Supplementary material Supplementary material 1 –samples and
advertisement

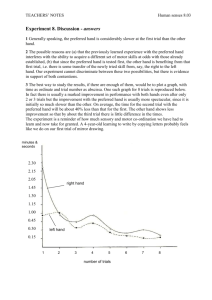
Supplementary material Supplementary material 1 –samples and methods Details of samples Group I. Operated patients. Twenty-two Parkinson’s disease patients (17 male, 21 right handed) aged between 35 and 67 (M = 52.09, SD = 8.4) received unilateral subthalamotomy (10 right and 12 left subthalamotomy) following procedures described in Alvarez et al., (2001). They were all assessed after an interval of 2 to 8 months (M = 4.47, SD = 1.5) after surgery, which was not significantly different for those with right or left subthalamotomies (p > 0.05). Group II. Unoperated patients. Fourteen unoperated Parkinson’s disease patients (9 male, 10 right handed) aged between 46 and 68 (M = 58.74, SD = 5.1), who were also potential candidates for surgery, served as patient controls. The operated and unoperated patients had similar demographic characteristics, degree of disease evolution and severity (see Table 1). Twenty-three healthy participants (11 male, 19 right handed) aged between 45 and 67 (M = 55.00, SD = 6.1) were assessed as controls. The healthy control group was assessed at UCL Institute of Neurology, UK, by the same investigator (IO) who undertook patient assessments in Havana. None of the controls had any neurological disorder or history of psychiatric illness, head injury, drug or alcohol abuse. The study was approved by The National Hospital for Neurology and Neurosurgery and Institute of Neurology Joint Research Ethics Committee as well as the Cuban National Ethical Committee. Informed consent was obtained prior to participation in the study. Clinical evaluation The clinical criteria and evaluations have been described previously in detail (Alvarez et al., 2001;Alvarez et al., 2005;Alvarez et al., 2009). All patients met the UK Brain Bank diagnostic criteria 1 (Hughes et al., 1992), showed an adequate dopaminergic response, and absence of atypical features. All patients were non-demented, as revealed by scores above 26 on the Mini-Mental State Examination (Folstein et al., 1975). Patients were screened for clinical depression (scores > 18) on the Beck Depression Inventory (Beck et al., 1961). Patients were taking their normal medication with levodopa + benserazide and dopamine agonists during the current assessments. The Unified Parkinson’s Disease Rating Scale-III was used for evaluation in the “on” and “off” medication states. Surgery The surgical technique has also been described previously (Alvarez et al., 2001). In brief, a unilateral lesion of the STN was performed under local anaesthesia on the hemisphere contralateral to the most-affected side of the body. Coordinates chosen for targeting the STN were 2–3 mm behind the middle inter-commissural point (Y coordinate), 12 mm lateral (X coordinate), and 5–6 mm (Z coordinate) below the ACPC line. To induce the lesion, a thermolytic lesion (60°C for periods of 30 seconds) of 4 mm in diameter was produced with a needle of 1.1 mm diameter and a 3-mm tip (Elektra Instruments AB, Sweden). Post-surgical MRI confirmed correct lesion placement over the dorsolateral section of the STN in all patients (see Figure S1). 2 Figure S1. Axial and sagittal view for two operated Parkinson’s disease (PD) patients with left (axial) and right (sagital) STN lesions. Conditional stop signal task A series of interleaved Go and Stop trials was presented. Go trials consisted of a left (or right) pointing green arrow and participants were asked to respond as fast as possible using their index and middle fingers of one hand to press left or right keys. For each participant either the left or right pointing arrows were designated as the ‘critical’ direction. When a stop signal was presented following an arrow/go signal in the ‘critical’ direction, participants had to stop their response. In contrast, when a stop signal was presented following an arrow/go signal in the ‘non-critical’ direction, participants were instructed to ignore the stop signal and respond to the ‘non-critical’ go signal. A Go trial began with a black fixation circle located in the centre of a gray background of the computer screen. After a 500 ms interval, the fixation circle was replaced by presentation of a green arrow in the center of the screen for a maximum of two seconds (limited hold), followed by the background screen during the variable (0.5 to 4 second) null period until the next trial. If a participant responded within