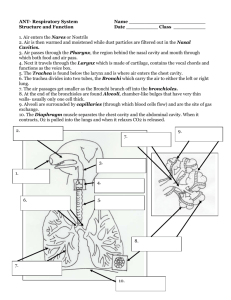
Respiratory System
advertisement

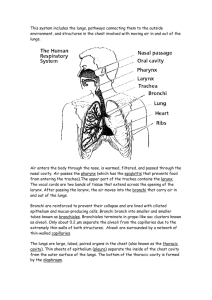
Biology 322 – Human Anatomy Respiratory system Respiratory system function and anatomy •In biology, RESPIRATION can have several meanings: 1. Movement of air in/out of the lungs (really known as ventilation) 2. Exchange of O2 for CO2 in the bloodstream 3. Use of O2 during aerobic respiration (ATP generation) •Main function of respiration is to replenish O2 and expel CO2 •Need O2 for aerobic respiration •Need to eliminate CO2 waste •CO2 + H2O → H2CO3 → HCO3- + H+→ acid build up in blood and tissues •Additional, important functions: •Need to move air for vocalization (speech, laugh, cry, etc…), sense of smell •Respiratory pump aids blood flow back to heart •Breath holding – allows us to survive underwater briefly, aids in urination, defacation, childbirth Respiratory system anatomy 1. Nose 2. Pharynx • nasopharynx, oropharynx, laryngopharynx 3. Larynx 4. Trachea 5. Bronchi – airways within the lung 6. Lungs • Most distal portions end in sacs called ALVEOLI How we get O2 from atmosphere to blood Essentially a “dead end” circuit – air enters resp. system, travels to distal parts of lung, then goes back the way it came in •Two main functional divisions exist: 1. Conducting division – Organs which allow air to get to lungs, but do not exchange O2 and CO2 Nose, pharynx, larynx, trachea, most bronchi 2. Respiratory division – Portion of resp. system that carries out gas exchange Some smaller distal bronchi and alveoli Conducting Division •Main function is to move air from outside → inside → back outside •Several organs also play other roles and contribute to normal function of respiratory system •Nasal cavity – Conditions the air as it enters the body Nasal conchae cause air to swirl as it enters Nasal cavity lined by MUCOSAL MEMBRANE •GOBLET CELLS that secrete mucous, pseudostratified ciliated cells that “sweep” material back so that it can be swallowed Air is warmed and humidified •ERECTILE TISSUE in inferior conchae fills with warm blood (common site of nosebleed) Dust, allergens, other particles get trapped in nasal hairs VIBRISSAE and in mucous that lines the nasal cavity OLFACTORY MUCOSA – patch of cells located mostly in superior portion of nasal cavity •Contains nerve fibers (C.N. I) that pass through cribiform plate •Pharynx – divided anatomically into 3 regions 1. Nasopharynx – posterior to the nasal cavity, slightly superior to oral cavity Air enters through nose and is directed inferiorly Lined by mucus membrane Lymphoid tissues (tonsils) are well positioned to combat this Eustachian tube (auditory tube) opens here 2. Oropharynx – posterior to the oral cavity, inferior to the soft palate (roof of mouth) Also well supplied with lymphoid tissues 3. Laryngopharynx – inferior to oropharynx Lined by pseudostratified columnar epithelia (like much of the conducting airway) Laryngopharynx and oropharynx transmit BOTH food/liquid and air •Lined by non-keratinized, stratified squamous epithelia Nasopharynx ONLY transmits air EPIGLOTTIS covers opening to laryngopharynx – prevents choking! Larynx – a.k.a. the “voicebox” •Obviously hugely important for its social and psychological function •Also very important for keeping food, fluids out of the airways Epiglottis – larynx is PULLED upwards when we swallow and closes opening of larynx Vestibular folds – also close shut when we swallow •Very well protected by a number of thick cartilage structures Thyroid cartilage – forms “Adam’s Apple” Cricoid cartilage – connects larynx to trachea below Many smaller cartilages that are important for vocal portion of larynx •Several INTRINSIC muscles and ligaments allow opening/closing of glottis (opening of larynx) as well as movement of vocal cords •Vestibular fold controls opening of glottis – prevents choking •Vocal fold - fold of tissue overlying the vocal ligaments Inferior to vestibular