Permanent Impairment Awards - Getman, Schulthess & Steere
advertisement

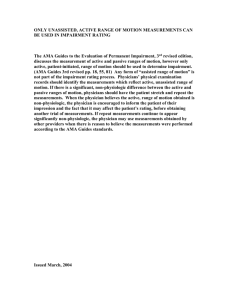
Permanent Impairment Awards: From MMI through Calculation & Approval Presented by: Getman, Schulthess & Steere, PA Three Executive Park Drive Ste 9 Bedford, NH 03110 603-634-4300 and Jo-Ann Dixon Permanent Impairment Coordinator New Hampshire Department of Labor 281-A:32 Scheduled Permanent Impairment Award I. Basic Award. Except when death results from injury, in addition to other benefits payable under this chapter, an award shall be paid to employees in amounts provided by RSA 281-A:28 for the number of weeks set forth in this section for permanent bodily loss or losses: (a) (b) (c) (d) (e) (f) (g) (h) (i) (j) (k) (l) (m) (n) (o) Total loss of arm 210 Total loss of hand 189 Total loss of thumb 76 Total loss of index finger 47 Total loss of middle finger 38 Total loss of ring finger 19 Total loss of little finger 9 Total loss of leg 140 Total loss of foot 98 Total loss of great toe 18 Total loss of toe, other 3 Total loss of vision--one eye 84 Total loss of vision--both eyes 300 Total loss of hearing in one ear 30 Total loss of binaural hearing 123 phalanx /pha·lanx/ (fa´langks) pl. halan´ges [Gr.] 1. any bone of a finger or toe. Each finger has three phalanges (the distal, middle, and proximal); the thumb only has Two metacarpal bones – Phalanges II. A loss in excess of the distal phalanx shall entitle the employee to the award for the loss of the entire digit. A loss of a distal phalanx shall result in half the award for the loss of the entire digit. A loss of less than one phalanx shall result in one quarter of the award for the loss of the entire digit. Calculation for a finger amputation (RSA-32 II) • Less than whole distal phalanx = 25% digit impairment • Whole distal phalanx loss = 50% digit impairment • Excess of distal phalanx = 100% digit impairment Two or More Digits IV. The loss of 2 or more digits, or the loss of one or more phalanges of such number of digits, of a hand or foot, shall entitle the employee to an award proportioned to the loss of use of the hand or foot occasioned by that loss; except that the income benefits for the loss of a hand or foot may not be exceeded. (189 Hand 98 Foot) Amputated Arm or Leg III. The amputation of an arm or leg at or above the elbow or at or above the knee, respectively, shall entitle the employee to the award for the loss of the arm or leg. Otherwise, amputation of an arm or leg shall result in the award for the loss of a hand or foot. Total Loss of Use VI. An award for the permanent total loss of the use of a member shall be identical to that for the loss of the member, except that amputation of such member resulting from the original or subsequent injury shall not entitle the employee to a further award under this section. Partial Loss of Use VII. An award for the permanent partial loss of the use of a member. Such award shall be in the proportion that such partial loss bears to a total loss. If subsequent amputation of such member occurs an additional award shall accrue on the basis of the difference between the award for the newly established loss and the award for the original loss. Subsequent Amputation VIII. Upon amputation which has been preceded by the loss of a component or part of such member, an additional award shall accrue on the basis of the difference between the award for the newly established loss and the award for the original loss. 281-A:32 Scheduled Permanent Impairment Award - Multiple Losses Spinal Injury, Brain and Burns IX. If an injury results in more than one permanent bodily loss specified in paragraphs I-VIII, If the injury is to the spinal column or the spinal cord, or to the brain, or involves scarring, disfigurement, or other skin impairment resulting from a burn or burns------Award shall be made on the basis of a maximum of 350 weeks weeks to be determined in proportion to the maximum in accordance with the percent of the whole person specified for such bodily losses in the 5th edition of Guides to the Evaluation of Permanent Impairment'' • (P.) Spinal column/cord, Burn scarring/disfigurement or Brain injury – AMA Guide Whole person, capped at 350 weeks. • (Q.) More Tan One Permanent Loss – specified in paragraphs I-VIII --- Whole Person, combined Values Chart, capped at 350 weeks*** *** No spinal soft tissue injury or Combined Values Impairment for Spinal injury unless spinal injury results in the loss of use of an upper or lower extremity Appeal of Hiscoe (2001) II. Permanent Impairment The board also concluded that the petitioner was not entitled to a permanent impairment award because her injury was a soft-tissue injury and therefore not a compensable permanent impairment. See RSA 281-A:32, IX; In re Petition of Abbott, 139 N.H. 412, 415 (1995). 