Pediatric Obesity: A Family Affair
advertisement

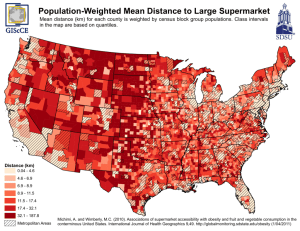
Pediatric Obesity: A Family Affair Samuel N. Grief, MD Outline Introduction Definition of childhood overweight/obesity Scope of Problem Etiology: Multifactorial Genetics and obesity Environment and obesity Culture and obesity Taking a pediatric nutrition history Nutrition recommendations for treating obesity Practical pointers for all Family Physicians in dealing with the obese child Conclusion Pediatric Obesity: A Family Affair Pediatric obesity is rapidly becoming a serious health epidemic in the united states. Health officials estimate the percentage of overweight/obese children has risen to 30% and is climbing. This symposium will bring the topic of pediatric obesity into the limelight elucidating: The severity of this health epidemic, The multiple causes of pediatric obesity, The genetic connection, The latest nutrition recommendations, A practical approach for family doctors to assess a child’s nutrition habits in the context of the family unit and provide sensitive and sound medical advice to help children and their family members conquer obesity. Definition of Childhood Overweight/obesity Adults: BMI – mild, moderate, severe or extreme For children, not clearly established BMI >85% defined as overweight BMI >=95% for age and gender BMI not used for infants Definition of overweight BMI varies with age Scope of Pediatric Obesity Problem NHANES III NHANES III Boys Age/Month NHANES I NHANES II HHANES 2-5 NHANES III 322 6-11 152 47 595 12-23 285 368 101 648 24-35 166 361 116 610 36-47 300 403 113 497 48-59 304 403 126 546 60-71 273 393 116 495 Number of Survey Participants in Sex and Age Groups by Survey NHANES III Girls Age/Month NHANES I NHANES II 2-5 HHANES NHANES III 334 6-11 143 53 576 12-23 267 350 118 635 24-35 129 315 112 591 36-47 286 340 85 545 48-59 281 386 93 532 60-71 314 369 112 554 Number of Survey Participants in Sex and Age Groups by Survey Prevalence of overweight Based on Percentage of 2-5 year-old children above the 95% of the weight-for-stature growth reference (NHANES III) 14 12 10 Non Hispanic White Non Hispanic Black Mexican American 8 6 4 2 0 Non Hispanic White Non Hispanic Black Mexican American Boys 2-3 Girls 2-3 Boys 4-5 Girls 4-5 1.1 2.8 6.2 2.8 5.6 10.5 2.7 8.5 12 9 11.2 13.2 NHANES I, II, III 6-11 Months White Boys Girls 2.7 7.3 6.5 11.1 NHANES I NHANES II NHANES III 9.0 9.5 10.7 Mexican American HHANES NHANES III 4.5 12.2 7.3 16.3 NHANES I NHANES II NHANES III Black NHANES I, II, III 6-11 Months ALL RACES NHANES I NHANES II NHANES III Boys Girls 4.0 7.5 6.2 10.8 NHANES I, II, III 12-23 Months White Boys Girls NHANES I NHANES II NHANES III Black 8.3 6.6 7.6 5.7 7.5 7.9 NHANES I NHANES II NHANES III 3.8 11.8 6.4 8.9 6.8 15.2 Mexican American HHANES NHANES III 7.9 13.6 11.3 14.0 NHANES I, II, III 12-23 Months ALL RACES NHANES I NHANES II NHANES III Boys Girls 7.5 7.2 7.5 6.1 7.2 9.5 NHANES I, II, III 2 – 3 Years White Boys Girls NHANES I NHANES II NHANES III Black 1.9 1.5 2.0 1.6 2.9 4.5 NHANES I NHANES II NHANES III 3.4 2.2 3.0 2.2 1.0 6.2 Mexican American HHANES NHANES III 5.6 3.0 4.2 6.2 NHANES I, II, III 2 - 3 Years ALL RACES NHANES I NHANES II NHANES III Boys Girls 3.1 2.0 2.1 2.0 2.5 4.8 NHANES I, II, III 4 - 5 Years White Boys Girls NHANES I NHANES II NHANES III Black 4.0 4.6 4.3 6.0 7.4 11.2 NHANES I NHANES II NHANES III 7.0 3.0 8.7 5.0 6.5 12.6 Mexican American HHANES NHANES III 4.9 12.0 10.6 13.2 NHANES I, II, III 4 - 5 Years ALL RACES NHANES I NHANES II NHANES III Boys Girls 4.4 4.4 5.0 5.8 7.6 10.8 NHANES III Percentage of children younger than 3 years above the 95% of the weight-for-length growth reference, NHANES