Rehabilitation for Children after Major Trauma
advertisement

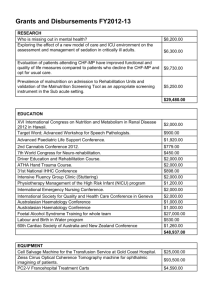
The North West Children’s Major Trauma Network Completing the Jigsaw: Putting the Pieces Back Together Again. Rehabilitation for Children after Major Trauma Friday 24th April 2015 at the Centre, Birchwood, Warrington, WA3 6YN Report nwchildrenstrauma.nhs.uk Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 1 Contents 1. Introduction 2. Objectives of the Day 3. The Outline of the Day 4. The Target Audience 5. Summary of sessions i. Overview of Rehabilitation in Children after Major Trauma Nicola Adamson, Associate Director of Strategy Royal Manchester Children’s Hospital ii. Rehabilitation in the Context of the Major Trauma Pathway Helen Blakesley Rehabilitation Coordinator Royal Manchester Children’s Hospital/Sharon Charlton Rehabilitation Coordinator Alder Hey Children’s Hospital iii. Psychological Impact of Major Trauma on Children :Stewart Rust, Consultant Clinical Psychologist Royal Manchester Children's Hospital and Dr Victoria Gray Alder Hey Children’s Hospital iv. Return to Education :Tracy Gallier Assistant Head Teacher. Royal Manchester Children’s Hospital v. NHS England Overview and Paediatric Neurorehabiltation: Anthony Prudhoe NHS England vi. Neurorehabilitation after Major Trauma: Dr Ram Kumar Consultant Paediatric Neurologist Dept. of Neurology, Alder Hey Children’s NHS Foundation Trust vii. A therapist’s view of complex step down from hospital to community care: A case study Gareth Troughton MCSP Specialist Paediatric Physiotherapist St Anne’s viii. Barriers to delivering rehabilitation in the community Dr Lisa Kauffmann Consultant Community Paediatrician Manchester ix. Rehabilitation of the child following femoral shaft fracture and fracture management with external fixation Rose Davies Orthopaedic Nurse Specialist Sharon Atherton Senior Physiotherapist Orthopaedics Alder Hey Children’s Hospital x. Traumatic Amputation Dr Fergus Jepson, Consultant Rehabilitation Medicine , Lancashire Teaching Hospitals Trust Workshops i. ii. iii. iv. How can the Transition of Children’s from Paediatric to Adult Services for Rehabilitation after Major Trauma be improved? Groups led by Krystina Walton and Stewart Rust How can Step-down from the Tertiary Centres to local care be improved? Lisa Kauffman & Rob Boon What should future rehabilitation services for Children after Major Trauma look like and how should they be resourced ? Nicola Adamson Rachel Greer 4.How can a Children’s Major Trauma Rehabilitation Network be developed in the North West? Helen Blakesley and Sharon Charlton Closing Comments : Miss N.Davis, Joint Clinical Lead NW Children’s Major Trauma Network 8. Appendices Appendix 1 : A Young Persons Experience of Major Trauma Care Appendix 2 : Programme : Completing the Jigsaw: Putting the Pieces Back Together Again. Rehabilitation for Children after Major Trauma Appendix 3: Delegates Registered Completing the Jigsaw: Putting the Pieces Back Together Again. 7. Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 2 1.Introduction In the North West of England, North Wales, and Isle of Man in 2013/2014 there were 350 children who experienced major trauma. Currently the majority of rehabilitation for Children after the Major Trauma event if required is provided in the two children’s major trauma centres at Alder Hey and Royal Manchester Children’s Hospitals. This can mean when hospitalised that children are a long way from their homes and this results in additional stress on the child and their family. After discharge children and their families can be required to undertake long journeys to the Children’s Hospitals disrupting school and family life. 2.Objectives of the Day The objectives of the event were 1. Initiate a Children’s Rehabilitation Network in the North West of England, North Wales and the Isle of Man 2. Map services across the North West, North Wales and the Isle of Man 3. Share knowledge of the Major Trauma pathway for Children 4. Identify expertise outside the Children’s Major Trauma Centres in rehabilitation for Major Trauma who can support service development in the North West 5. Develop a model for Children’s Rehabilitation after major Trauma in the North West 6. Seek support from Commissioners in developing the service 3. The Outline of the Day The day was divided into 4 main themes 1. 2. 3. 4. Overview of Rehabilitation in Children after Major Trauma Rehabilitation in children after Traumatic Brain Injury Rehabilitation in children after Orthopaedic Major Trauma Group Work on Transition of Children’s from Paediatric to Adult Services for Rehabilitation after Major Trauma Step-down from the Tertiary Centres to Children’s Local Services after Major Trauma Future rehabilitation services for Children after Major Trauma how they be resourced How can a Children’s Major Trauma Rehabilitation Network be developed in the North West 4. Target Audience The audience targeted for the day are professionals in the NWChMTN area including Therapists, Clinicians in primary care and hospital services, Secondary Care and Community Paediatric Nurses, Commissioners Managers Education professionals and Clinical Psychologists. Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 3 5.Summary of sessions Overview of Rehabilitation in Children after Major Trauma Introduction: Nicola Adamson, Associate Director of Strategy Royal Manchester Children’s Hospital Presentation included a teenage girl’s perspective of the care she received after major trauma before the Major Trauma Network was established in 2012 . Issues highlighted included the traumatic impact of the initial event, issues about being cared for so far from home, transferring out of intensive care to critical care to high dependency and feeling vunerable on a general ward. Once discharged the difficulties of returning to education were described , issues about availability of physiotherapy, feelings of isolation and depression and eventual description of feelings of recovery 5 years after the initial major trauma. Rehabilitation in the Context of the Major Trauma Pathway Helen Blakesley Rehabilitation Coordinator Royal Manchester Children’s Hospital/Sharon Charlton Rehabilitation Coordinator Alder Hey Children’s Hospital An overview was given of rehabilitation in the context of the Major Trauma Pathway. Information was given on how children present, prehospital care, NWAS prealerts , Bypassing local trauma units of patients to take to the MTC and 45 minute isochrones . Explanations were given of how Major Trauma is defined by Injury Severity Scores. Psychological Impact of Major Trauma on Children :Stewart