the limited hold period, the arrow disappeared, leaving the background screen and the null period. Participants responded with their index finger to left arrows and their middle finger to the right arrows. The number of left and right pointing arrows was equal. The ‘critical’ direction was 3 the left pointing arrow for 5/10 patients in the group with right subthalamotomy, 6/12 patients in the group with left subthalamotomy, 6/14 of unoperated patients and 15/23 of healthy controls. A Stop signal was presented on 25% of all trials. Half of the Stop signals were presented after a Go signal in the ‘critical’ direction, and participants had to stop their response. On Stop trials, after a variable stop signal delay, the green arrows were replaced by a red cross. If a participant’s response was successfully inhibited during a stop signal trial, the red cross stayed on the screen throughout the limited hold. However, if a participant responded within the limited hold period, the arrow disappeared, leaving the background screen and the null period. The stop signal delay value for the Stop trials changed dynamically during the task on the basis of each individual’s behaviour, based on four staircases. If successful inhibition was achieved, the stop signal delay was increased by 50 ms on the next Stop trial, which made inhibition more difficult. If the response was not successfully inhibited, the stop signal delay was reduced by 50 ms, which made it easier to achieve inhibition. The reason for the staircases of four step-up and step-down algorithms was to ensure convergence to probability of inhibition [P(inhibit)] of 50% by the end of the three blocks. Initially, the four stop signal delay staircases started with values of 100, 150, 200, and 250 ms, respectively. A block of trials consisted of 96 Go trials and 32 Stop trials, where 16 Stop trials were in the ‘critical’ direction and 16 Stop trials were in the ‘non-critical’ direction. Therefore, each staircase (100, 150, 200, and 250 ms) moved four times within each block for the Stop trials of the ‘critical’ direction. The staircases were independent but were randomly alternated. Stop signal delays for Stop trials in the ‘non-critical’ direction were yoked to the ‘critical’ direction values. Participants were instructed to respond to the green arrows by pressing the correct response key as fast and as accurately as possible. In the ‘critical’ direction, it was also important to stop their response to the green arrow when it was followed by a red cross. Participants were also informed that it would not always be possible to stop their response on ‘critical’ stop trials. In addition, in the ‘noncritical’ direction when a green arrow was followed by a stop signal presentation, participants were 4 instructed to ignore this stop signal and continue responding as fast and accurately as possible. Finally, participants were specifically instructed not to try to delay their performance on the Go task in order to improve their chances of stopping after green arrows in the ‘critical’ direction. Following these instructions, 20 practice trials were completed. Each block was preceded by an instruction screen and was followed by performance feedback with mean correct reaction time and the number of discrimination errors on the Go trials. Several measures were obtained (see Tables 2 and S1): mean Go reaction times for both ‘critical’ and ‘non-critical’ trials, percentage of Stop trials with successful inhibition (Stop Inhibit) for the ‘critical’ direction, number of Stop trials resulting in erroneous inhibition for the ‘non-critical’ direction, mean reaction time on Stop trials without successful inhibition in the ‘critical’ direction (‘critical’ StopRespond reaction times) and reaction times on ‘non-critical’ trials with a stop signal (‘non-critical’ StopRespond reaction times). In addition, we obtained a measure of conflict resolution, conflict-induced slowing obtained by subtracting ‘non-critical’ Go from ‘non-critical’ StopRespond reaction times. The measure of proactive action restraint, the response delay effect was calculated by subtracting ‘non-critical’ Go from ‘critical’ Go reaction times. To detect violations of independence in the ‘horse race’ model, we examined the patient’s individual data block by block (Verbruggen et al., 2013). Blocks where ‘critical’ StopRespond reaction times (failed inhibition on stop trials) were not faster than ‘critical’ Go reaction times were removed from the analysis. This