281-A:32 Scheduled Permanent Impairment Award Payment of the scheduled award becomes due upon prompt Medical disclosure, after maximum medical improvement Has been achieved,of the scheduled award Due. Payment XI. Payment becomes due upon prompt medical disclosure, after maximum medical improvement has been achieved, regarding the loss or loss of the use of the member of For the purposes of determining disability rates, the average weekly the body. For the purposes of determining disability wage used shall the be the average weekly wage of theused employee at the rates, average weekly wage shall be the time of the injury weekly wage of the employee at the time of the average injury. No later than 15 days following such disclosure the employer, or the employer's insurance carrier shall notify the commissioner as to whether it objects to the extent of the loss claimed by the employee, in which later than 15 days following disclosure employer, or the case No it shall have 30 days to such arrange for athemedical employer'spursuant insurance carrier shall281-A:38, notify the commissioner as to whether examination, to RSA and request a it objects the extent of the by lossthe claimed by the employee, in which case hearing and to determination commissioner. it shall have 30 days to arrange for a medical examination, pursuant to Payment of the scheduled award shall be made in a RSA 281-A:38, and request a hearing single payment. 281-A:32 Scheduled Permanent Impairment Award XIV. Rulemaking Required. In order to reduce litigation and establish more certainty and uniformity in the rating of permanent impairment, the commissioner shall adopt rules, under RSA 541-A, incorporating by reference the 5th edition of the American Medical Association's “Guides to the Evaluation of Permanent Impairment” to determine the degree of permanent impairment and on which to base awards under this chapter. Effective Date = June 26, 2008 6th Edition from 1/108 to 6/26/08 Lab 506.02 i) Carriers, self-insured, employers or third party administrators shall pay a permanent impairment award for the, loss of specified members or parts of the body 'or for loss of the use thereof under RSA 281-A:32, (j) In order to determine if a permanent impairment award is owed, the carrier shall: (1) Contact the injured employee or the employees’ treating physician to advise them of the need of a permanent impairment evaluation which shall: Lab 506.02 Continued… a. Be based on the most recent edition of the Guides to the Evaluation of Permanent Impairment, published by he American Medical Association; b. Contain affirmation from the submitting physician that the findings for permanent bodily loss were determined from the Guides. c. Contain medical evidence that the injured worker has reached maximum medical improvement; Lab 506.02 Continued… (2) Advise the injured worker that if the treating physician does not perform permanent impairment evaluations, the physician may refer the employee to a physician that does perform permanent impairment evaluations; (3) Pay the cost of the initial permanent impairment evaluation by the treating or referring physician; (4) Submit "Memo of Permanent Impairment Award" form 10WCA together with the medical reports that support the impairment rating within 15 days of receipt of the physicians report if no objection is filed; Lab 506.02 Continued… (5) Pay the permanent impairment award within 5 days of receipt of the approved "Memo of Permanent Impairment Award" form 10WCA; (6) Pay the permanent impairment award based on the physicians report that used the American Medical Association Guides published by the American Medical Association except where RSA 281-A:32 II is more favorable to the injured worker; (7) Pay the award in a single payment based on the average weekly wage of the employee at the time of the injury; AMA Guides 2.6 Preparing Reports A clear, accurate and complete report is essential to support a rating of permanent impairment. The following elements in bold type should be included in all impairment evaluation reports. Other elements listed in italics are commonly found within an IME or may be requested for inclusion in an impairment evaluation. 