FINAL PRESENTATION
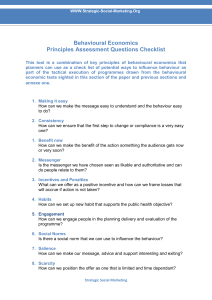
advertisement

Bobbie, Caroline, Jason and Jo Introduction and definitions ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Brain injury –terms Types of traumatic brain injury Neuroanatomy Frontal lobe – overview Orbitofrontal damage Executive functioning Working memory Baddeley’s working model Deficits in executive functioning Neuropsychological assessments Epidemiology Psychological Issues ◦ ◦ ◦ ◦ ◦ ◦ Interpersonal issues Systemic issues Emotional impact Theories of depression Adjustment Behavioural difficulties Interventions ◦ ◦ ◦ ◦ • • Functional analysis Behavioural approaches Aims of cognitive rehabilitation Organisational issues National policy& guidance Ethical issues Summary Discussion Questions INTRODUCTION & DEFINITIONS Types of injury: Acquired brain injury (ABI) “Damage to the brain, which occurs after birth and is not related to a congenital or a degenerative disease. These impairments may be temporary or permanent and cause partial or functional disability or psychosocial maladjustment .” The World Health Organization (1996) Traumatic brain injury (TBI) “Traumatic brain injury (TBI), a form of acquired brain injury, occurs when a sudden trauma causes damage to the brain. TBI can result when the head suddenly and violently hits an object, or when an object pierces the skull and enters brain tissue.” National Institute of Neurological Disorders and Stroke (2012) Difficulties ◦ Lack of consistency with definitions ◦ Brain injury network (2012) has called for this to be addressed Three types: ◦ Concussion: An impact to the head that jars the brain and temporally disrupts its normal functioning ◦ Closed head injury: A concussion or head trauma, the symptoms of which include loss of consciousness after the trauma, confusion, headache, nausea or vomiting, blurred vision, loss of short-term memory and perseverating. ◦ Contusion: A severe head trauma in which the brain is not just jarred but the impact also causes bruising to the brain. (Davey 2008; p.504) No FL damage statistics found Hospital Episode statistics for 2000/2001 112,978 admissions to hospitals in England with a primary diagnosis of head injury. 75% were male 33% were children NICE, (2007) 70-88% of people who sustain a head injury are male 10-19% are aged ≥ 65 years ? Emotional control centre and home to personality Area of brain where damage presents with broadest range of symptoms (Kolb & Milner, 1981) Involved in motor function, spontaneity, problem solving, memory, judgement, language, initiation, social and sexual behaviour and impulse control Damage can affect flexibility of thinking, problem solving, attention and memory even following a ‘good’ recovery from a TBI (Stuss et al., 1985) MRI studies identified frontal as most common region of injury following mild to moderate traumatic brain injury (Levin et al., 1987) Area of the brain associated with: ◦ regulating planning behaviour ◦ sensitivity to reward and punishment ◦ ToM ◦ sensory integration ◦ representing the affective value of reinforcers, and decision making & expectation Destruction of the OFC through acquired brain injury typically leads to a pattern of disinhibited behaviour. Bechara et al,1994; Kringelbach, 2005; Schore, 2000; Stone, Baron-Cohen, & Knight, 1998; Snowden et al 2001 Epilepsy Hormonal changes Coma Marital breakdown Loss of self Relating to others Executive functioning (Dysexecutive syndrome) Abnormal cognition and behaviour following the war (Luria, 1966) First documented case Phineas Gage (Harlow, 1848) Costandi, M (2010) Early EF models described it in unitary, homogenous terms with no individual components and generalised to the frontal lobes, “frontal lobe syndrome” (Anderson, Jacobs & Anderson 2008, p. xxviii) Limitations of frontal lobe syndrome (Anderson, Jacobs & Anderson 2008, p. xxviii) EF umbrella term describing a range of highly complex and interrelated group of cognitive phenomena such as: ◦ attention control, inhibition, working memory, goal setting, planning, problem solving, multi tasking and abstract reasoning (Senn, Espy, & Kaufmann, 2004; Welsh, Pennington, & Groisser, 1991) In order to achieve a goal-directed behaviour (Levin & Hanten, 2005; Lezak, 2004). Critique Agreed upon definitions problematic (Anderson, 2008; p. 6) Should be theoretically sound, encompass the various cognitive functions, explain the different presentation of impairments, provide a link between brain and behaviour and be able to suggest assessment methods as well as interventions (Gioia, Guy & Isquith, 2001; p.329). ◦ Self Regulation model; the ability to inhibit behavioural responses (Barkley, 1997) ◦ Developmental model; how EF profile develops in children (Anderson, 2002). (for brief review of prominent EF models see Anderson 2008). Critique - No one model has been uniformally accepted but, current work is evolving at defining an integrated one see Cascadeof control model (Banich, 2009) One leading model that addresses Gioia et al (2001) recommendations is the working memory model of Baddeley and Hitch (1974; see also Baddeley 1997 and 2001); Two discrete functions holding information as the focus of attention and the retrieval of information from long term memory (Spillers, & Unsworth, 2011; p, 1532). Central Executive Visuospatial Sketchpad Episodic buffer Visual Semantics Episodic LTM Phonological loop Language Baddeley’s working memory model (2001) TBI can lead to deficits in executive functioning such as working memory, in particularly the central executive of Baddeleys model, where it is argued that the systems impaired are collective known as Dysexecutive syndrome (DES) (Wilson, Alderman,Burgess, Emslie, and Evans 2003; p. 33) DES is used as umbrella term to describe a pattern of deficits in executive functioning such as planning, abstract thinking and behavioural control (Baddeley 1988; p214) Assessment of these deficits are typically conducted using performance based neuropsychological tests (Gerstadt, Hong, & Diamond,1994) Critique ecological validity of such tests has been questioned because the tests are highly structured, administered in a distraction-free environment, and in some instances, provide cues on how to respond (Goldbery & Podell, 2000) Two test that address these criticism are the Behavioural assessment of the Dysexecutive Syndrome (Wilson, Alderman, Burgess, Emslie, & Evans 1996) Delis–Kaplan Executive Function System both of which use a battery of test to identify specific executive functioning deficits (D-KEFS, Delis, Kaplan & Krammer, 2001) The BADS (1996) is designed to require participants to plan, initiate, monitor and adjust behaviour in response to the explicit and implicit demands of a series of tasks using six test, such as the zoo map which test the ability to plan while following a set of rules. It also contains the 20 item dysexecutive questionnaire which lists statements common problems of everyday life and to rate them according to their personal experience (Wilson, Alderman,Burgess, Emslie, and Evans 2003; p. 33). While the D-KEFS (2001) aims for a similar goal in both children and adults but using nine tests. It is also able to be utilised in different clinical populations from TBI like multiple sclerosis (Parmenter et al, 2007) PSYCHOLOGICAL ISSUES Difficulties with empathy, perspective taking and cognitive flexibility (Grattan, 1994) Theories of interpersonal relationships ◦ Attachment theory ◦ Social exchange theory (Homans, 1958) Human relationships formed by use of cost-benefit analysis & the comparison of alternatives (Although some critique re. basis in economic theory; based on openness which not relevant to all & places relationships in linear structure rather than flexible in path followed – Miller, 2005) ◦ Uncertainty reduction theory (Berger and Calabrese, 1975) Individuals seek to reduce uncertainty with each other when first interacting, based on self-disclosure Critics discuss driving force of interaction is desire of positive relational experiences (e.g. Sunnafrank, 1986) All discuss in some form a sense of giving and receiving of emotional and/or cognitive information ◦ Empathy positively associated with relationship satisfaction, negatively associated with depression and conflict; depression and conflict negatively associated with relationship satisfaction (Cramer, 2010) ◦ Cognitive flexibility positively related to interpersonal effectiveness (Adler, Rosenfold & Proctor, 2007) Neighbours /society Colleagues Extended family Parents Partner Children Friends Employer Healthcare/social professionals Major depressive disorder (MDD) may be the most common and disabling psychiatric condition in individuals with TBI Poorer cognitive functioning, aggression and anxiety, greater functional disability, poorer recovery, higher rates of suicide attempts, and greater health care costs associated with MDD after TBI (Bombardier et al., 2010) Incidence of major depression among 559 people with traumatic brain injury was nearly eight times greater than would be expected in the general population "less than half of the people who