cleaning of data is recommended when the race model is likely to be violated because of clinical conditions (Verbruggen et al., 2013). In the unoperated group, 7/14 (50%) patients showed responses with model violation (i.e. ‘critical’ StopRespond > ‘critical’ Go reaction times) and in the operated group, 4/10 (40%) from the right and 5/12 (42%) from the left subthalamotomy groups. These blocks were removed from the analysis. The stop signal reaction time (SSRT) was computed using the integration method, estimated independently for each block (Verbruggen et al., 2013). We first rank ordered the correct ‘critical’ Go 5 reaction times. For each participant, the nth Go reaction time value was obtained by multiplying the total number of ‘critical’ Go trials by the probability of responding on stop trials. The mean stop signal delay (averaged from the mean values for the last six moves in each of the four staircases when the participant had converged on 50% inhibition) was subtracted from the nth Go reaction time value to compute the SSRTs. Supplementary material 2 – comparison of groups on demographic and clinical variables Clinical and demographic differences between the groups were examined by completing oneway ANOVAs on each demographic (age, years of education) or clinical (Beck Depression Inventory, Mini-Mental State Examination, disease duration, medication dose, time since surgery) variables. No significant differences in age [F(3,58) = 1.48, p = .14], or Beck Depression Inventory [F(3,58) = 1.86, p = .15] were found between the four groups. A chi-square test was used to examine sex distributions across the groups and no significant differences were found [X2 = 2.77, p = .10]. The results showed significant differences in education [F(3,58) = 6.70, p < .001] and Mini-Mental State Examination scores [F(3,58) = 4.35, p < .01] between the four groups. Patients with right subthalamotomy did not differ significantly from the group with left subthalamotomy or the unoperated patients in terms of years of education [left subthalamotomy: t(20) = -1.62, p = .12; unoperated: t(22) = -.28, p = .77] or Mini-Mental scores [left subthalamotomy: t(20) = .28, p = .77; unoperated: t(22) = .21, p = .83]. However, relative to controls, patients with right subthalamotomy had significantly lower education [t(31) = -3.66, p = .001] and Mini-Mental scores [t(31) = -2.76, p = .01]. Patients with left subthalamotomy did not differ from the unoperated patients or controls in terms of years of education [unoperated: t(24) = -1.42, p = .16; controls: t(33) = - 1.90, p = .07], whereas their Mini-Mental scores were equivalent to those of the unoperated: [t(24) = -.83, p = .41], but significantly lower than the controls [t(33) = -2.83, p < .01]. Finally, unoperated patients had significantly less years of education [t(35) = -3.54, p = .001] and lower 6 Mini-Mental scores [t(35) = -4.73, p < .001] than controls. As a result, Mini-Mental and education were used as covariates in all analyses. Surgery was uneventful in all cases and there were no major adverse effects at follow-up for any of the operated patients. Post-surgical MRI showed that lesions were mostly placed in the dorsolateral region of the STN (see example Figure S1). As expected, a significant difference in motor score (Unified Parkinson’s Disease Rating Scale-III: [F(3,35) = 14.36, p < .001]) and medication dose [F(3,35) = 4.74, p = .01] was found between the two operated and the unoperated patients groups; but the groups did not differ in disease duration [F(3,35) = 1.03, p = .37]. Patients with right or left subthalamotomy did not differ in terms of time since surgery [t(22) = - .37, p = .71]. The two operated groups did not differ in terms of post-operative motor score [t(22) = - 1.75, p = .11] or medication dose [t(22) = 1.35, p = .19]. Therefore, unilateral right or left subthalamotomy significantly improved Parkinson’s disease motor signs as measured on the Unified Parkinson’s Disease Rating Scale-III, and post-operatively the operated patients had significantly lower motor scores and medication doses than unoperated patients. No differences in motor scores were found between patients with right or left subthalamotomy after surgery. Patients with right subthalamotomy had similar pre-operative motor scores [t(22) = -1.08, p = .29], but significantly lower post-operative motor scores [t(22) = -4.75, p < .001] than unoperated patients. Similarly, the right subthalamotomy group did not differ from the unoperated patients in medication dose [t(22) = 1.31, p = .16] before surgery, but had significantly lower doses than the unoperated patients [t(22) = 2.31, p = .04] post-operatively. Compared to unoperated patients, patients with left subthalamotomy had significantly higher pre-operative motor scores [t(24) = 2.87, p = .01] and significantly lower post-operative motor scores [t(24) = -3.28, p = .006] and numerically, but not significantly lower medication levels before surgery [t(24) = 0.44, p = .67] which then became significantly lower after surgery [t(24) = -3.06, p = .008]. 