representative of the legal person • Proposed date of installation and/or commissioning of facilities and equipment Nuclear Medicine Part 3. Principles of Radiation Protection 133 Application for Authorization SOURCES: • Radionuclides involved in the work • Containment of the radionuclides • Work pattern • Work locations • Radioactive waste Nuclear Medicine Part 3. Principles of Radiation Protection 134 Application for Authorization FACILITIES AND EQUIPMENT Facility specifications Location Layout Ventilation, plumbing and surfaces Equipment specifications Imaging equipment Activity meter Safety equipment Monitoring equipment Nuclear Medicine Part 3. Principles of Radiation Protection 135 Application for Authorization RADIATION PROTECTION PROGRAMME Organizational structure Area classification Individual and workplace monitoring Local rules and supervision Quality assurance Transportation of radioactive material Emergency procedures Radioactive waste Records Nuclear Medicine Part 3. Principles of Radiation Protection 136 Application for Authorization MEDICAL EXPOSURE • Responsibilities • Justification • Optimization • Calibration • Clinical dosimetry • Quality assurance • Dose constraints • Investigation of accidental medical exposures • Guidance levels Nuclear Medicine Part 3. Principles of Radiation Protection 137 Inspections An inspection to assess the status of compliance with regulatory requirements and safety of an authorized operation should be based on direct observation of work activities, interviews with workers, independent measurements of radiation and contamination levels, and review of records. The review and inspection processes should be closely coupled, with reviewers of the application and inspectors and inspectors exchanging experiences. Nuclear Medicine Part 3. Principles of Radiation Protection 138 Inspections Adequate preparation before the inspection is essential. The inspector should review the documents submitted with the application, and the history of the facility. Appropriate monitoring instruments to measure radiation and contamination levels should be obtained as necessary. An inspection plan as a guide for inspection of the organization's safety programme should be prepared. The plan should prioritize inspection of potential problem areas in the facility. Nuclear Medicine Part 3. Principles of Radiation Protection 139 Inspections Unannounced inspections The advantage of an unannounced inspection is that it provides the opportunity to see the facility operating under its usual conditions. The disadvantages are that the key personnel may not be available, or part of the facility may not be operating. Nuclear Medicine Part 3. Principles of Radiation Protection 140 Inspections The facility and operating programmes should be inspected in detail to determine whether they conform to those described in the application. The inspector should verify that the staff present are as described in the application. The inspector should carefully review records. The inspector should interview key members of the staff to elicit information which helps the inspector assess the status of protection and safety Nuclear Medicine Part 3. Principles of Radiation Protection 141 Inspections The frequency of routine inspections for each facility should be planned according to the hazards and risks associated with the operation of that facility and its previous compliance history. Nuclear Medicine Part 3. Principles of Radiation Protection 142 Frequency of Regular Inspections Category A High safety risk; every 1 – 3 years Category B Medium safety risk; every 3 – 5 years Category C Low safety risk; every 5 – 10 years Nuclear Medicine Part 3. Principles of Radiation Protection 143 Inspections 1. 2. 3. 4. 5. 6. 7. Nuclear Medicine Identifying information Verification of safety Verification of worker protection Verification of public protection Emergency preparedness Medical exposure Records Part 3. Principles of Radiation Protection 144 Inspections Verification of safety: • • • • • • • • Nuclear Medicine Description of radioactive material in use Description of measuring and handling equipment Facility design Safety control and equipment design Warning systems Safety operation-management Safety operation-technical Investigation and quality assurance Part 3. Principles of Radiation Protection 145 Inspections Verification of Occupational Protection • • • Nuclear Medicine Classification of areas Local rules and supervision Monitoring Part 3. Principles of Radiation Protection 146 Inspections Medical exposure: • Responsibilities • Justification • Optimization • Calibration • Clinical dosimetry • Quality assurance • Dose constraints • Investigation of accidental medical exposures • Guidance level Nuclear Medicine Part 3. Principles of Radiation Protection 147 Enforcement Enforcement is Action taken by the Regulatory Authority to ensure that the responsible party corrects non-compliance with regulatory requirements Nuclear Medicine Part 3. Principles of Radiation Protection 148 Graded Enforcement Actions Based on threat to health and safety Operations likely not safe Potential threat of health and safety No immediate threat to health and safety (usually regulatory infraction) Nuclear Medicine Part 3. Principles of Radiation Protection 149 Graded Enforcement Actions No immediate threat to health and safety (usually regulatory infraction) Informal or formal instructions to correct the infraction Operations may continue while corrective measures are taken Informal oral instruction should be followed in writing Examples might be a non-complying or deteriorated warning sign for a controlled area, or the calibration of an instrument not having been carried out by the due date. Nuclear Medicine Part 3. Principles of Radiation Protection 150 Graded Enforcement Actions Potential threat of health and safety Suspension of or restrictions on operations until regulatory infraction or safety condition is corrected An example might be a requirement to replace badly cracked and poor quality flooring material in a ward room used for thyroid cancer patients treated with I-131. Nuclear Medicine Part 3. Principles of Radiation Protection 151 Graded Enforcement Actions Operations likely not safe Licensee shows a record of poor performance or adverse safety conditions Suspension of or restrictions on operations An example might be the unauthorised use of lung ventilation studies in a room without appropriate air pressure controls used also for ultrasound scans of pregnant women. Nuclear Medicine Part 3. Principles of Radiation Protection 152 Questions? Nuclear Medicine Part 3. Principles of Radiation Protection 153 Discussion Give examples of non-justified situations in: • The practice of nuclear medicine • Examination or treatment of a single patient Nuclear Medicine Part 3. Principles of Radiation Protection 154 Discussion A nuclear medicine department which has treated hyperthyroid patients on an outpatient basis for some time proposes to extend its services to include treatment of thyroid cancer patients. A two room area is to be designated for therapy in-patients. What information should be submitted to the Regulatory Authority to allow this extension of the work of the department to be authorised? Nuclear Medicine Part 3. Principles of Radiation Protection 155 Discussion A nuclear medicine department in a hospital had taken delivery of a single dose vial of I-131 for treatment of a thyroid cancer patient. A different hospital had ordered a different activity amount of I131 from the same supplier (external to the country). The wrong vial was delivered by courier to the first hospital and the dose was administered to the patient. The error was discovered when checks at the second hospital showed the incorrect activity in the vial received by them. Appropriate investigation and enforcement action? Nuclear Medicine Part 3. Principles of Radiation Protection 156 Where to Get More Information? Further Readings: IAEA Basic Safety Standards, Interim Edition (2011) ICRP publication 103, 2007 RPOP website: www.rpop.iaea.org WHO/IAEA. Manual on Radiation Protection in Hospital and General Practices. Volume 1, Basic Requirements IAEA. Practice-specific Model Regulations on Radiation Safety in Nuclear Medicine Nuclear Medicine Part 3. Principles of Radiation Protection 157