fold Vibrate as air moves over them Varying tension on vocal cords allow us to create various “rough” sounds Trachea – rigid tube found ANTERIOR to the esophagus, continuous with inferior part of larynx •C-shaped rings of hyaline cartilage offer structural support Rings get smaller, thinner as you go deeper into the lung tissue (more distal) •Interior lined by pseudostratified columnar epithelium and many GOBLET CELLS (mucus cells) Particles get trapped in mucus and cilia on columnar cells sweep upwards Dirty mucus gets moved towards esophagus where it can be swallowed Referred to as the MUCOCILIARY ELEVATOR Bronchial Tree •Trachea branches at a point known as the CARINA to form a right and left PRIMARY BRONCHUS •After 2-3 cm the primary bronchi enter the lung tissue and branch into successively smaller SECONDARY and TERTIARY bronchi •Distal to the bronchi are the BRONCHIOLES •Each bronchiole branches into TERMINAL BRONCHIOLES – the end of the conducting system This is where gas exchange actually occurs •Terminal bronchioles branch into RESPIRATORY BRONCHIOLES that have small ALVEOLAR DUCTS branching off •The ends of the alveolar ducts have small, thin sacs known as ALVEOLI budding from them Air Flow Mostly pseudostratified columnar, goblet cells Often cuboidal, with or without cilia Simple squamous cells 1. 2. 3. 4. 5. 6. 7. 8. 9. Trachea Primary bronchi Secondary bronchi Tertiary bronchi Bronchioles Terminal bronchioles Respiratory bronchioles Alveolar ducts Alveoli Supported by cartilage No cartilage Lung structure •Inferior is BASE, superior is APEX •Surfaces : Costal surface – anterior, lateral, posterior (faces the rib cage) Mediastinal surface – medial surface Diaphragmatic surface – portion of the base that rests on the diaphragm •There is a large impression on the left lung where the heart projects laterally – CARDIAC IMPRESSION •Right lung has 3 lobes – superior, middle, inferior •Left lung has 2 lobes – superior and inferior Lobes are separated by fissures: •Oblique fissure in left lung •One oblique and one horizontal fissure in right lung Pleura •Like the heart, the lungs reside in the thoracic cavity and are surrounded by two layers of serous membranes VISCERAL PLEURA – lies directly on top of the lung PARIETAL PLEURA – lines part of the thoracic cavity, mediastinum, and diaphragm •The PLEURAL CAVITY is space between the pleurae filled with PLEURAL FLUID that has three functions 1. Reduces friction during ventilation 2. Creates pressure gradient 3. Compartmentalization of organs Pulmonary Blood Supply •Pulmonary arteries and veins enter the heart near where the primary bronchi enter – HILUM •Pulmonary vessels follow roughly the same path and branching pattern as the bronchial tree •The more distal parts of the lung (respiratory bronchioles, alveolar ducts, alveoli) receive O2 and nutrients directly from the pulmonary circulation •The more proximal parts (primary bronchi, secondary bronchi, pleura, etc…) need their own supply BRONCHIAL ARTERIES branch off of the descending aorta BRONCHIAL VEINS drain blood that eventually reaches the superior vena cava However, some venous blood from the bronchial veins ends up in the pulmonary veins…. Alveolar Structure •Most gas exchange occurs near the terminal ends of the bronchial tree in closed sacs called ALVEOLI •Average human lung has about 150 MILLION alveoli with a huge surface area of well over 200 ft2 •Most cells are simple squamous epithelial cells •Each alveolus is surrounded by a capillary bed Simple squamous cell of alveolus + endothelial cell/basement membrane of capillary = RESPIRATORY MEMBRANE Creates a gas exchange barrier of only 0.5 microns!! Gases are easily exchanged Type 1 alveolar cell Alveolar Structure, cont… •Alveoli are composed of two unique cell types: Type 2 alveolar cell Alveolar macrophage 1. Type 1 alveolar epithelial cells – simple squamous cells • Most numerous • Well suited for gas exchange 2. Type 2 