2.6a Clinical Evaluation 2.6a.2 Include a work history with a detailed, chronological description of work activities. 2.6a.3 Assess current clinical status, including current symptoms, review of symptoms, physical examination. • 2.6a.4 List diagnostic study results and outstanding pertinent diagnostic studies. • 2.6a.5 Discuss the medical basis for determining whether the person is at MMI. 2.6a.6 Discuss diagnoses, impairments. 2.6.a.7 Discuss causation and apportionment, if requested, according to recommendations outlined in Chapters 1 and 2. 2.6.a.8 Discuss impairment rating criteria, prognosis, residual function and limitations. 2.6.a.9 Explain any conclusion about the need for restrictions or accommodations. 2.5c Consistency Consistency to ensure reproducibility and greater accuracy. These measurements…. lumbosacral spine range of motion are good but imperfect indicators of people's efforts. If, in spite of an observation or test result, the medical evidence appears insufficient to verify that an impairment of a certain magnitude exists, the physician may modify the impairment rating accordingly and then describe and explain the reason for the modification in writing. AMA Guides 1.6 Causation, Apportionment Analysis and Aggravation Medical or scientifically based causation requires a detailed analysis of whether the factor could have caused the condition, based upon scientific evidence and, specifically, experienced judgment as to whether the alleged factor in the existing environment did cause the permanent impairment, Determining medical causation requires a synthesis of medical judgment with scientific analysis. AMA Guides1.6b Apportionment Analysis Apportionment analysis in represents a distribution or allocation of causation among multiple factors that caused or significantly contributed to the injury or disease and resulting impairment. The factor could be a preexisting injury, illness, or impairment. The physician may be asked to apportion or distribute a permanent impairment rating between the impact of the current injury and the prior impairment rating. Before determining apportionment, the physician needs to verify that all the following information is true for an individual: 1. There is documentation of a prior factor. 2. The current permanent impairment is greater, 3. There is evidence indicating the prior factor caused or contributed to the impairment, based on a reasonable probability (> 50% likelihood). Appeal of Fournier (2001) The Guides …require such a procedure if "apportionment" of an impairment is necessary. "Apportionment" is a term of art in the Guides which is defined as "an estimate of the degree to which each of various occupational or nonoccupational factors may have caused or contributed to a particular impairment." Id. at 315. Thus, apportionment would be appropriate if, for instance, the petitioner had had a previous carpal tunnel injury caused by something other than her work for the employer. AMA Guides 2.5h Changes in Impairment from Prior Ratings Although a previous evaluator may have considered a medical impairment to be permanent, changes may occur: the condition may have become worse as a result of aggravation or clinical progression, or it may have improved. Note-which guides to use? Appeal of Louis Cote (2001) The petitioner first asserts that the board erred in rejecting Dr. Myers‘ permanent impairment evaluation because Dr. Myers is the only doctor who conducted the specific permanent impairment assessment physical examination required by the Guide. Pursuant to section 3.3 of the Guide, each permanent impairment evaluation "should include a complete, accurate medical history and a review of all pertinent records, [and] a careful and thorough physical examination. “ Appeal of Rainville (1999) The employer contends that the board correctly rejected Dr. Nagel's evaluation because he failed to follow the AMA Guides as required by RSA 281-A:32, IX. During the hearing before the board, Dr. Nagel admitted that the AMA Guides does not refer to myofascial pain and that the petitioner did not have any of the listed physical conditions. Dr. Nagel testified that the AMA Guides "has a couple of sections that allow you to go outside ... of [its] basic techniques of range of motion [to assess impairment]." Appeal of Rainville (1999) The AMA Guides expressly allows a physician to deviate from the guidelines if the physician finds it necessary to produce an impairment