7 To establish the effect of surgery on motor symptoms, a 3-way ANOVA with Time of assessment (pre vs. post surgery), Lesion side (right vs. left subthalamotomy) and Medication state (on vs. off medication) was completed on the motor scores for operated patients. Significant main effects of Time [F(1,21) = 15.86, p < .01], Medication [F(1,21) = 35.48, p < .001] and a significant Time x Medication interaction [F(1,21) = 6.01, p = .04] were obtained. Patients had significantly lower motor scores after surgery both on [right subthalamotomy t(9) = 3.62, p = .02; left subthalamotomy t(11) = 3.92, p = .03] and off medication [right subthalamotomy t(9) = 3.56, p = .01; left subthalamotomy t(11) = 4.02, p = .04]. Patients with right subthalamotomy had significantly lower motor scores while on medication than the left subthalamotomy group after surgery [t(21) = -2.36, p = .04], but not significantly so off medication [t(11) = -1.75, p = .11]. A 2-way ANOVA with Time of assessment and Lesion side was completed on medication dose scores for the operated patients. Significant main effects of Time [F(1,21) = 10.94, p = .01] and Lesion side [F(1,21) = 6.43, p = .03] were obtained. The Time x Lesion side interaction was not significant [F(1,21) = .93, p = .36]. Patients with right subthalamotomy had significantly lower medication doses after surgery [t(9) = 2.69, p = .05], similarly for those with left subthalamotomy [t(11) = 2.73, p = .01]. Patients with right subthalamotomy had significantly higher doses compared to those with left subthalamotomy before surgery [right subthalamotomy, M = 1379.60, SD = 266.0; left subthalamotomy, M = 924.00, SD = 277.1; t(20) = 2.65, p = .02] but the dose for the two groups was not significantly different after surgery [right subthalamotomy, M = 450.0, SD = 243.9; left subthalamotomy, M = 368.33, SD = 208.4; t(20) = 1.31, p = .20]. Supplementary material 3- results Effect of subthalamotomy on performance of the stop signal task with the ipsi-lesional hand The data for each of the measures on the stop signal task are presented in Table S1, for the hand ipsilateral to subthalamotomy for operated patients and the non-dominant hands for unoperated 8 patients and controls. Here, we report the results using one-way ANOVAs to compare performance of the ipsi-lesional hand for operated patients with the non-dominant hand of unoperated patients and healthy controls for each measure. A one-way ANOVA on stop signal delay showed a significant effect of Group [F(3,59) = 3.55, p = .02]. Post-hoc comparisons showed the group with right subthalamotomy had non-significantly shorter/worse stop signal delay compared to unoperated patients [t(23) = 1.80, p = .08] and controls [t(31) = 1.33, p = .19]. Mean stop signal delays were significantly shorter/worse for the right compared to left subthalamotomy group [t(20) = 2.97, p < .01]. Mean stop signal delays of the left subthalamotomy patients did not differ significantly from those of controls [t(31) = - .79, p = .43] or unoperated patients [t(25) = - .28, p = .77]. Mean stop signal delay for unoperated patients did not differ significantly from controls [t(39) = 1.31, p = .19] (see Table S1). Table S1. Performance measures on the Conditional Stop Signal reaction time task for the patients with Parkinson’s disease with right or left subthalamotomy, unoperated patients and healthy controls. Standard deviations are given in brackets. Right Trial Description ‘Critical’ direction RT to go stimulus Go Left Unoperated Measure Controls subthalamotomy subthalamotomy ipsilesion ipsilesion patients non- non- dominant dominant 553.22 574.90 636.65 497.31 (101.8) (107.2) (93.8) (87.6) 50% 56% 53% 52% in ‘critical’ direction % correct StopInhibit inhibition 9 RT on failure to 507.41 522.32 594.87 457.84 stop trials (84.9) (101.1) (101.1) (73.8) Number of 2.50 3.16 7.00 .40 omissions (4.3) (3.4) (9.1) (.8) Delay between Go 