III Boys NHW NHB MA Under 1 9.6 9.1 10.2 Ages 1 & 2 7.5 6.4 8.9 Girls NHW 12.8 11.0 10.2 13.0 11.5 8.4 NHB MA Both Sexes 15.0 15.5 10.3 14.0 16.8 9.4 Assessment of Medical Conditions Related to Obesity Findings Potential Conditions History Developmental Delay Genetic Disorders Poor linear growth Hypothyroidism, Cushing’s syndromePrader-Willi syndrome Headaches Pseudotumor Cerebri Nighttime breathing difficulty Sleep apnea, obesity hypoventilation syndrome Daytime somnolence As above Abdominal pain Gallbladder disease Hip or knee pain Slipped capital femoral epiphysis Oligomenorrhea or amenorrhea Polycystic ovarian syndrome Assessment of Medical Conditions Related to Obesity Family History Obesity NIDDM Cardiovascular disease Hypertension Dyslipidemia Gallbladder disease Social/psychologic history Tobacco use Depression Eating Disorder Assessment of Medical Conditions Related to Obesity Physical exam Height, weight, BMI Triceps skinfold thickness Truncal obesity Blood pressure Dysmorphic features Acanthosis nigricans Hirsutism Violaceous striae Optic disks Assessment of Medical Conditions Related to Obesity Tonsils Abdominal tenderness Undescended testicle Limited hip range of motion Lower leg bowing Risk of cardiovascular disease; Cushing’s syndrome Genetic disorders (PW) NIDDM, insulin resistance Polycystic ovarian syndrome; Cushing’s syn Pseudotumor cerebri Assessment of Medical Conditions Related to Obesity Sleep apnea Gallbladdeer Disease Prader-Willi Syndrome Slipped Capital Femoral Epiphysis Blount’s Disease Etiology of Pediatric Obesity: Multifactorial Environmental: Neighborhood, school, community Genetic: Inborn diseases, chromosomal mutations, familial, ethnic predisposition Cultural: Increased risk with minorities Societal: Affluent vs. Underserved Physical: Height and body frame; sick vs. healthy Attitude: Family influence on nutrition habits and physical activity Medical advice: Doctors not taking an active role The American way of life! Genetics and Obesity Twin studies Familial syndromes: Cohen’s, Alstrom’s, and Bardet-Biedl (look these up!!!) Ob gene and leptin POMC Pro-opiomelanocortin MC4R – a melanocortin receptor Genetics and obesity What next? Additional leptin to those who are deficient. Ongoing research for pharmacological manipulation. Continued research in rodents is directly relevant to humans. Environment and Obesity Socioeconomic status and rates of obesity Single parent families and risk of obesity Social support and relevance to pediatric obesity School and extracurricular activities Inner city vs. suburban setting Western vs. third world setting Culture and Obesity Minorities and increased rates of obesity African-American Hispanic Native Indian Pacific Islander White Asian European Other Culture and Obesity Culture and food Food is a way of life Learn about different cultures: ASK! The taste of Chicago… You deserve a… BREAK! Nutrition Exercise 1. 2. 3. 4. 5. 6. Split into groups of three Designate one member as the physician Designate one member as the parent of an obese child Designate one member as the observer The physician has ten minutes to obtain a complete nutrition history from the parent Observer to take notes re: 1. 2. 3. 4. Style – effective or not and why? Open or closed ended questions Anything missing? Anything else? Ready, set… GO! Taking a pediatric nutrition history Back to basics! Methods of assessing dietary intake: 1) 24-Hour recall 2) Usual Intake/Diet history 3) Food frequency questionnaire 4) Family history 5) Past medical history 6) Any diets that have been tried? Successful? 7) Social habits: cigs, caffeine, illicit drugs, ETOH 8) MEDS, vitamins, herbals 9) Food allergies? Lactose intolerance? 