Rust, Consultant Clinical Psychologist Royal Manchester Children's Hospital and Dr Victoria Gray Alder Hey Children’s Hospital All types of traumatic physical injury can have significant psychological impacts on children and families. Medical treatment for physical injury can also have significant psychological impact. Psychological needs are wider than PTSD / PTSS Psychological Needs can emerge over time and can be long term. Parents are really important and their reactions can determine how children respond. Children (and Parents) need to regain a sense of safety and it’s everyone's job to help them do that. Return to Education :Tracy Gallier Assistant Head Teacher. Royal Manchester Children’s Hospital Overview was given of the Royal Manchester Children’s Hospital School and case examples given of children who had experienced Major Trauma .In any given year there are some 100,000 children and young people who require education outside school because of illness or injury. In addition, there are a significant number of children who experience clinically defined health problems .The situations of these young people will vary widely but they will all run the risk of reduction in self-confidence and educational achievement. NHS England Overview and Paediatric Neurorehabiltation: Anthony Prudhoe NHS England Subjects discussed included -Five Year Forward View ;what are the drivers of change? :New care models; Specialised commissioning and co-commissioning ; new care models ;specialised commissioning and co-commissioning .Specialised paediatric neurorehabilitation Neurorehabilitation after Major Trauma: Dr Ram Kumar Consultant Paediatric Neurologist Dept. of Neurology, Alder Hey Children’s NHS Foundation Trust Rehabilitation begins from the initial emergency response (early supportive care) Through inpatient stay (acute and post-acute rehabilitation) To return into the community (cognitive and educational rehabilitation, complex community rehabilitation, vocational rehabilitation, slow stream rehab, psychiatric rehab)Neurorehabilitation after Major Trauma consists of 2 main groups: the walking Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 4 wounded; and the complex inpatients .Not all the rehab can be provided by one person or team at all stages in recovery and long-term. A therapist’s view of complex step down from hospital to community care: A case study Gareth Troughton MCSP Specialist Paediatric Physiotherapist St Anne’s A case study was presented of a 10 year old girl, running outside house and hit by a car that had loss of consciousness and was air lifted to Alder Hey. Issues which the case highlighted included greater inclusion of community teams in discharge planning. Avoidance of common holiday periods for discharge! Better access to specialist treatment options & equipment Better use of information technology and communication for community services Post-op protocols & clinic letters . Staff numbers in the community . Barriers to delivering rehabilitation in the community Dr Lisa Kauffmann Consultant Community Paediatrician Manchester Knowledge and skills are out there too in Community In addition there are special skills in witness and develop understanding of the life experience of the children and their families Understanding of child development and rehabilitation of many conditions Access to, understanding of, and empathy for local social and educational services .It’s all about communication, mutual respect, Effective information sharing Meetings when everyone important can attend Written information in advance, listening. The knowledge, skills and desire are there in the community the current community delivery model doesn’t work for acute rehabilitation, but could do There is not currently enough resource We need to listen to and respect each other if we are going to provide joined up care for families Rehabilitation of the child following femoral shaft fracture and fracture management with external fixation Rose Davies Orthopaedic Nurse Specialist Sharon Atherton Senior Physiotherapist Orthopaedics Alder Hey Children’s Hospital The session illustrated the Orthopaedic rehabilitation pathway using the examples of children with femoral shaft fracture and children requiring limb reconstruction with external fixation. This included treatments including hip spica, fixed traction and flexible nailing ( dependent on age) Fractured femur is a difficult diagnosis for a family – no quick simple fix. Parents happy with traction as long as child is comfortable Hip spica option does not offer a great deal more normality, it involves GA and risk of position loss. Surgical option only benefits a child old enough to use crutches Support of Hospital at Home is well received but community nursing input not always available . There are a reduced numbers of nurses and doctors skilled in traction The role of the physiotherapist includes liaison with MDT. Pre op explanation. If possible Ensure adequate pain control prior to any treatment intervention Observe pressure ,colour, and active movement Explanation pre-treatment Ensure good resting position Oedema management. Traumatic Amputation Dr Fergus Jepson, Consultant Rehabilitation Medicine , Lancashire Teaching Hospitals Trust Overview given of service available for amputees in Lancashire Teaching Hospital Trusts. Different prosthesis described . Numbers of children under his care low and are treated as a priority group. The management of expectations of type of prosthesis was discussed. Dr Jepson was willing to take referrals for children if advice needed. Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 5 6.Workshops 1. How can the Transition of Children’s from Paediatric to Adult Services for Rehabilitation after Major Trauma be improved? Groups led by Krystina Walton and Stewart Rust What are arrangements in place now ? Currently variable. Examples of good practice in CF and Burns Where are the gaps ? Communication A 16 - 18 year old hole i.e. Children’s services end at 16 , Adults start at 18. In some stand-alone Trusts difficult to link Pathways unclear to who or what ? Geographical variation Processing health different to social services What needs to be in place ? A rehab tariff that acknowledges transition National standards that are currently and honestly applied Key workers case manager for transition Cross over transition clinics – staffed by Adult Child Team Hand held records Planning for transition from a younger age Dissolve Organisational Boundaries Promote Collaboration not competition Tripartite funding – clearer, quicker and more transparent What actions need to be taken and by who? Alder Hey : Transition