rating more accurate than the recommended formula can achieve. Appeal of Rainville (1999) The decision however, must be grounded in adequate clinical information about the patient's medical condition. Additionally, in order to allow a third party to compare reports properly, physicians must utilize a standard protocol in evaluating and reporting impairment. "A clear, accurate, and complete report is essential to support a rating of permanent impairment." Appeal of Rainville (1999) Whether the statutory requirements of RSA 281-A:32, IX have been satisfied is a legal question we review de novo. See Petition of Blackford, 138 N.H. 132,13435,635 A.2d 501, 502-03 (1993). RSA 281-A:32, IX mandates that the AMA Guides be used to calculate the percent of the whole person impaired as a result of multiple permanent bodily losses. It is the statute that governs whether a permanent impairment exists; the AMA Guides applies only to the determination of appropriate compensation for a permanent impairment. We therefore examine the AMA Guides to evaluate the legal sufficiency of Dr. Nagel's assessment. Appeal of Fournier (2001) We disagree with the employer's characterization of the Guides as "evidence," and conclude that the CAB could have properly considered the Guides because their use is required by administrative rule, as authorized by statute. See N.H. Admin. Rules, Lab 508.01(d); RSA 281-A:32, XIV (Supp. 2000). We therefore examine the Guides to evaluate the legal sufficiency of a doctor's permanent impairment assessment. See Appeal of Rainville, 143 N.H. 624, 631 (1999). Petition of Gilpatric (1994) We hold that Dr. O'Neil's diagnosis and evaluation constitute competent medical testimony that supports the hearings officer's decision. Gilpatric's treating physician, Dr. Noboru Murakami, examined her and submitted reports to the department. Dr. O'Neil's calculation of eight percent permanent impairment, following the "Guides to the Evaluation of Permanent Impairment" published by the American Medical Association, is also found to be reliable. See RSA 281-A:32, XIV (Supp. 1993); N.H. ADMIN. RULES, Lab 514.03. Petition of Markievitz (1992) The triggering of a claimant's entitlement to a scheduled award may occur either at the time of the injury or when sound medical opinion has determined that "further medical treatment will be of no avail and that the loss is permanent." In this case, although the petitioner was injured on May 4, 1988, the permanency of his injury was not determined until September 6, 1990. Therefore, prior to September 6, 1990, the petitioner had no right to "claim" a permanent partial impairment award based on injury to the spinal column, and his employer had no obligation to provide such compensation. Appeal of Cote (2001) The respondent contends that the relevant date for the applicable compensation rate is the date of maximum medical improvement. While our case law regarding permanent impairment has focused upon the date maximum medical improvement is established as being the relevant date for the accrual of benefits, see, e.g., Ranger v. N.H. Youth Dev. Center, 117 N.H. 648,651 (1977); Petition of Markievitz, 135 N.H. 455, 457 (1992), the instant case is distinguishable. Here, the legislature has explicitly provided that the decreased compensation rate applies only to injuries that occurred on or after February 8, 1994. 60% Rule at Issue Appeal of Lorette (2006) In the 2003 amendment to RSA 281-A:32, XI, the legislature provided that for purposes of calculating the permanent impairment award, "the average weekly wage of the employee at the time of the injury" shall be used. RSA 281-A:32, XI. However, this amendment did not change the date upon which the employee's right to the award accrues; this date remains the date of the permanent impairment assessment. RSA 281-A:32, X; Appeal of Cote, 144 N.H. at 129; Petition of L’Heureux, 132 N.H. at 500-01; Petition of Dependents of Doran, 123 N.H. at 433. Interest on Permanency Award • RSA 281-A:44 – IV. Interest on awards for a scheduled permanent impairment shall be computed from the date when payment is due under RSA 281-A:32,XI. • RSA 281-A:32 – XI. Payment Due. Payment of the scheduled award becomes due upon prompt medical disclosure, after maximum medical improvement has been achieved, regarding the loss or loss of the use of the member of the body. (a) The carrier shall supply on Form J QWCA the following information: • (1) Name of the employee; • (2) Name and federal