118.71 231.44 244.38 213.81 and Stop signals (81.0) (94.4) (122.0) (92.5) 386.96 231.44 372.74 257.41 (109.1) (94.4) (121.3) (60.6) 487.52 508.46 596.22 436.08 (79.4) (91.5) (114.1) (45.5) % incorrect 10.80 5.50 9.18 2.72 Inhibition (7.0) (6.1) (8.5) (4.0) 624.33 617.14 793.91 555.17 (130.0) (123.1) (109.7) (74.2) Number of 1.60 2.7 7.09 .22 omissions (7.0) (4.5) (12.2) (.5) StopRespond Go errors § Stop signal delay SSRT RT ‘Non-critical’ direction RT to go stimulus Go in ‘non-critical’ direction StopInhibit RT on trials with StopRespond ‘to be ignored’ stop signal Go errors § ‘Non-critical’ Conflict-induced Stop Respond RT 136.80 108.68 197.69 119.09 slowing minus non-critical (97.0) (71.5) (81.6) (54.9) Go RT Other variables 10 Go discrimination 12.30 17.66 5.45 .22 (14.5) (17.9) (8.6) (.6) 65.69 66.44 40.43 61.23 (61.2) (36.5) (49.5) (60.3) Number of errors errors § Response delay ‘Critical’ Go RT minus ‘non- effect critical’ Go RT RT: reaction times; Stop signal delay: the average stop-signal delay, computed from four staircases (see Methods) at the point at which p(inhibit) =50%. SSRT: is computed for each patient by subtracting the mean SSD from the mean critical Go reaction times. Go omission errors: failure to respond on a go trial. Go discrimination errors: pressing the response key in the opposite direction indicated by the stimulus. ‘Critical’ direction and reactive inhibition For ‘critical’ Go reaction times, the main effect of Group was significant [F(3,59) = 5.46, p < .01]. Post-hoc comparisons revealed that ‘critical’ Go reaction times were faster for patients with right subthalamotomy than unoperated patients, a difference which approached significance [t(22) = - 1.95, p = .06]. ‘Critical’ Go reaction times of unoperated patients were significantly slower than controls [t(35) = 4.20, p < .001]. No differences in ‘critical’ Go reaction times were found between right and left subthalamotomy patients [t(20) = .48, p = .63], or right subthalamotomy patients compared to controls [t(31) = 1.59, p = .12]. ‘Critical’ Go reaction times of the left subthalamotomy group did not differ from unoperated patients [t(24) = - 1.46, p = .15], and controls [t(35) = 1.79, p = .10], the latter did not survive correction for multiple comparisons due to the complexity of the four group design. For ‘critical’ StopRespond reaction times, the main effect of Group was significant [F(3,59) = 6.06, p = .001]. Post-hoc comparisons revealed significantly slower ‘critical’ StopRespond reaction times for unoperated patients than controls [t(35) = 4.43, p < .001]. ‘Critical’ StopRespond reaction times for patients with right subthalamotomy were non-significantly faster than unoperated patients 11 [t(22) = 1.39, p = .16] (did not survive correction for multiple comparisons due to the complexity of the four group design). None of the other group comparisons were significant (left x right subthalamotomy [t(20) = - .37, p = .71], right subthalamotomy x controls [t(31) = 1.68, p = .10]; left subthalamotomy x unoperated patients [t(24) = 1.71, p = .10]; left subthalamotomy x controls [t(35) = 1.90, p = .07, did not survive correction for multiple comparisons due to the complexity of the four group design]). A significant main effect of Group in the SSRT results was observed [F(3,59) = 9.09, p < .001]. Post-hoc comparisons showed SSRTs of right subthalamotomy patients were significantly longer compared to those with left-sided operation [t(20) = 3.58, p < .01]. In addition, patients with right subthalamotomy showed significantly longer SSRTs compared to controls [t(31) = 4.33, p < .001], but did not differ from the unoperated group [t(22) = - .28, p = .78]. Patients with left subthalamotomy had significantly faster SSRTs than unoperated patients [t(24) = 3.13, p < .01], but did not differ from controls [t(35) = .97, p = .33]. Unoperated patients were significantly slower than controls [t(35) = 3.67, p = .001]. ‘Non-critical’ direction and conflict-induced slowing For ‘non-critical’ Go reaction times, the main effect of Group was significant [F(3,59) = 10.09, p < .001]. Post-hoc comparisons revealed that right and left subthalamotomy groups did not differ [t(20) = - .56, p = .57]. ‘Non-critical’ Go reaction times for the group with right subthalamotomy did not differ from those of the unoperated patients [t(22) = - 1.56, p = .13]. Patients with right subthalamotomy had significantly slower ‘non-critical’ Go reaction times than controls [t(31) = 2.33, p = .02]. Unoperated patients were significantly slower than controls [t(35) = - 5.79, p < .001]. ‘Noncritical’ Go’s reaction times of patients with left subthalamotomy were marginally significant faster than unoperated patients [t(24) = -2.04, p = .054] and significantly slower compared to controls [t(35) = 3.09, p < .01]. 