Case Study: Nutrition Management of Aspiration Pneumonia
advertisement

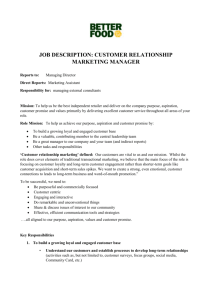
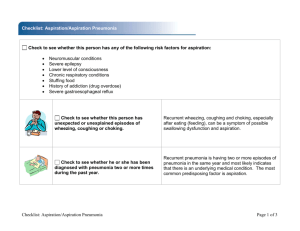
Case Study: Nutrition Management of Aspiration Pneumonia Renee (Pik Shan) Fung Dietetic Intern ARAMARK Healthcare Distance Learning Dietetic Internship Maple Grove Hospital Disease Description Definitions Aspiration- the inhalation of oropharyngeal or gastric contents into the larynx and lower respiratory tract Aspiration Pneumonitis- Chemical injury caused by the inhalation of sterile gastric contents Aspiration Pneumonia- Infectious process caused by the inhalation of oropharyngeal secretions that are colonized by pathogenic bacteria Aspiration Aspiration can cause serious illnesses and even death. Four common problems of aspiration: 1. Failure to distinguish aspiration pneumonitis from aspiration pneumonia 2. Tendency to consider all pulmonary complications of aspiration as infectious 3. The failure to identify the spectrum of pathogens in patients with infectious complications 4. Misconception that aspiration must be witnessed for it to be dx. Etiology Half of all healthy adults aspirate. The human body is capable of removing foreign objects by coughing Individuals who have problem with removing foreign objects properly are at risk of developing aspiration pneumonia/ pneumonitis Pathophysiology Common cause of aspiration pneumonia is the inhalation of Haemophilus influenza and Streptococcus Pneumonia. They are colonized in the nasopharynx or oropharynex before they are aspirated. Pathophysiology Since aspiration pneumonitis is the inhalation of sterile gastric contents, bacterial infection does not play an important role at early stage. At a later stage of aspiration pneumonitis, bacterial colonization may occur if the individual has gastroparesis, small-bowel obstruction, receives enteral feedings, or has higher pH gastric acids. In this case, the individual has aspiration pneumonia. Aspiration Pneumonia Diagnosis Signs/symptoms: (signs of aspiration) Persistent cough and fever. However, many times silent aspiration can develop. In aspiration pneumonia, the episode of aspiration is generally not witnessed. Swallowing evaluation by an SLP CT scan- radiographic evidence of foreign material infiltrating in patient’s lungs (some may be undetectable) Individuals who are at risk of aspiration pneumonia Currently, there are no recognized guidelines for risk factors of aspiration pneumonia Elderly Neurologic Dysphagia Unconscious individuals Individuals at hospitals Disruption of the gastroesophageal junction Abnormalities of the upper GI tract Poor oral care individuals Patients with stroke After the removal of an endotracheal tube due to residual effects or sedative drugs, the presence of an NG tube, and swallowing dysfunction related to alterations of upper-airway sensitivity, glottic injury, and laryngeal muscular dysfunction Co-morbidity Increased LOS Increased cost Increased morbidity and mortality Decrease aspiration pneumonia complication Early detection of patents who are at risk of or have aspiration pneumonia SLP evaluation Barium swallow CT scan Provide appropriate care Evidenced Based Nutrition Recommendations for Aspiration Pneumonia AND Evidence Analysis Library and the A.S.P.E.N 30-45 degree head of bed elevation position Promotility agents AND: if >500 mL GRV A.S.P.E.N: If >250 mL GRV E.g. Metoclopramide and Erythromycin Associated with reduced GRV in critically ill pts Recommend to be used in critically ill pts who experience feeding intolerance (high gastric residuals, emesis) Horiuchi A, et al (2013) – Elemental diets may reduce the risk of aspiration pneumonia in bedridden gastrostomy-fed patients Hypothesis: Elemental diets may be useful for the prevention of aspiration pneumonia possibly through more rapid gastric emptying than standard liquid diets. This study is separated into 2 different parts. Horiuchi A, et al – Elemental diets may reduce the risk of aspiration pneumonia in bedridden gastrostomy-fed patients PART 1 Participants: 128 Bedridden PEG participants Age: Average 80 years old Gender: 60 of the participants were male. Method: 60 subjects were assigned to elemental diet group 67 subjects were assigned to the standard liquid diet group. Record subjects who experienced aspiration and aspiration pneumonia Horiuchi A, et al – Elemental diets may reduce the risk of aspiration pneumonia in bedridden gastrostomy-fed patients PART 1 Result: The number of patients who had diet aspirated from the trachea or who developed new aspiration pneumonias in the elemental group was significantly less than the standard liquid diet group. Horiuchi A, et al – Elemental diets may reduce the risk of aspiration pneumonia in bedridden gastrostomy-fed patients PART 2 Randomized, crossover trial which focused on identifying the gastric emptying velocity differences between the two diets via PEG