Champion Karl Emerson Neurorehab NHS England has to pay for it Complex need Maria Burney Reignite Trusts interests in Transition We can agitate/advocate for transition- be passionate about our jobs 2How can Step-down from the Tertiary Centres to local care be improved? Lisa Kauffman & Rob Boon What currently happens ? Local teams are invited into MDT re discharge Early involvement with discharge Can the process be improved ? Yes How could it be improved ? Access to hospital notes by local teams Joint teaching sessions Local Leads Standards of care for rehab A rehab package for every child Advising what the local team needs to do especially for less severe major trauma Clear discharge plans Clear pathways to community and for them to be clear who they are to interact Wheelchairs Early communication with local units Knowing who the local leads are What actions need to be taken and by who ? Improving the rehab prescription – make sure its comprehensive Need a patient passport Early communication local unit Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 6 3What should future rehabilitation services for Children after Major Trauma look like and how should they be resourced ? Nicola Adamson Rachel Greer What do the rehabilitation services for children after major trauma are in place now? Services depend where you live Where the gaps are Rehabilitation Services for Children, are services in the right place? Access to equipment hydrotherapy variable Communication with hospital teams Lack of coordination IT Gaps and Differences in Community Services Some teams look after children with specific conditions some don’t Services that meet the specific needs of cultural groups Services are not equitable depends where you are Lack of continuity in some services What needs to be in place and how should it be resourced ? Rehab Tariff that follows the patient Specialist Outreach Team A network to drive change Equipment and Wheelchairs Specialist Outreach team Full MDT to include health and Education What actions need to be taken and by who? A network that builds relations Centralised patient held records Use of IT to support Community Teams, Allow people to attend a virtual MDT Focus on preparing families for going home back to community Advocate with commissioners for a tariff for paediatric rehab Needs to be an equivalent Tadworth of the North Need locality based hubs for patients – Liverpool and Manchester great but Lancashire less well served 4How can a Children’s Major Trauma Rehabilitation Network be developed in the North West? Helen Blakesley and Sharon Charlton What would be the Network Objectives be? Map the gaps Build evidence to support practice Communication on line – directory better local links Positive referral pathways – all areas signed up to Who should be members of the Network? Geographical representation GP/Patient and parent involvement Therapy, Nursing, Sch Nursing HV, paediatricians, education, social care ,voluntary sector How would the Network Function? Meet /contact regularly Work together on equipment, rehab prescriptions, structure to plan discharge What actions need to be taken to develop a network for Rehabilitation after Major Trauma ? List of contacts to develop a Directory Wok together outreach Website – all professionals have access , Accept referrals, training events , share knowledge Work with not for profit sector Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 7 6.Concluding Comments ; Naomi Davis 1. 2. 3. 4. 5. There is a need for a Rehabilitation network for Children after Major Trauma Standards should be set in Rehabilitation extend beyond neurorehabilitation Services for Rehabilitation for Children after Major Trauma must be cohesive The Idea of In reach from community services into tertiary care as well as outreach from tertiary children’s centres 6. Communication and IT solutions must be explored 7. Equity of Care for rehabilitation needs to be achieved across the North West 8. Plans need to be drawn up from the day for the next steps Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 8 Appendix 1 A Young Persons Experience of Major Trauma Care The Accident In September 2010 I was involved in a car accident. I have no recollection of the event (or for several days before) and there is some confusion over what actually happened. It is thought however, that the horse I was looking after at the time, Blue, spooked in the yard whilst we were getting ready for a competition the following day. A series of unfortunate events led to the gate being wide open at this point, with an extremely fit horse heading towards it. Although I would always say that people should put their own safety before anything else this is something we rarely do when a loved one is in great danger and there is little time to think. I have been told that I attempted to stop Blue in his tracks. My Dad, who was with me at the time, said that I was successful and I had him heading back towards the gate before Blue made a second attempt for freedom. Unfortunately this time he was successful and with me hanging on to him ran down the drive and into the main road. Although this road is not the busiest and regularly has long gaps with no traffic, sadly the moment we reached the road we were in the path of a Landrover. In many ways we were fortunate as the driver happened to be going below the speed limit in an area where a large number of people speed. The landrover collided with Blue, and possibly myself- we are still not sure, before Blue fell on top of me. Blue weighed around 400kg. As with most horses (and men!) he only had thoughts for food and with what I have assumed to be several broken legs he got himself to the grass verge and spent the last hour of his life eating grass. I like to think he would have been happy. I on the other hand was lying unconscious in the road. I had my airway opened by the farmer whose yard it was, a family friend who happened to be a bank theatre nurse in his spare time. A lady who had learnt first aid off her mountain rescue husband arrived at some point and held my head still. Whilst this was going on, my Mum had been rung by the farmer’s wife and he was on the phone to the ambulance service. Mum, who thought I’d just had a bump in the yard was shocked to find the road blocked and the flashing lights of police cars. Pre Major Trauma Centre Care The North West Air Ambulance arrived and I was treated by them and an on-call anaesthetist at the scene before being flown to Preston Hospital. There I was stabilised, given blood transfusion, ventilated and decisions were made about whether to start operating now or leave it all to a specialist paediatrics hospital. My parents had been driven by the first aider and one of my brothers had driven himself, unaware of how serious the situation I was in. I will always remember Mum telling me at a later date that the A&E consultant came out and told them to get anyone there that needed to be because he didn’t think I would survive. Apparently my brothers face dropped, we are extremely close and I can only imagine how I would feel if our roles were reversed. My eldest brother was rung in London as well as my Godmother and my uncle who was a paediatrician. I am unsure about the timing in this but it was decided that I needed to go to PICU and a bed was free at RMCH. I was transferred in the middle of the night by road ambulance accompanied by medical staff. Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 9 Major Trauma Centre Immediate Care I was met by a fantastic team of consultants covering a wide range of specialities including orthopaedics, urology and general surgery. My Dad and middle brother had gone home to get things they thought we might need whilst my mum and eldest brother drove to Manchester. That night I was in surgery for twelve hours. I had broken my pelvis in multiple places, ruptured my diaphragm and had a compound fracture of my right humorous amongst many other breaks, scrapes and tears. I had an external fixation put on my pelvis until a pelvic specialist from Wigan could come to repair it. My orthopaedic surgeon was very worried about the nerve ending in my arm and there was a fear that my right arm would be paralysed. I have been told there was great excitement when I wiggled my fingers for the first time! Intensive care ( 2 weeks) Pain relief I remember very little of intensive care. I was ventilated for the first seven days and then the sedation was lifted. At this point, through the eyes of the intensive care consultant I was better and he was happy to wheel me next door to HDU but the other consultants objected and I stayed for another week. I have flashbacks of severe abdominal pain and I know the pain team spent lots of time with me trying to get it under control. Morphine wasn’t effective and in the end I was put on ketamine, quite ironic considering the nature of my accident. Personal Care When I came round I got very irritated by the beeping of my machines which seemed to be set off by the slightest movement and I had a few demands for my parents; apparently I invented my own sign language to communicate these! Firstly and most importantly I wanted my legs shaving! Very important aged 14. One nurse sent Mum off to Superdrug with a list of things she thought would make me more comfortable including nice soap, a razor and lip balm. On day ten a pelvic specialist came and I spent a further seven and half hours in theatre where he put two plates in. I have no recollection of meeting him but one of my most clear memories is having my hair washed and French plaited a few days later by a fantastic nurse so I could feel pretty (when I was very unattractive) for my friend coming to see me. Although some may think that having smooth legs and clean hair is very trivial in the grand scheme of things, it was these small things that made such a huge difference to my happiness which I believe affected my recovery. Physiotherapy Now that I was awake, all though very drugged up, lessons and physiotherapy began. I never thought there would be lessons in intensive care but there I was telling my new teacher, extremely slowly, what 2 x 3 was. My physio began with tiny finger stretches and elbow extensions as the elbow joint of my broken arm was locked in flexion. I also had a chest physio who had a small plastic object I had to blow in to, trying to raise a tiny ball. I did quite well at avoiding the teachers; because I had so many consultants and two physios I was quite often being seen by one of these when they arrived so they left me to it! Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 10 Transfer out of Intensive Care to High Dependency On day 14 I was moved to high dependency. I found it quite confusing to no longer have my own nurse and I know my parents were worried about it too. It was a big change. It was on this ward that demands first started being made of me. One consultant was insisting that I had my catheter taken out due to the risk of infection. In my eyes he didn’t realise the difficulty I would have using a bed pan or the fear a teenage girl has of wetting the bed. Even when I was very poorly I felt embarrassed about such issues. At the same time the same consultant was demanding that I had what appeared to be enema after enema as my bowels hadn’t been open for over three weeks. Although I now know that he meant well and that he was worried he would need to operate again at the time I was very confused about having things put up my bottom! The physios began using the hoist to get me out of bed and sat in a chair which was a huge step forward. I got along with the nurses on HDU like a house on fire. One night, mine logged on to my Facebook account on her phone for me and read out all the messages people had been leaving for me. I was most pleased to hear that several of the rugby team at the local boys grammar schooled had posted comments and it was great to hear from the girls at school too. Nutrition/ Appetite in High Dependency I developed severe nausea during my time on HDU which I was given cyclazine for, extremely effective for short periods of time until I had an allergic reaction to it causing scary uncontrollable shaking. The nurses were trying to tempt me with food but I had no appetite. My first attempt was ice cream; I had a tea spoon, decided I was full and gave the rest to Dad. Next I tried toast several times and threw up after each lot, having only taken a couple of bites. It took me many years to get over my fear of toast but I now happily eat it! Realisation of Loss It was on HDU that it really sunk in that my beloved horse was no longer with us. He had helped me get through many hard times and we had developed a strong bond so I was obviously very sad. Dad brought me some pictures in of him so I could think about all the good memories we had. The physios began getting me to stand with a Zimmer frame, starting with only a few seconds. It was incredibly difficult and I am still shocked at how quickly muscle wastes. It was decided that I would remain in HDU until I was well enough to travel to Lancaster Hospital, where I would be close to my home and my friends. Mum went home for the first time after a week in HDU; she stayed a night before coming back with two of my school friends. Move to a General Ward It was with some surprise that when she arrived back at the hospital she found her daughter confused and upset being moved from HDU to a general ward when this wasn’t part of the plan. With the time it took to move me I barely saw my friends before they had to go home again, they had travelled 60 miles to see me and only had a few minutes with me. Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 11 Vulnerability /Personal Care on General Ward I stayed on the ward for two weeks and it was the only part of my hospital experience I found unpleasant. I was put on a side ward with three young toddlers and three creepy Dads. One introduced himself by saying he had only just got custody of his child as his wife had stabbed someone and another only came to see his child when social services were coming. The third spent ages complaining about the service his child was receiving and even told us that a few weeks ago he hadn’t been able to see a doctor all day because they were in theatre for twelve hours... I wonder who had caused that! I got very little sleep which I found very difficult. As previously I had been sleeping most of the time and was awake at funny times like the middle of the night. I found the nurses had very little understanding, and I might even say interest, in how poorly I had been and still was. I also found most of them didn’t smile and this was very unwelcoming, particularly on a children’s ward. I am shocked to tell you that whilst I was on the ward I wasn’t actually offered a wash. My Mum had been helping with my care previously but now she was left to do it all. Me and my mum have a great relationship and I was quite happy for her to wash me but the majority of my teenage friends would have been mortified being seen naked by their mother and yet no one asked me if I was happy with this arrangement. Also there was no bath hoist or shower chair so Mum had to shower me in the wheelchair (Don’t tell the physio’s!) One night during my patient checks I was found to have a temperature of 43.5 degrees Celsius. I had lost nearly two stone and as a result I was very cold all of the time, I had several blankets and thick fluffy socks to keep me warm. These were quickly whipped off me despite my protest and the doctor was called. I had not yet covered much human biology at school and although I knew the human body temperature should be 37 degrees I did not understand why a few degrees mattered so much. The situation was improved remarkably when an extremely handsome doctor arrived to see to me. He discovered my central line had become infected so he took it out and gave me antibiotics. After this I was moved to my own room and could finally sleep as much as I needed to. It was now that I was told I really had to start eating or I would have to go back to theatre to have another central line fitted. I can honestly say that eating was the most difficult part of my recovery but I tried my best and ate minute amounts of plain rice or jacket potato which I managed to keep down. Nutrition My nausea remained very bad and I did not want to eat. I met with a dietician who gave me protein drinks to try and increase my weight without having to eat huge amounts. Things progressed very quickly all of a sudden and one day I had a go with crutches. I got the hang of these rapidly and could soon get to the toilet by myself and hop up steps. I could only use these for a short period of time due to my broken arm and used a wheelchair when I had a further distance to travel. I had little trips around Manchester in my wheelchair, wrapped in blankets to keep me warm. The plan had still been to transfer to Lancaster but Mum and my consultant decided that the eating difficulty could be best managed at home! After five weeks, a much shorter time than expected, home I went. This was just the beginning! Discharge Home On the way to the car I saw my face in a mirror for the first time and couldn’t believe it was me. I had become so thin that I hardly recognised myself. I slept for the majority of the car journey home and Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 12 became apparent how painful I would find speed bumps for the next six months, no matter how slow we took them. I was very excited to tell my friends that I was coming home but I quickly realised their lack of understanding of my situation when I was asked if I would be back at school on Monday. I was thrilled to back in my little village and to hear the birds singing again. I found home cooked food much easier to stomach although I still ate miniscule amounts and I relished having a duvet and my favourite teddy bear again. Wheelchairs My OT assessment at the hospital had resulted in me coming home without a wheel chair as apparently these could only be given to those who really needed them and I didn’t class as that. Had it not been for kind neighbours who leant me their own I would have been housebound as I could only travel very short distances on my crutches. The local OT came round very quickly to deliver the items it had been decided that I needed. She was extremely confused as to why I hadn’t been classed as needing a wheelchair and ordered me one. This was delivered in only a couple of days and was very light weight so my parents found it much easier to push that the one we had borrowed. Personal Care at Home We had difficulties using the shower in my bathroom as the door is very narrow and there was little room for my carer (mum) to help me get in or wash me. I am fortunate to live in an area full of incredibly kind people and my neighbours offered me the use of their wet room with a walk in shower. There was plenty of space and they even gave me a stool to sit on. I remember the shock of the Manchester OT’s when they heard I would be using a neighbour’s bathroom as I imagine this would never happen in cities! Getting washed took such a long time as I could do very little for myself. We usually found the morning was gone by the time I had eaten breakfast and had a shower. I remember finding simple tasks such as brushing my teeth or my hair incredibly difficult and tiring. One of the problems we faced was that you can’t get temporary blue badges for disabled parking so it was often a struggle when we went out in the car. Physiotherapy at Home In the first week of me being home I was in the village swimming pool. I used the hoist to get in which was quite daunting and with the support of Mum and the use of floats I had a splash around and did some floating. I wasn’t in long as I became tired so quickly and then there was the slow process of getting washed and dried. I have always loved swimming and I felt a huge sense of freedom to be able to move around a bit by myself. I also started going to physio at Lancaster hospital this week. I went twice a week for the next few months. And have been on and off for the last few years. They particularly worked on my core stability and continued with the arm extension exercises. It was through physio that I became involved in hydrotherapy. Our local hydrotherapy is run by two physios and it is a charitable organisation. I started by just walking with floats and other simple exercises but I progressed quite quickly as my muscles began to strengthen again. Very quickly my left leg became twice the size of my right leg just from weight bearing. I attended hydrotherapy for one year and it was of huge benefit to me. Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 13 Relationships with Friends and School I became very isolated at home as my school friends had quickly lost interest in me. None of them came to visit once I was home and I became very used to the company of those much older than me. I had a trip in to school in November where once again I became exciting although it was short lived. I had home schooling with different lessons a few times a week covering the basics of maths, science and English but I struggled to concentrate for more than a few minutes at a time. The teachers were very patient and took their time with me, going over things until they stuck. Outpatient Appointments At the end of November I had my first outpatient’s appointment with my pelvic specialist in Wigan. He asked me how I was feeling and then told me to walk to x-ray! It was the most peculiar feeling to walk again after nearly three months of non-weight bearing on my right leg and I felt extremely wobbly! I tottered to and from x-ray and was thrilled to find out my x-rays showed great healing of the bones. It then asked the all-important question of when I could ride again and he told me he was happy for me to ride now! Although I could now walk I needed to use my wheelchair for long trips as I still became very tired and my right leg was weak. Back on a Horse The next Saturday I went to my riding school. The girls were thrilled to see me walking and when I told them I could ride again my favourite horse was tacked up in minutes. With my riding instructors help I climbed on board and had a walk around, I had rather a large audience and I think most of them were crying! It was the most fantastic feeling to be back on a horse but an incredibly emotional one too! The next week I visited the children’s hospital for outpatients and was told very firmly that I should not be riding by my General surgeon... It didn’t stop me but I did take it very slowly! Returning to School It became apparent that I would have to go back to school earlier than I should purely for social reasons. For some reason the government will not let a patient be home schooled at the same time as going into school for short visits. We had tried to get me back to school much earlier but I was told I could not attend school in my wheel chair as I was a fire risk! How this is acceptable in the 21st century I don’t know, and I still get very angry about it. I had my first session at the end of December just before we broke up for Christmas so my home schooling stopped then. I only stayed for a couple of hours and even though it was very relaxed work I was exhausted. I started going back part time in January; I started by doing a few hours a week and building up. Mum had to drop me off and pick me up at the door and I remember feeling completely zoned out and taking in almost nothing for the first few months. My teachers did not understand and I was regularly shouted at for not remembering things and for not attending all the lessons. It was difficult because I had recovered so well physically and looked perfectly fine but I was still so tired all the time. The teachers had obviously never come across serious health issues and had no idea how to cope with them. I attended a very highly sort after Grammar school but I have a very poor opinion of it after my experience. They should have been pleased just to see me in lessons but the worry of me ruining the GCSE results was too much of a risk for them. I was put under incredible pressure to drop subjects that I really enjoyed including history and food technology so that I could focus on the core Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 14 subjects and even told that “perhaps the school wasn’t for me”. I was told that I would never catch up and I was predicted D’s or E’s in an environment where few girls get below an A. My self-esteem plummeted and every day was difficult. I no longer fit in with the other girls at school, I had been forced to grow up very quickly and there was nobody I connected with. Despite being at school for the social reasons I became more and more isolated. By Easter I was nearly back in full time education, only missing the one day for a rest and hydrotherapy. I had been offered a place at another school and a lot of me wanted to accept it but being an extremely determined (some may say stubborn) girl I refused to let the school win and stuck it out. The sense of relief I felt when the summer holidays arrived was huge. I spent a lot of time catching up on school work but we had a long family holiday in Wales where I could chill out and literally forget about all my worries. As September grew closer my fear of returning to school began to grow and to make matters worse I sprained a ligament in my sacroiliac joint causing incredible pain, difficulty moving and once again having to have mum wash and dress me. Psychological effects I became very depressed, although people who knew nothing of my current situation tried to tell me I wasn’t, and it was at this point that I began to see my GP very regularly. I am very lucky to have such a wonderful doctor who put me on the end of his day so I could stay and talk as long as I needed to. He managed to get me bumped up the list for seeing a psychologist who I also saw regularly. With the combination of the two I managed to stay relatively calm at school. I was still exhausted all the time, always being in bed by 8pm at the latest, having no social life and still struggling at school the next day. Perceptions of School The school continued to be very unsupportive and there were several heated arguments between me and my deputy head. I had been awarded ESAP funding giving me £3000 a year to help get me back into education and the school were spending none of it and hoping to keep it for themselves. We did spend some on private lessons in maths and science and found these extremely