identification number of the employer; • (3) Name and address of the insurance carrier; • (4) Adjusting office number assigned to the carrier by the labor department; • (5) Date of injury; • (6) The name and address of the employer; • (7) The average weekly wage at the time of the injury; • (8) The percentage and the body part which is permanently impaired; • (9) The temporary total compensation rate to which the clairi1ant is entitled; • (10) The number of weeks of compensation to which the claimant is entitled as a result of this award; • (11) The date that the carrier started paying this award; • (12) The average weekly wage at the time the permanency was first evaluated; • (13) The date the form was completed; • (14) Signature of person completing this form; and • (15) Title of the person completing this form. Calculating a Permanent Impairment Award The % of impairment multiplied by the RSA-32 schedule amount of weeks for body part times the compensation rate established at time of injury. We do look up all MOP's and Wages. If they are not on file, I will call and request them. If state forms are not on file, or filed incorrectly and not amended, a request to recoup overpayment of a Permanency Award will be denied. All requests to recoup an overpay must be put in writing and submitted with the award and must explain how the overpay occurred. If I cannot substantiate the requested amount I will call for further documentation. An overpayment cannot be deducted from a Permanency Award until this department gives approval. THIS IS VERY IMPORTANT If you do not object in writing to a treating physician's rating, you will owe the claimant his treating physicians percentage rating. If you choose to negotiate any kind of settlement between parties, an objection still needs to be filed within the 15 days of receipt of the treating physicians rating. If you fail to put an objection in writing and copy all parties, the claimant can request Administrative Approval from this department and it maybe granted. NOTES FOR PI When reading the doctor's rating and report, make sure they are using the correct body part. Upper extremity involves the shoulder, elbow and arm. Lower extremity involves the leg; the foot is not part of lower extremity. Do not convert a rating to whole person if only one body part is involved. The spine/back is not whole person, but is still 350 weeks. Anatomical Planes of the Body Second, you will consider the planes of the body. Understanding these will facilitate learning terms related to position of structures relative to each other and movement of various parts of the body. FRONTAL (or coronal) separates the body into Anterior and Posterior parts MEDIAN (or midsagittal) separates body into Right and Left parts HORIZONTAL separates the body into Superior and Inferior parts SAGITTAL any plane parallel to the median plan TERMS OF RELATION OR POSITION superior (closer to the head Inferior (closer to the feet) reference point – horizontal plane posterior (dorsal) closer to the posterior surface of the body medial anterior (ventral) closer to the anterior surface of the body reference point – frontal or coronal plane medial (lying closer to the midline) lateral (lying further away from the midline) reference point – sagittal plane Proximal closer to the origin of a structure distal further away from the origin of a structure reference point – the origin of a structure superficial deep reference point – surface of body or organ median reference point – along the midsagittal or median plane intermediate between two other structures external internal Refers to a hollow structure (external being outside and internal being inside supine prone face or palm up when laying on back, face or palm down when lying on anterior surface of body cephalad caudad Toward the head, toward the tail (feet) TERMS OF MOVEMENT flexion extension increasing angle with frontal plane decreasing angle with frontal plane abduction adduction moving away from or toward the sagittal plane protraction Retraction moving forward or backward along a surface elevation depression raising or lowering a structure medial rotation lateral rotation movement around an axis of a bone pronation supination placing palm backward or forward (in anatomical position) circumduction combined movements of flexion, extension, abduction, adduction medial and lateral rotation circumscribe a cone opposition bringing tips of fingers and thumb together as in picking something up