were found to have major depression received any treatment during the first year“ (Fann et al., 2010) Treating depression can be effective and can decrease functional impairment, somatic symptoms, and perception of impairment (Varney et al., 1987) Theories of depression Learned helplessness theory: Clinical depression may result from perceived absence of control over a situation’s outcome (Seligman, 1975) When suffering uncontrollable events, can impact on emotions, aggressions, physiology and problem-solving tasks (Roth, 1980) Critique Does not account for varying reactions to same situations (Peterson & Park, 1998) “Coping refers to the persons’ cognitive and behavioural efforts to manage (reduce, minimise, master or tolerate) the internal and external demands of the person-environment transaction that is appraised as taxing or exceeding the person’s resources.” ◦ Folkman, Lazarus, Gruen & DeLongis (1986, pg. 572) Direct result of the structural lesion Psychological reaction to the lesion (Brown et al, 1988) ◦ Somatising Evidence for both Adjustment disorders ◦ Many patients suffer poor psychosocial adjustment and experience a reduced quality of life Wolters et al. (2010) ◦ Effectiveness of psychotherapy and adjustment Ratzel-kurzdorfer, Franke & Wolfersdorf (2003) Strain & Newcorn (2006) Challenging behaviour ◦ Not a diagnostic category ◦ Culturally abnormal behaviour ◦ Risk to self or others & limits access to community services Why the change ◦ ◦ ◦ ◦ ◦ Difficulties communicating needs / understanding incoming information Frustration / memory of previous abilities Attachment Effect of injury / site of injury Environmental factors Critique ◦ Almost all literature is based in learning disabilities ◦ Limited research into prevalence or differences in CB ◦ Aggression / challenging behaviour Baguley et al, 2006; Emerson, 1995; Kelly et al, 2008; Pfafflin & Adshead, 2004; Yody et al, 2000 INTERVENTIONS “challenging behaviours exhibited by those with ABI are significant obstacles to achieving successful rehabilitative outcomes.” “the neurorehabilitation field has been slow to embrace the practice of functional analyses” Rahman, Oliver & Alderman(2010, pg 212 - 13) Rahman et al (2010) 9 ABI survivors with challenging Behaviours method - descriptive functional analysis. Found – all participants exhibited at least one behaviour which was socially reinforced. - Functional analysis was a useful assessment intervention Recommended - Assessment using functional analysis in the field of neurorehabilitation. Critique - There were a variety of injury types and frontal lobe damage was not specified. Clinical interventions based on functional assessments are still limited. (Ager & O’May, 2001) Behavioural treatment models have been successfully applied for ABI (Corrigan & Bach, 2005) Rahman et al (2010) “such behaviours can be decreased and managed by adopting treatment approaches based on operant conditioning.” any combination of 3 reinforcers motivate challenging behaviours (Carr,1977) o Social positive reinforcement. o Social attention, or tangible items /activities given in response to behaviours (Kodak, Northup and Kelley, 2007) o Social-negative reinforcement o Behaviours which serve to remove postpone or reduce aspects e.g not needing to do tasks or engage in social contacts (Iwata, Pace, Kalsher, Cowdery, & Cataldo,1990 ) o Automatic reinforcement o non environmental BUT internal e.g.Pain attenuation (Sandman & Hetrick, 1995) Experimental functional analysis – systematic manipulation of environmental controls to identify which bring about a change in behaviour. (Rahman et al , 2010) Teaching the patient and family to adapt their lifestyle Taking into account the severity of cognitive and behavioural problems Patient being stimulated to learn new skills and compensatory strategies To return to activities of daily life and participate in society ◦ Wilson (2000) Parente (in Shaughnessy & Beyer, 2010) • • • An American approach for working with patients with brain injury, incorporates therapy group and individual work. Focusses on topics identified as problematic by the client and family Examples – Memory training - devices – mobile phones, digital recorders , planners and checklists Disinhibition and hostility – family & patient learning to defuse situations, cue words. Emotional dysregulation & Impulse control – Medication, making client aware of issue, looking at scenarios and possible responses. Awareness of normative social behaviour – teach techniques, pair work, video recordings. Other focusses Loss