12 For the ‘non-critical’ StopRespond reaction times, the main effect of Group was significant [F(3,59) = 12.88, p < .001]. Post-hoc comparisons revealed the two operated groups did not differ significantly [t(20) = .13, p = .89]. Patients with right subthalamotomy did not differ from controls in ‘non-critical’ StopRespond reaction times [t(31) = 1.91, p = .06] but were significantly faster than unoperated patients [t(22) = -3.24, p < .01]. The group with left subthalamotomy had significantly faster ‘non-critical’ StopRespond reaction times compared to unoperated patients [t(24) = 3.62, p < .01], but the difference from controls only approached significance [t(35) = 1.90, p = .06]. Unoperated patients had significantly slower ‘non-critical’ StopRespond reaction times than controls [t(35) = 7.40, p < .001]. For conflict-induced slowing, the main effect of Group was significant [F(3,59) = 3.57, p = .02]. No differences in conflict-induced slowing were found between the two operated groups [t(20) = .78, p = .44]. Conflict-induced slowing for the right subthalamotomy group did not differ from that of the unoperated patients [t(22) = 1.56, p = .13] and controls [t(31) = .66, p = .51]. However, patients with left subthalamotomy had significantly less conflict-induced slowing compared to unoperated patients [t(24) = 2.78, p = .01] but did not differ from controls [t(35) = - .47, p = .63]. Unoperated patients had significantly more conflict-induced slowing than controls [t(35) = 3.28, p < .01]. For the response delay effect, the main effect of Group [F(3,59) = .57, p = .63] was not significant, suggesting no differences using ipsi-lesional/non-dominant hand between groups. Omission and discrimination errors The error data are presented in Table S1. A series of Kruskal-Wallis tests were completed to compare ‘critical’ Go omissions, ‘non-critical’ Go omissions and discrimination errors between the four groups when performing the task with the ipsi-lesional or non-dominant hands. 13 A significant difference was found between the groups for ‘critical’ Go omission errors [X2 = 17.10, p < .001], ‘non-critical’ Go omission errors [X2 = 11.53, p < .01], and discrimination errors [X2 = 28.04, p < .001]. To ascertain the direction of the above differences between the groups, post-hoc comparisons with Mann-Whitney tests were completed. For ‘critical’ Go omission errors, significantly more errors were made by unoperated patients compared to controls [U = 37.00, p = .001] but the differences were not significant compared to patients with right [U = 33.50, p = .14] or left subthamotomy [U = 59.00, p = .73]. The two operated groups did not differ in ‘critical’ Go omission errors [U = 37.50, p = .13]. Patients with right subthalamotomy made non-significantly more ‘critical’ Go omission errors compared to controls [U = 68.50, p = .06], while those with left subthalamotomy made significantly more ‘critical’ Go omission errors compared to controls [U = 37.50, p < .001]. For ‘non-critical’ omission errors, significantly more errors were made by unoperated patients compared to controls [U = 51.00, p < .01] and also compared to patients with right [U = 27.00, p = .03] but not left subthalamotomy [U = 53.00, p = .46]. The two operated groups showed no significant differences [U = 38.00, p = .10]. Operated patients made more ‘critical’ omission errors than controls, a difference which was significant for those with left subthalamotomy [U = 78.00, p = .04], but not patients with right subthalamotomy [U = 112.00, p = .86]. Significantly more discrimination errors were made by the unoperated patients compared to controls [U = 58.50, p < .01]. In turn, although approaching significance, unoperated patients committed less discrimination errors compared to right [U = 27.50, p = .052] or left subthalamotomy groups [U = 31.00, p = .06; did not survive correction for multiple comparisons due to the complexity of the four group design]. The two operated groups did not differ in discrimination errors [U = 55.00, p = .77]. Both right and left subthalamotomy groups made significantly more errors compared to controls [right: U = 15.50, p < .001; left: U = 18.00, p < .001]. Therefore, an ipsi-lesional effect on discrimination errors was also present after surgery for both operated groups. 