10) ROS: Constitutional, GI, GU Pediatric Nutrition Refer to a trusted Registered Dietitian! Recommendations based on the USDA Food Guide Pyramid Most children will need to maintain their current weight until they reach a lower level BMI There is no magic wand to wave The three Es: Emphasize proper nutrition, Encourage an overall family approach to modifying nutrition habits, and Empathize with all those concerned. Medicinal Treatment Options for Pediatric Obesity Few are currently viable OTCs: Diet pills, ephedra, metabolife, caffeine, chitosan, hydroxycitric acid, pyruvate, etc. Methylphenidate, dextroamphetamine, etc. Diuretics Thyroid hormone Growth hormone Testosterone Leptin Metformin Xenical Surgical Treatment Options for Pediatric Obesity Useful for adolescents with extreme obesity Last resort option for severely obese adolescents Choose patients carefully Obesity and Psychological Disorders in Children Do obese children suffer from greater rates of depression? Study of 868 third grade students KEDS Results: there is a relationship between depressive symptoms and BMI in preadolescent girls; not in boys. Girls express more overweight concerns. Take home message: when girls present to Family Docs, assessing overweight concerns with the 5question scale may help identify overweight girls at highest risk of developing depression, and perhaps subsequent eating disorders. Obesity and Eating Disorders At any given time, 44% of adolescent girls and 15% of adolescent boys are “dieting” Prevalence of eating disorders (anorexia and bulimia) is estimated to be 1-4% of adolescent and young adult women Predisposing factors may include: genetic, biological vulnerability, individual psychopathology, familial and cultural influences Survey of women on the most common weight loss practices: weighing oneself regularly, walking, fasting, meal skipping, diet pills, cigs Weight cycling: not related to increased psychopathology! Non-dieting approaches for obese children Identify and combat cultural notions that “thinner is better” and that body weight can be controlled by willpower Help participants “stop dieting” by abandoning efforts to restrict energy intake and avoid certain foods Help participants identify and eat in response to the body’s “natural” hunger and satiety signals Increase self-esteem and positive body image through self-acceptance rather than weight reduction Increase awareness about dieting behaviors and their purported ill effects Obesity and Children Miscellaneous Early onset of adiposity rebound (AR) Early onset of puberty related to obesity in girls Increased rates of Type 2 diabetes diagnosed among obese children Adult food fears impact children General Approach to Treating Pediatric Obesity Intervention should begin early The family must be ready for change Clinicians should educate families about medical complications of obesity Clinicians should involve the family and all caregivers in the treatment program Treatment programs should institute permanent changes, not short-term diets or exercise programs aimed at rapid weight loss General Approach to Treating Pediatric Obesity As part of the treatment program, a family should learn to monitor eating and activity The treatment program should help the family make small, gradual changes Clinicians should encourage and emphasize and not criticize A variety of experienced professionals can accomplish many aspects of a weight management program BIBLIOGRAPHY 1. 2. 3. 4. 5. 6. 7. 