of hope Co-occuring PTSD Shame and embarrassment (around social behaviour) Local issues – referrals into neuropsychological services Head injury and PTSD? Who treats them? NHS vs private, increasing pressure to meet targets and prove effectiveness in outcome measures, impact on actual treatment received? ◦ Increase in traumatic brain injuries in veterans returning from war America, rehab, v pricey Who provides rehabilitation? NICE guidelines, - Only for Triage, Assessment, Investigation and early management of head injury. Does not address the rehabilitation or long-term care of patients with a head injury (NICE 2007). There was an action plan of services for Acquired brain injury In Northern Ireland in 2009 The plan suggested amongst other suggestions; Making the services more Joined up Standardised care pathway including targets around waiting times improving information around prevalence to plan future service provision Recognising the importance of family support & importance of promoting independence Support education and training of staff . Between 2009/10 and 2011/12 and additional £1.2 million was invested in implementing these changes No equivalent yet in England and Wales British Society of Rehabilitation Medicine - called for a joint framework between employment , social services , and independent/voluntary providers to guide brain injury services (British Society of Rehabilitation Medicine 2008; p. 3) National Audit Office ( 2011)Report Almost £1billion wasted through people with neurological conditions being unnecessarily admitted to hospital. The MS Society, Motor Neurone Disease (MND) Association, Parkinson’s UK Neurological Alliance, Neurological Commissioning Support – urging Government to create a targeted, properly resourced national strategy for neurological conditions which would include acquired brain injury. Communication problems Informed consent Family issues DNA policy – appropriate for FL patients (Spontaneity, impulse control, disinhibited behaviour etc.) Clinical responsibility / Organisational ◦ Which services are best to deal with traumatic brain injury and in particular support with the challenging behaviour? Compensation claims Sexual difficulties – under acknowledged, lack of information Study by Rolls, Honack, Wade and McGrath (1994) Problematic sexual behaviour in patients with FL - sexually explicit language, actual sexual advances being over friendly, kissing and hugging exposure Difficulties for the patient and partner Headway (charity) Patient information leaflets mention sexual difficulties (? Psychological ) – suggests; - sexual counselling from e.g. Relate - a clinical neuropsychologist who specialises in sexual relationships Introduction and definitions ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Brain injury –terms Types of traumatic brain injury Neuroanatomy Frontal lobe – overview Orbitofrontal damage Executive functioning Working memory Baddeley’s working model Deficits in executive functioning Neuropsychological assessments Epidemiology Psychological Issues ◦ ◦ ◦ ◦ ◦ Interpersonal issues Systemic issues Emotional impact incl. theories of depression Adjustment Behavioural difficulties Interventions ◦ ◦ ◦ ◦ • • Functional analysis Behavioural approaches Aims of cognitive rehabilitation Organisational issues National policy & guidance Ethical issues Think about the experience and knowledge you have of working with services offering neuropsychological assessment, formulation and intervention Imagine you are a qualified psychologist working in this field. Based on the above, complete a SWOT (Strengths, Weaknesses, Opportunities and Threats) analysis of factors you think are likely to be experienced by psychologists in this area Additional areas for consideration: Political Economic Social Technological Legal Environment Questions Adler, R.B., Rosenfold, L.B. & Proctor, R.F. (2007) Interplay: The process of interpersonal communication, 10th Ed., Oxford University Press: New York. Ager, A., & O’May, F. (2001). Issues in the definition and implementation of “best practice” for staff delivery of interventions for challenging behaviour. Journal of Intellectual & Developmental Disability, 26, 243–256. Anderson, P. (2002). Assessment and development of executive function (EF) during childhood. Child Neuropsychology, 8(2), 71-82. Anderson P.J. (2008). Models of executive function. In V Anderson, Jacobs R, Anderson PJ. Executive functions and the frontal lobes: A lifespan perspective. New York: Taylor & Francis. pp. 3–21. Baddeley, A. (1997). Human Memory: Theory and practice, revised edn, Psychology Press: Hove. Baddeley A.D. (2002) Is working memory still working? American Psychologist; 56 (11), 851-864. Baddeley, A. D., & Hitch, G. (1974). Working memory. In G. H. Bower (Ed.), Recent advances in learning and motivation (Vol. 8, pp. 47–90). New York: Academic Press. Baddeley, A., & Wilson, B. (1988). Frontal amnesia and the dysexecutive syndrome. Brain and Cognition, 7, 212-230 Banich, M.T. (2009). Executive function the search for an integrated account. Current directions in Psychological Science18, (2), 89-94. Barkley, R.A. Behavioural inhibition, sustained attention, and executive functions: Constructing a theory of ADHD. Psychological Bulletin, 121, (1), 65-94. Bechara, A., Damasio, A.R., Damasio H., & Anderson, S.W. (1994) "Insensitivity to future consequences following damage to prefrontal cortex". Cognition 50: 7-15. human Bombardier, C. .H., Fann, J. R., Temkin, N. .R., Esselman, P. C., Barber, J. & Dikmen, S. S. (2010). Rates of Major Depressive Disorder and Clinical Outcomes Following Traumatic Brain Injury. JAMA, 303 (19): 1938-1945. Brain Injury network, (2012 ) who are we , retrieved from http://www.braininjurynetwork.org/aboutbin.html on 13/01/2012 British Society for Rehabilitation Medicine (2008). Vocational assessment and rehabilitation after acquired brain injury inter-agency guidelines. Retrieved from http://bookshop.rcplondon.ac.uk/contents/fbc3513a-5642-459a-9b2c-a1e47e8745ad.pdf Costandi, M. (2010, November 8). Phineas Gage and the effect of an iron bar through the head on personality. The Guardian. Retrieved from http://www.guardian.co.uk/science/blog/2010/nov/05/phineas-gage-head-personality Davey, G. (2008) Psychopathology Research, Assessment and Treatment In Clinical Psychology. West Sussex: Wiley-Blackwell. Delis, D. C., Kaplan, E., & Kramer, J. (2001). Delis–Kaplan Executive Function System. San Antonio, TX: Psychological Corporation. Folkman, S. Lazarus, R. S., Gruen, R. J. & DeLongis, A. (1986) Appraisal, coping, health status and psychological symptoms Journal of Personality and Social Psychology, 50, 571-579. Fann JR, Katon WJ, Uomoto JM. (1995) Psychiatric disorders and functional disability in outpatients with traumatic brain injuries. Am J Psychiatry, 152:1493-1499. Gerstadt, C. L., Hong, Y. J., & Diamond, A. (1994). The relationship between cognition and action: Performance of children 3[1/2]–7 years old on Stroop-like day–night test. Cognition, 53, 129–153. Goldberg, E., & Podell, L. (2000). Adaptive decision making, ecological validity, and the frontal lobes. Journal of Clinical and Experimental Neuropsychology, 22, 56–68. Gioia, G.A., Guy, S.C., Isquith, P.K. (2001), Assessment of Executive Functions in Children with Neurologic Impairment. In G.A. Gioia, S.C. Guy, & P.K. Isquith (Eds.), Psychological and Development Assessment, (pp. 317-356). New York, NY: Guilford Press. Guess, D., & Carr, E. (1991). Emergence and maintenance of stereotypy and self-injury.American Journal on Mental Retardation, 96, 299– 319. Headway (2012) sex and sexuality after brain injury, retrieved from http://www.headway.org.uk/sex-and-sexuality-after-brain-injury.aspx on 13/01/2012 Harlow, J. (1848). The passage of an iron rod through the head. Boston medical and surgical journal, 39, 389-393. Retrieved from http://books.google.co.uk/books?vid=HARVARD:32044089567515&printsec=titlepage&redir_esc=y#v=onepage&q&f=false Hospital Episode statistics 2000 – 2001 retrieved from http://www.patient.co.uk/doctor/Head-Injury.htm#ref1 , January 2012 Kringelbach, M.L. (2005) The orbitofrontal cortex: linking reward to hedonic experience. Nature Reviews Neuroscience 6: 691-702. Iwata, B. A., Pace, G. M., Kalsher, M. J., Cowdery, G. E., & Cataldo, M. F. (1990). Experimental analysis and extinction of self-injurious escape behavior. Journal of Applied Behavior Analysis, 23, 11–27. Kodak, T., Northup, J., & Kelley, M. E. (2007). An evaluation of the types of attention that maintain problem behavior. Journal of Applied Behavior Analysis, 40, 167–171. Kolb, B., & Milner, B. (1981). Performance of complex arm and facial movements after focal brain lesions. Neuropsychologia, 19:505-514. Lovaas, I., Newsom, C., & Hickman, C. (1987). Self–stimulatory behavior and perceptual reinforcement. Journal of Applied Behavior Analysis, 20, 45–68. Carr, E. G. (1977). Motivation of self-injurious behavior: A review of some hypotheses. Psychological Bulletin, 84, 800–816. Levin et al. (1987). Magnetic resonance imaging and computerized tomography in relation to the