useful. I fought the entire to time I was at school and eventually I reaped the reward. After missing nearly six months of my first GSCE year I achieved five A*’s, three A’s and a B ! It makes me even happier to say that two of my A*’s were in History and Food Technology, the subjects I had fought to carry on. Continuing effects of accident 3 years before It is amazing how even health professionals have a lack of understanding about how long it takes to recover. I was told by several doctors that I was better and had to get over it but they weren’t living my life with my body. Three years after the accident and I was still under three consultants following issues related to the initial injuries. I still suffered with severe nausea and I was still struggling to eat. It turned out that the volume of tablets I was taking to cope with this raised my prolactin level so high that my periods stopped and I was suffering from other gynaecological problems which caused me severe pain and it turned out that I had damaged nerve endings in my vagina. It was here again that my GP was very useful, we still saw each other regularly and we tried different medication until we found the ones that worked best. Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 15 Recovery It is now coming up to five years since that accident and I’m pleased to say that I no longer have any consultants, I no longer see my GP regularly and I am loaning a beautiful (but huge) horse! I completed my A levels last year and I am currently in my Gap Year and enjoying it thoroughly. I work as a receptionist in a GP surgery and as an ambulance care assistant on a private ambulance. I have been to Uganda on a medical mission for three weeks and have an exciting summer of travelling and horse competitions coming up before I go to university in September. I am going to Bradford University to study clinical sciences before hopefully going on to study medicine at Leeds University. Advice for Professionals I would like to offer you two pieces of advice; firstly to smile at your patients and secondly don’t judge a book by its cover. Just because a patient looks well it doesn’t mean they are! It takes a very long time and a huge number of people to ensure full recovery after major trauma. Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 16 The North West Children’s Major Trauma Network Completing the Jigsaw: Putting the Pieces Back Together Again. Rehabilitation for Children after Major Trauma Friday 24th April 2015 at the Centre, Birchwood, Warrington,WA3 6YN Time 8.15- 9.00 9.00 -9.05 Subject Registration Opening Comments Speaker Nicola Adamson Associate Director Strategy, Royal Manchester Children’s Hospital Session 1 Chair :Rachel Greer Manager Head and Neck Alder Hey Children’s Hospital 9.05 – 9.25 Rehab in Context MT Pathway Helen Blakesley Rehabilitation Coordinator Royal Manchester Children’s Hospital/Sharon Charlton MCSP Rehabilitation Coordinator Alder Hey Children’s Hospital 9.25-9.35 Patient perspective TBC 9.35- 9.55 Psychological Impact MT Stewart Rust, Consultant Clinical Psychologist Royal Manchester Children's Hospital 9.55 – 10.15 Return to Education Tracy Gallier Assistant Head Teacher. Royal Manchester Children’s Hospital 10.15- 10.35 NHS England Overview Anthony Prudhoe Programme of Care Manager NHS England 10.35-11.00 Coffee/Tea Break Session 2 : Chair Bimal Mehta : Joint Clinical Lead North West Children’s Major Trauma Network 11.00-11.20 Neurorehabilitation after Major Dr Ram Kumar Trauma Consultant Paediatric Neurologist Dept. of Neurology, Alder Hey Children’s NHS Foundation Trust 11.20 -11.40 Community Therapists and Rehab Gareth Troughton MCSP Specialist Paediatric Physiotherapist St Anne’s 11.40 – 12.00 Complex Step down Lisa Kauffman ,Consultant Paediatrician 12.00 -13.00 Lunch Session 3 : Chair Naomi Davis Joint Clinical Lead North West Children’s Major Trauma Network 13.00 -13.20 Fractured Femur / Limb Rose Davies Orthopaedic Nurse Specialist Reconstruction : Rehabilitation in Sharon Atherton Alder Hey Children’s Hospital children 13.20 – 13.25 Questions 13.25-13.50 Traumatic Amputation Dr Fergus Jepson, Consultant Orthopaedic Medicine , Lancashire Teaching Hospitals Trust 13.50 – 13.55 Questions 13.55 – 14.40 Break out Group Work Workshop 14.40 – 15.00 Coffee/Tea 15.00 -15.20 Feedback Group Work 15.20 -15.40 Overview and Way Forward Miss N.Davis, Joint Clinical Lead NW Children’s Major Trauma Network. 15.40 – 16.00 Concluding Comments Dr Mehta Joint Clinical Lead NW Children’s Major Trauma Network Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer Page 17 Delegates Completing the Jigsaw: Putting the Pieces Back Together Again. Rehabilitation for Children after Major Trauma Friday 24th April 2015 at the Centre, Birchwood, Warrington,WA3 6YN NAME 1. Adamson, Nicola 2. Aitken,Iris 3. Atherton Sharon 4. Bacon Wendy 5. Barnes Lynne 6. Bedson Chris 7. Bell Ingrid 8. Benbow Helen 9. Benstead Jacqueline 10. Blakesley Helen 11. Boon Rob 12. Booth Nicola 13. Brennan Adele 14. Brown Amanda 15. Brown Shelley 16. Butler Frances 17. Chamberlain Jeanette 18. Charlton Sharon 19. Clancy Tanya 20. Dainty Jennifer 21. Davies Rosemary 22. Davies Leanne 23. Davis Naomi 24. De Goede ,Dr Christian 25. Dixon Gill 26. Dunning Annette Job Title , Organisation Associate Director Strategy, Royal Manchester Children’s Hospital Assistant Practitioner, NMW/TCU Alder Hey Children’s Hospital, Liverpool Alder Hey Children’s Hospital, Liverpool ODN GM Care Co-Ordinator, Children’s Community Assisted Ventilation Service Royal Blackburn Hospital. Lead Nurse/Matron, Paediatric Family Divison Royal Bolton Hospital Ward Manager NMW/TCU, Alder Hey Children’s Hospital, Liverpool Children's Complex Care Specialist Nurse Northwest Commissioning Support Unit, Countess of Chester Health Park Paediatric Occupational Therapist, Bridgewater Community Healthcare, Platt Bridge Health Centre Clinical Therapy Manager for Rehabilitation, Physiotherapy Dept., Royal Preston Hospital Major Trauma Rehabilitation Co-Ordinator, Royal Manchester Children’s Hospital Consultant Paediatrician - Royal Manchester Children’s Hospital Senior Sister Newborn ICU St Marys Family Support, Royal Manchester Children’s Hospital Clinical Manager, CAMHS Families Directorate, Bridgewater NHS Foundation Trust Paediatric Nurse The Complete Group, Telford, Clinical Team Lead, Children’s PhysiotherapyCentral Community Health Centre, , Douglas, Isle of Man Service Manager, NMSS Clinical Business Unit Alder Hey Children’s Hospital, Liverpool Major Trauma Rehabilitation Co-Ordinator Alder Hey Children’s Hospital, Liverpool Team Lead Physiotherapist Paediatrics