8. Ogden, Troiano, et.al., Prevalence of Overweight Among Preschool Children in the United States, 1971 Through 1994, PEDIATRICS, Vol.99, No.4, April 1997 Barlow and Dietz, et.al.,Obesity Evaluation and Treatment: Expert Committee Recommendations, PEDIATRICS, Vol.102, No.3, September 1998 Goodman, et.al., Accuracy of Teen and Parental Reports of Obesity and Body Mass Index, PEDIATRICS, Vol.106, No.1, July 2000, pp.52-58 Whitaker, et.al., Predicting obesity in young adulthood from childhood and parental obesity, N Engl J Med, 1997; 337:869-873 Kiernan and Winkleby, Identifying Patients for Weight-Loss Treatment: An Empirical Evaluation of the NHLBI Obesity Education Initiative Expert Panel Treatment Recommendations, ARCHIVES of Internal Medicine, Vol.160, No.14, July 24, 2000, pp 2169-2176 Farooqi and O’Rahilly, Recent advances in the genetics of severe childhood obesity, ARCHIVES OF DISEASE INC CHILDHOOD, Vol.83, No.1, July 1, 2000, pp 31-34 Guy, Roche, et.al., The predictive value of childhood body mass index values for overweight at age 35 y., Am J Clin Nutr, 1994; 59:810-819 Oken and Lightdale, Updates in pediatric nutrition, Current Opinion in Pediatrics, VOl13, No.3, June 2001, pp 280-288 BIBLIOGRAPHY 10. Mokdad, Serdula, Dietz, et.al., The spread of the obesity epidemic in the United States, 1991-1998, JAMA, 1999, 282:1519-152210. Anderson, et.al., Relationship of physical activity and television watching with body weight and level of fatness among children, JAMA, 1998, 279:938-942 11. Spieth, et.al., A Low-Glycemic Index Diet in the Treatment of Pediatric Obesity, ARCHIVES of Pediatrics & Adolescent Medicine, Vol.154, No.9, Sept.2000, pp 947-951 12. Flegal, et.al., Overweight and obesity in the United States: prevalence and trends, 1960-1994, Int J Obes Relat Metab Disord, 1998; 22:39-47 13. Wing, et.al., Behavioral Science Research in Diabetes: Lifestyle changes related to obesity, eating behavior, and physical activity, Diabetes Care, Vol.24, No.1, January 2001, pp 117-123 14. Millis, et.al., The relationship between childhood onset obesity and psychopathology in adulthood, J Psychol 127: 547-551, 1993 15. Review article: Dieting and the Development of Eating Disorders in Overweight and Obese Adults, ARCHIVES of Internal Medicine, Vol.160, No.17, Sept.25, 2000, pp 2581-2589 16. Baughcum, et.al., Maternal Perceptions of Overweight Preschool Children, Pediatrics, Vol.106, No.6, Dec.2000, pp 1380-1386 BIBLIOGRAPHY 17. Strauss, et.al., Gastric bypass surgery in adolescents with morbid obesity, The Journal of Pediatrics, Vol.138, No.4, Apr.2001, pp 499-504 18. Erickson, et.al., Are overweight children unhappy? BMI, Depressive symptoms, and overweight concerns in elementary school children, ARCHIVES of Pediatrics & Adolescent Medicine, Vol.154, No.9, Sept.2000, pp 931-935 19. Roberts and Dallal, The New Childhood Growth Charts, Nutrition Reviews, Vol.59, No.2, Feb.2001, pp 31-36 20. Roberts and Dallal, The New Childhood Growth Charts, Nutrition Reviews, Vol.59, No.2, Feb.2001, pp 31-36 Troiano, et.al., Overweight prevalence among youth in the United States: why so many different numbers? Int J Obes Relat Metab Disord, 1999;23:S22-7 21. Bundred, et.al., Prevalence of overweight and obese children between 1989 and 1998: population based series of cross sectional studies, BMJ, Vol.322, No.7282, Feb.10,2001, pp 326-328 22. Baker, et.al., The Use and Misuse of Juice in Pediatrics, Pediatrics, Vol.107, No.5, May 2001, pp 1210-121Fagot-Campagna, et.al., Diabetes, Impaired Fasting Glucose, and Elevated HbA1c in US Adolescents: The Third National Health and Nutrition Examination Survey, Diabetes Care, Vol.24, No.5, May 2001, pp 834-83 23. Gidding, Samuel S., MD, Cholesterol Guidelines Debate, Pediatrics, Vol.107, No.5, May 2001, pp 1229-123 24. Bray and Tartaglia, Medicinal strategies in the treatment of obesity, NATURE, Vol.404, Apr.6, 2000, pp 672-677 Thank you very much!