neurobehavioral sequelae of mild and moderate head injuries. Journal of Neurosurgery, 66, 706-713. Levin, H.S., Culhane, K.A., Hartmann, J., Evankovich, K., Mattson, A.J., Howard, H., et al. (1991). Developmental changes in performance on tests of purported frontal lobe functioning. Developmental Neuropsychology, 7(3), 377-395. Lezak, M.D. (2004). Neuropsychological Assessment. New York: Oxford University Press. Luria, A.R. (1966). Higher cortical functions in man. New York: Basic Books. National Audit Office (December 2011) services for people with neurological conditions, The stationary office: London. National Institute of Neurological disorders and stroke (2012 ) Traumatic Brain Injury Information Page retrieved from http://www.ninds.nih.gov/disorders/tbi/tbi.htm on 13/01/12 Parementer, B.A., Zivadinov, R., Kerenyi, L., Gavett, R., Weinstock-Guttman, B., Dwyer, M.G., Garg, N., Munchauer, F., & Benedict, R. (2007). Validity of the Wisconsin Card sorting and Delis –Kaplan Executive functioning system (D-KEFS) sorting tests in multiple sclerosis. Journal of Clinical Experimental Neuropsychology, 29, (2), 215-223. Rahman,B., Oliver,C.& Alderman,N.(2010) Descriptive analysis of challenging behaviours shown by adults with acquired brain injury. Rehabilitation,20 (2), 212–238 Neuropsychological Repp, A. C., Felce, D., & Barton, L. E. (1988). Basing the treatment of stereotypic and selfinjurious behaviors on hypotheses of their causes. Journal of Applied Behavior Analysis, 21, 281–289. Sandman, C. A., & Hetrick, W. P. (1995). Opiate mechanisms in self-injury. Mental Retardation and Developmental Disabilities Research Reviews, 1, 130–136. Senn, T. E., Espy, K. A., & Kaufmann, P. M. (2004). Using path analysis to understand executive function organisation in preschool children. Developmental Neuropsychology, 26, 445–464. Shaughnessy,M.F.& Beyer,J.(2010) An interview with Rick Parente:head injury and brain trauma, N.American journal of psychology, Vol.12, No 2, 221-232. Schore A.N., (2000) Attachment & the Regulation of the Right BrainAttachment & human Development 2(1) 23-47. Snowden, J. S.; Bathgate, D.; Varma, A.; Blackshaw, A.; Gibbons, Z. C. & Neary. D. (2001) Distinct behavioural profiles in frontotemporal dementia and semantic dementia. Journal of Neurological Neurosurgical Psychiatry 70: 323-332. Spillers, G.J., & N. Unsworth. (2011). Variation in Working Memory Capacity and Temporal–Contextual Retrieval From Episodic Memory. Journal of experimental psychology: Learning, Memory and Cognition, 37, (6), 1532-1539. DOI: 10.1037/a0024852 Stone, V.E.; Baron-Cohen, S. & Knight, R. T. (1998a) "Frontal Lobe Contributions to Theory of Mind." Journal of Medical Investigation 10: 640-656. Stuss, D. et al. (1985). Subtle neuropsychological deficits in patients with good recovery after closed head injury. Neurosurgery, 17, 41-47. Wilson, B. A., Alderman, N., Burgess, P. W., Emslie, H., & Evans, J. J. (1996). Behavioural Assessment of the Dysexecutive Syndrome. London: Harcourt Assessment. Wilson, B.A., Alderman, N., Burgess, P.W., Emslie, H., and Evans J.J. (2003). Behavioural assessment of the Dysexecutive Syndrome (BADS). Journal of Occupational Psychology Employment and Disability, 5 (2), 33-37. Wolters, G., Stapert, S., Brands, I. & Van Heugten, C. (2010) Coping styles in relation to cognitive rehabilitation and quality of life after brain injury. Neuropsychological Rehabilitation 20(4), 587- 600. World health organisation (1996) Geneva Varney, N.R, Martzke, J.S, & Roberts R.J. (1987) Major depression in patients with closed head injury. Neuropsychology, 1(7), 9. Brain Injury Association of America National Institute of Neurological Disorders and Stroke (NINDS) Brain Injury Association of Canada Brain Injury Association of Queensland Australia Headway - the brain injury association Ontario Shores Centre for Mental Health Sciences Ontario Brain Injury Association NICE guidelines, but only for Triage, assessment, investigation and early management of head injury in infants, children and adults Head injury (CG56 It does not address the rehabilitation or long-term care of patients with a head injury http://www.nice.org.uk/nicemedia/live/11836/36260/36260.pdf Rehabilitation following acquired brain injury National clinical guidelines - by Royal College of physicians http://bookshop.rcplondon.ac.uk/contents/43986815-4109-4d28-8ce5-ad647dbdbd38.pdf ◦ Included recommendation for clinical psychology provision! per 500000 of population (pg18) More British ones – found at Headway http://www.headway.org.uk/home.aspx