Royal Oldham Hospital Clinical Psychologist, Alder Hey Children’s Hospital Orthopaedic Nurse Specialist Alder Hey Children’s Hospital, Liverpool Specialist Nurse Practitioner - Neurosciences Acquired Brain Injury Joint Clinical Lead North West Children’s Major Trauma Network Consultant Paediatric Neurologist, Royal Preston Hospital Paediatric Nurse CCNT St Helens and Knowsley NHS Trust Senior Children’s Community Nurse Bridgewater Community Healthcare, L&SC Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer L&SC C&M GM C&M C&M C&M L&SC GM GM GM GM C&M - C&M C&M GM C&M C&M GM GM L&SC C&M C&M Page 18 27. Nicola Durham , 28. Edwards Tracey 29. Ellery Patsy 30. Ellis Pauline 31. Emmerson Karl 32. Fillery Caroline 33. Fissler Sarah 34. Frith Dawn 35. Gallier Tracy 36. Gould Deborah 37. Gray Dr Vicky 38. Greer Rachel 39. Hargreaves Vicki 40. Hazlehurst Kath 41. Hewlett, Kate 42. Hogg Denise 43. Horsley Louise 44. Hutchens Lisa 45. Fergus Jepson 46. Jones Samantha 47. Kauffman Lisa 48. Keable Hannah 49. Kisseh Sarah 50. Kumar Ram 51. Lancaster Rachel 52. Lees Susan 53. Lipshen Gabi 54. Lloyd Gaynor 55. Mehta Bimal Children’s Complex Needs/Additional Needs Sister Paediatric Outreach Team, Royal Preston Hospital Lead Nurse, Paediatrics The Complete Group, Telford, TF2 9TU Ward Manager, Neurosurgical Unit, Alder Hey Children’s Hospital, Liverpool Community Nurse Manager Health Visiting Service, Wirral Community NHS Trust Neurology Clinical Nurse Specialist NMW/TCU Alder Hey Children’s Hospital, Liverpool Occupational Therapist Alder Hey Children’s Hospital, Liverpool Emergency Paediatric Trainee Alder Hey Children’s Hospital, Liverpool Paediatric Occupational Therapist Blenheim House Child Development and Family Support Team, Whitegate Health Centre Assistant Headteacher Hospital Education, Royal Manchester Children’s Hospital Specialist Speech and Language Therapist Bridgewater Community NHS Foundation Trust Consultant Clinical Psychologist Alder Hey Children’s Hospital, Liverpool General Manager, Alder Hey Children’s Hospital, Liverpool Ward Sister, NMW/TCU Alder Hey Children’s Hospital Royal Manchester Children’s Hospital L&SC Advanced Physiotherapist,Liverpool Community Physiotherapy Complex Health Needs Service Lead for Children/Young People Bridgewater Community Healthcare Clinical lead , Paediatric Occupational Therapy, Halliwell Health Centre, Bolton Highly Specialised Paediatric Physiotherapist, Neurosciences, Bristol Children’s Hospital Consultant Orthopaedic Medicine , Lancashire Teaching Hospitals Trust Major Trauma Co-Ordinator, Royal Manchester Children’s Hospital Consultant Community Paediatrician, Royal Manchester Children’s Hospital Trauma & Rehabilitation Co-Ordinator Sheffield Children's Hospital Paediatric Occupational Therapist, Royal Manchester Children’s Hospital Consultant Paediatric Neurologist, Alder Hey Children’s Hospital, Liverpool Chartered Clinical Psychologist Preschool Integrated Services for Children Rowan House Clinical Service Manager Active Assistance Paediatric Trauma Rehabilitation Lead Bolton Children’s Occupational Therapist, Disabled Children’s Services, Liverpool City Council Joint Clinical Lead ,North West Children’s Major Trauma Network C&M Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer C&M C&M C&M C&M C&M L&SC GM C&M C&M C&M GM C&M GM L&SC GM GM GM C&M GM GM C&M C&M Page 19 56. McCullagh Dr Gary 57. O'Neill Cheryl 58. Partington Naomi 59. Pemberton Angela 60. Perera Dr G Sheran 61. Perry Shona 62. Preston,Christopher 63. Prudhoe Anthony 64. Ramirez Roberto 65. Roberts Nia 66. Rodway,Sarah 67. Rust Stewart 68. Sakthivel Kumar 69. Shackleton Tracey 70. Simpson Jayne 71. Smith Barbara 72. Starbuck-Ashton Joanne 73. Sutch Alison 74. Spurling Emma 75. Stringman Laura 76. Sutcliffe Julie 77. Tatham Steve 78. Toman Marie 79. Toft Alison 80. Trenchard Sian 81. Troughton Gareth 82. Vasallo Grace 83. Wafer Mike 84. Walton Dr Krystyna Consultant Paediatric Neurologist, Dept. of Paediatric Neurology, Paediatric Physiotherapist, Bridgewater Community Healthcare, Platt Bridge Health Centre Paediatric Nurse Manager, The Complete Group, Telford, TF2 9TU Clinical Tutor, Radiology Wirral University Teaching Hospital CD Community and Neurodevelopmental Paediatrics. Royal Blackburn Hospital Consultant Acute and Community PaediatricsBetsi Cadwaladr University Health Board Advanced Paramedic Practitioner South Sector North West Ambulance Service Programme of Care Manager NHS England Neurosurgical Consultant,Neurosurgery, Royal Manchester Children’s Hospital Paediatric Physiotherapist Ysbyty Glan Clwyd Children’Occupational Therapist,Rowan House ,Hyde,Cheshire Consultant Clinical Psychologist , Royal Manchester Children’s Hospital Consultant Paediatrician, Salford Royal NHS Foundation Trust Major Trauma Co-Ordinator,Alder Hey Children’s Hospital Practice Educator - Paediatrics Ward E5, Bolton NHS Foundation Trust Quality Improvement Program Lead NHS England Family Support , Royal Manchester Children’s Hospital Disability Nurse Specialist for Children and Young People Bridgewater Community Healthcare, Physio Team Leader Paediatric Occupational Therapy, Halliwell Health Centre, Bolton Community Paediatric Physiotherapist Alder Hey Children’s Hospital, Liverpool Clinical Lead in Paediatric Physiotherapy, Physiotherapy Dept., Royal Preston Hospital Lead Commissioner – Maternity, Children and Families Warrington Clinical Commissioning Group Children’s Complex Needs/Additional Needs Sister Paediatric Outreach Team, Royal Preston Hospital Highly Specialist Team Leader Paediatric Occupational Therapy, Halliwell Health Centre, Bolton Clinical Psychologist Highly Specialist Paediatric Physiotherapist St Anne’s Consultant Paediatric Neurologist, Royal Manchester Children’s Hospital Major Trauma Network Manager Major Trauma Centre, Royal Manchester Children’s Hospital Major Trauma Neuro Rehabilitation Consultant, Hope Hospital, Salford Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer GM C&M C&M L&SC - GM - GM GM C&M GM GM C&M GM C&M L&SC C&M L&SC GM GM L&SC GM GM GM Page 20 85. Williams Clare 86. Wright Elly 87. Wright Linda 88. Wright Liz Highly Specialised Paediatric PhysiotherapistChild Development and Family Support Team, Whitegate Health Centre Specialist Health Visitor Wirral Community NHS Trust Clinical Manager, Children’s Community Nursing Services Children's Specialist Services, Children & Families Directorate Bridgewater NHS Foundation Trust Principal Physiotherapist in Neurosciences Physiotherapy Department Birmingham Children's Hospital Completing the Jigsaw : Putting the Pieces Back Together Again V.1 Author: Mike Wafer L&SC C&M C&M - Page 21