14 Supplementary material 4- results Effect of subthalamotomy on performance of the stop signal task with the contra-lesional hand Mean stop signal delays of the left subthalamotomy group compared to unoperated patients [t(25) = .32, p = .75] and controls [t(31) = -.48, p = .62] were not significantly different. There were no significant differences in mean stop signal delay between left and right subthalamotomy groups [t(20) = 1.72, p = .10]. Stop signal delays of unoperated patients did not differ from controls [t(39) = .97, p = .33] (Table 1). ‘Critical’ Go and StopRespond reaction times For ‘critical’ Go reaction times no differences between patients with right or left subthalamotomy [t(20) = -.66, p = .51] were found as well as between patients with right [t(31) = .18, p = .85] or left subthalamotomy from controls [t(35) = .98, p = .33]. For ‘critical’ StopRespond reaction times (failed inhibition on stop trials), the main effect of Group was significant [F(3,59) = 4.07, p = .01] (Table 2 and Figure S2). Post-hoc comparisons showed no significant differences between right and left subthalamotomy patients [t(20) = - .01, p = .99] and also non-significant differences in the remaining comparisons (right subthalamotomy vs. unoperated patients: t(22) = 1.78, p =.09; left subthalamotomy vs. unoperated patients: t(24) = 1.93, p = .06; right subthalamotomy vs. controls: t(31) = .95, p = .34; left subthalamotomy vs. controls: t(35) = - 1.05, p = .29). However, ‘critical’ StopRespond reaction times for unoperated patients were significantly slower than controls [t(35) = 3.60, p = .001]. In line with the race model, patients with left [t(11) = 3.77, p = .003] and right subthalamotomy [t(9) = 5.12, p = .001], similar to unoperated patients [t(13) = 3.64, p = .004] and controls [t(22) = 6.17, p < .001], had significantly faster ‘critical’ StopRespond than their ‘critical’ Go reaction times. 15 Figure S2. ‘Critical’ StopRespond reaction times for operated Parkinson’s disease (PD) patients with right (R STN) or left (L STN) subthalamotomy, unoperated PD patients and control participants. The figure shows reaction times for the contra-lesional (operated patients) or dominant hands (unoperated patients and controls). Error bars indicate standard errors. Asterisks indicate P < 0.05 Reactive inhibition Post-hoc comparisons showed SSRTs for patients with right subthalamotomy did not differ significantly from those of patients with left subthalamotomy [t(20) = 1.59, p = .12; did not survive correction for multiple comparisons due to the complexity of the four group design]. Right subthalamotomy patients did not differ from unoperated patients [t(22) = 1.33, p = .19]. Proactive action restraint ‘Critical’ Go reaction times were significantly slower than ‘non-critical’ Go reaction times for healthy controls [t(22) = 5.16, p < .001], and patients with left subthalamotomy [t(11) = 3.29, p < .01]. In contrast, no difference between the ‘critical’ and ‘non-critical’ Go reaction timess was found for unoperated patients [t(13) = 1.85, p = .09] and patients with right subthalamotomy [t(9) = .04, p = .96]. 16 The response delay effect difference score for patients with right subthalamotomy was less than unoperated [t(22) = - 1.58, p = .13] and left subthalamotomy patients [t(20) = 1.77, p = .09] but the differences did not survive correction for multiple comparisons due to the complexity of the four group design. The response delay effect for the left subthalamotomy patients did not differ from that of unoperated patients [t(24) = .14, p = .88] or controls [t(24) = -.91, p = .36]. The response delay effect for unoperated patients and controls did not differ significantly [t(35) = -.98, p = .33]. ‘Non-critical’ Go and StopRespond reaction times For ‘non-critical’ Go reaction times, the main effect of Group was significant [F(3,59) = 7.85, p < .001]. Post-hoc comparisons revealed no differences between right and left subthalamotomy groups [t(20) = .48, p = .63]. ‘Non-critical’ Go reaction times for right and left subthalamotomy groups were significantly faster than unoperated patients [right: t(22) = - 2.50, p = .02; left: t(24) = -2.11, p = .04 ], but significantly slower than controls [right: t(31) = 3.02, p < .01; left: t(35) = 2.12, p = .04]. Unoperated patients had significantly slower ‘non-critical’ Go reaction times than controls [t(35) = - 6.17, p < .001]. For ‘non-critical’ StopRespond reaction times (a ‘to be ignored’ stop signal), the main effect of Group was significant [F(3,59) = 7.68, p < .001] (see Table 2 and Figure S3). Post-hoc comparisons revealed that patients with right or left subthalamotomy did not differ significantly [t(20) = .46, p = .65]. Patients with right subthalamotomy had ‘non-critical’ StopRespond reaction times that were marginally faster than unoperated patients [t(22) = 2.07, p = .052]. Patients with left subthalamotomy were significantly faster than unoperated patients [t(24) = 2.65, p = .01]. Right subthalamotomy patients had non-significantly slower ‘non-critical’ StopRespond reaction times compared to controls [t(31) = 1.99, p = .055], as well as the left subthalamotomy group [t(35) = 1.27, p = .21]. Unoperated patients had significantly slower ‘non-critical’ StopRespond reaction times than controls [t(35) = - 5.45, p < .001]. 17 Figure S3. Mean ‘non-critical’ Go (A) and StopRespond reaction times (B) for operated Parkinson’s disease (PD) patients with right (R STN) or left (L STN) subthalamotomy, unoperated PD patients and control participants. The figures show reaction times for the contra-lesional (operated patients) or dominant hands (unoperated patients and controls). Error bars indicate standard errors. Asterisks indicate P < 0.05 Conflict-induced slowing Patients with right or left subthalamotomy did not differ from controls in terms of conflictinduced slowing [right subthalamotomy: t(31) = .10, p = .92; left subthalamotomy: t(35) = -.28, p = .77]. There were no differences between patients with right or left subthalamotomy in conflict-induced slowing [t(20) = .26, p = .79]. Omission errors Two Kruskal-Wallis tests were completed to compare the four groups in terms of ‘critical’ and ‘non-critical’ Go omissions errors. A significant difference was found between the groups for both ‘critical’ [X2 = 11.86, p < .01] and ‘non-critical’ Go omission errors [X2 = 12.30, p < .01]. 18 Post-hoc Mann-Whitney tests were completed to examine these significant Group effects. Patients with right or left subthalamotomy showed no significant differences in ‘critical’ Go omission errors [U = 53.50, p = .65]. Similarly, no significant differences in ‘critical’ Go omission errors were observed between patients with right [U = 31.50, p = .09] or left subthalamotomy [U = 40.00, p = .10] and unoperated patients. However, patients with right [U = 65.00, p = .03] or left [U = 78.00, p = .03] subthalamotomy made significantly more ‘critical’ Go omission errors compared to controls. Significantly more errors were made by the unoperated patients compared to controls [U = 52.00, p < .01]. Patients with right or left subthalamotomy showed no significant differences in number of ‘noncritical’ Go omission errors from each other [U = 58.00, p = .88] (Table 2). Similar results were obtained for operated patients compared with unoperated patients [right subthalamotomy: U = 32.00, p = .09; left subthalamotomy: U = 41.00, p = .11] and controls [right subthalamotomy: U = 74.00, p = .07; left subthalamotomy: U = 98.50, p = .12]. However, unoperated patients made significantly more ‘non-critical’ Go omission errors compared to controls [U = 39.50, p = .001]. 19 Supplementary material references Alvarez, L., Macias, R., Guridi, J., Lopez, G., Alvarez, E., Maragoto, C., et al. (2001). Dorsal subthalamotomy for Parkinson's disease. Mov Disord 16, 72-78. Alvarez, L., Macias, R., Lopez, G., Alvarez, E., Pavon, N., Rodriguez-Oroz, M.C., et al. (2005). Bilateral subthalamotomy in Parkinson's disease: initial and long-term response. Brain 128, 570583. Alvarez, L., Macias, R., Pavon, N., Lopez, G., Rodriguez-Oroz, M.C., Rodriguez, R., et al. (2009). Therapeutic efficacy of unilateral subthalamotomy in Parkinson's disease: results in 89 patients followed for up to 36 months. J Neurol Neurosurg Psychiatry 80, 979-985. Beck, A.T., Ward, C.H., Mendelson, M., Mock, J., and Erbaugh, J. (1961). An inventory for measuring depression. . Arch Gen Psychiatry, 561–571. Folstein, M.F., Folstein, S.E., and Mchugh, P.R. (1975). "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12, 189-198. Hughes, A.J., Daniel, S.E., Kilford, L., and Lees, A.J. (1992). Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55, 181-184. Verbruggen, F., Chambers, C.D., and Logan, G.D. (2013). Fictitious inhibitory differences: How skewness and slowing distort the estimation of stopping latencies. Psychological Science. 20