alveolar epithelial cells – more cuboid in shape • Much less prevalent • Main job is to produce PULMONARY SURFACTANT Alveoli also contain many MILLIONS of ALVEOLAR MACROPHAGES •Monitor the alveolus for bacteria, debris that didn’t get filtered out •After phagocytosis, macrophages make their way up the mucociliary elevator Alveolar Structure •Interior surface of alveolus is lined by a thin layer of fluid called the HYPOPHASE •Polar nature of H2O causes surfaces of alveoli to cling together •Type 2 cells produce a thin layer of PULMONARY SURFACTANT that reduces surface tension Prevents alveoli from collapsing when we exhale!! Pulmonary surfactant – •Complex mix of phospholipids and 4 proteins secreted by TYPE 2 ALVEOLAR CELLS •Plays two roles : 1. Reduces alveolar surface tension 2. Assists alveolar macrophages in digestion of bacteria/viruses Alveolar gas exchange •In order to exchange O2 and CO2, the gasses must cross the respiratory membrane and the hypophase •This occurs via diffusion •O2 and CO2 that are being exchanged are first dissolved in the water part of the hypophase AIR (alveolus) WATER (hypophase) CO2 O2 RESPIRATORY MEMBRANE BLOOD Pulmonary Ventilation Movement of air into and out of the lungs •RESPIRATORY CYCLE is the repetitive cycle of inhalation (air in) and exhalation (air out) •Movement of air between two spaces requires a pressure gradient Air moves from an area of high pressure → low pressure Important to remember that an increase in volume → decrease in pressure As pressure within the alveoli decreases air rushes in from the atmosphere Respiratory muscles •Main muscle responsible for ventilation is the DIAPHRAGM Contraction increases volume of cavity (and decreases pressure) •Intercostal muscles of ribs are also important External intercostals assist inhalation Internal intercostals assist in FORCED exhalation Visceral Pleura Parietal Pleura •Organization of the pleurae is critical to ventilation •Visceral pleura – attached to lung •Parietal pleura – attached to thoracic wall •Pleural cavity – fluid filled space between Normally a slight vacuum exists in this space (~4mm Hg) •Vacuum within pleural cavity and fluid on surfaces of membranes cause the two layer to “stick” together •As the thoracic cavity enlarges the parietal pleura moves and draw the visceral pleura with it. •Lung puncture (PNEUMOTHORAX) breaks this vacuum and prevents that lung from expanding Pleural Cavity Mechanics of Inhalation •Air movement is driven by pressure gradients •At rest, there is no pressure gradient between atmosphere and alveoli – called TRANSPULMONARY PRESSURE •INTRAPLEURAL PRESSURE – Pressure within the two pleural membranes, normally a -4 mm Hg vacuum This vacuum causes pleural membranes to stick together and move at the same time Creates a mechanical coupling of thoracic cavity volume to lung volume •INTRAPULMONARY PRESSURE – Pressure within the alveoli themselves As volume of alveoli increases, pressure drops below that of atmosphere→ air flows INTO the lung •Eventually, intrapulmonary pressure EQUALS atmospheric pressure and flow stops •Since inhalation requires muscle contraction, it is considered to be an active process “Balloon and Pipe Model of Respiration” AIR •In VERY simple terms the bronchial tree and alveoli can be thought of as a pipe (conducting airways) and a balloon (alveoli) Expansion of thoracic cavity Decrease in intrapleural pressure P P Decrease in intrapulmonary pressure Air rushes into lung Mechanics of Exhalation •As opposed to inhalation, exhalation is normally a passive process However, we can force exhalation (blowing up a balloon or blowing out candles) •Exhalation is primarily caused by three factors: 1. Recoil of thoracic cavity Decreases volume of thoracic cavity/lung 2. Relaxation of diaphragm 3. Recoil of elastic fibers that surround the alveoli • Decrease in volume of thoracic cavity/alveoli → increase in intrapulmonary pressure As intrapulmonary pressure exceeds atmospheric pressure, air is forced out of the lung • Rate of exhalation is slowed by CONTROLLED relaxation of diaphragm Allows respiratory cycle to occur smoothly Phrenic nerve continues to stimulate diaphragm slightly • Forced exhalation results from contraction of abdominal muscles (pull downward on rib cage) and internal intercostals (contract ribs) Forced exhalation DOES have its limits…….. Exhalation Contraction of thoracic cavity (Could be passive or forced) AIR Increase in intrapleural pressure Increase in intrapulmonary pressure P Air rushes out of lung P Inhalation/Exhalation Rate of expiration Limits to expiratory rate “Balloon and squishy pipe model” Force Increased AIRWAY RESISTANCE limits rate of forced expiration 1. Cartilage decreases moving from 1° bronchi, 2° bronchi, etc… 2. Increases in thoracic pressure can deform some airways (point of diminishing return) 3. Bernoulli’s principle – the faster air flows, the less pressure it exerts • Airways partially collapse when air flows rapidly out of the lung Airflow resistance •Air flowing through lungs encounters resistance like blood flowing through arteries and veins •Resistance decreases airflow in/out of the lung •Resistance is influenced by factors: 1. Bronchiole diameter – • ↓ airway diameter leads to ↑resistance to airflow, and vice versa • Resistance decreases airflow in/out of lung • Increase/decrease in airway diameter is known as BRONCHODILATION or BRONCHOCONSTRICTION • Mainly occurs in distal portions of lung – trachea, larger bronchi don’t really change diameter that much (lots of supporting cartilage) •Diameter is affected by contraction/relaxation of smooth muscle surrounding airway as well as the lining of the airway (inflammation of membranes) •Sympathetic stimulation (epinephrine, norepinephrine) cause bronchodilation •Parasympathetic stimulation causes bronchoconstriction Resistance to airflow….. 2. Pulmonary compliance – ability of the lungs to expand and contract • Alveoli are surrounded by elastic fibers • Damage to fibers can limit lung compliance Alveoli can expand but don’t want to contract • Accumulation of scar tissue can cause lungs to become stiff (no expansion) Emphysema is a disease of decreased lung compliance •Exposure to toxic chemicals, smoke trigger formation of scar tissue and degradation of elastic fibers Resistance to airflow….. 3. Alveolar surface tension – • Presence of hypophase within alveoli and distal bronchioles increases surface tension - walls want to stick together • Pulmonary surfactant reduces surface tension – prevents airway and alveolar collapse • Lack of surfactant in preterm infants causes respiratory distress syndrome •Water molecules on opposing surfaces want to form hydrogen bonds with themselves •Surfactant prevents formation of these bonds Alveolar Ventilation Describes the air that actually enters/exits the alveoli •During normal breathing we inhale about 500 mL of air (TIDAL VOLUME) •Some of this air only gets as far as the conducting airways (trachea, bronchi) and not involved in gas exchange •ANATOMICAL DEADSPACE – portion of lung where air is present but not involved in gas exchange •PHYSIOLOGICAL DEADSPACE – anatomical deadspace plus non-functional alveoli Increases with diseases like emphysema Alveolar ventilation, cont…. •Normal tidal volume is 500 mL, but about 150 mL is deadspace ventilation About 350 mL of air reaches the alveoli (ALVEOLAR VENTILATION) •Alveolar ventilation rate = alveolar ventilation (mL/breath) X breaths per minute •Ex.: 350 mL/ breath X 12 breaths/min. = 4,200 mL/min •Not all air in lungs is expelled each breath, so goal of A.V. is to “refresh” the air in the lungs at any given time rather than completely replace it Spirometry - Assessment of pulmonary/respiratory function Spirometry - Assessment of pulmonary/respiratory function Some common respiratory capacities: usually the sum of two or more respiratory volumes