Participants: 19 PEG subjects Horiuchi A, et al – Elemental diets may reduce the risk of aspiration pneumonia in bedridden gastrostomy-fed patients PART 2 Result: Elemental diets were associated with more rapid gastric empting. Possibly due to: Fatty diet takes longer time to empty and is associated with gastroesophageal regurgitation. Standard liquid diet has higher fat content than elemental diet. Horiuchi A, et al – Elemental diets may reduce the risk of aspiration pneumonia in bedridden gastrostomy-fed patients Limitation: Study 1 had increased risk of bias because it was neither randomized nor blinded Study 2 could not prove the hypothesis by itself Participants in study 1 included those who had pervious experience of aspiration which suggested that they can be generalized. Study 2 might have “carry-over” issues between treatments. Horiuchi A, et al – Elemental diets may reduce the risk of aspiration pneumonia in bedridden gastrostomy-fed patients In summary, this study found elemental diets to be associated with reduced episodes of aspiration and more rapid gastric empting among bedridden PEG patients. Nevertheless, further research is needed to prove whether or not there is a causation effect existing between rapid gastric empting and reduced episodes of aspiration and aspiration pneumonia. Jiyoung J, et al (2013) - Effect of gastric versus post-pyloric feeding on the incidence of pneumonia in critically ill patients: observations from traditional and Bayesian random-effects meta-analysis. Examined the effect of gastric versus post-pyloric feeding on the incidence of pneumonia in critically ill patients. Method: 2 reviewers reviewed and selected studies searched from MEDLINE, EMBASE, Web of Science, and CCTRD. The reviewers then compared gastric and post-pyloric feeding in critically ill patients. Selection Criteria: Trails should report at least one of the following outcomes: incidence of pneumonia, vomiting, or aspiration, and studies that were published in any language. Selected studies were all published in English and were from Canada, Australia, Italy, Spain, Taiwan, and the USA. The selected studies included patients from general ICUs, pediatric ICU, neurological ICU, and severe acute pancreatitis from gastroenterology. Jiyoung J, et al - Effect of gastric versus post-pyloric feeding on the incidence of pneumonia in critically ill patients: observations from traditional and Bayesian random-effects meta-analysis. Result: The incidences of pneumonia were 16.3% in the post-pyloric feeding group and 26.1% in the gastric feeding group (P = 0.001). There was no significant differences in the beneficial effect of the post-pyloric feed location (duodenum (P=0.03) versus jejunum (P= 0.07). there was no significant difference between post-pyloric feeding group and gastric feeding group in the amount of aspiration (P= 0.55) and vomiting (P = 0.56) incidence. Jiyoung J, et al - Effect of gastric versus post-pyloric feeding on the incidence of pneumonia in critically ill patients: observations from traditional and Bayesian random-effects meta-analysis. Limitation Not all outcomes in the selected studies were reported. Many of the studies were not good qualities. For example, potential biases may exist in the selected studies, clinical heterogeneity in the studies that may account for the statistical heterogeneity that were found in this study which could have affected the result, and not all studies reported adequate concealment, blinding of participants, and outcome assessment. The amount of eligible studies was relatively small. (757 pts; 15 studies) Jiyoung J, et al - Effect of gastric versus post-pyloric feeding on the incidence of pneumonia in critically ill patients: observations from traditional and Bayesian random-effects meta-analysis. In summary, Jiyong J, et al suggested that critically ill patients with post-pyloric feeding is associated with reduced incidence of pneumonia when compared with gastric feedings. Meanwhile, there is no significant difference in incidence of neither aspiration nor vomiting between the two groups. Finally, no significant beneficial difference was found between post-pyloric feeds to the jejunum or duodenum. Case Presentation Case Presentation 58 yrs old F Lives at group home Aspiration noted by group home manager. Patient had continuous coughing and developed a fever. Patient was admitted to the ER the next day Nutrition Care Process- Assessment Client Hx Mental Retardation Epilepsy Schilder’s cataract Hypothyroidism Family Hx Unknown; pt was in foster care since the age of 2 DNR status Nutrition Care Process- Assessment Food/ Nutrition-Related Hx Patient consumes a ground diet (Dysphagia 2) with honey thickened liquids for the past 15 yrs due to recurrent aspirations NKFA Upon admission, patient was provided with calcium + vit D pills, D5W NS @ 125 mL/hr, Colace, Synthroid, Protonix, Miralax, and Propofol ranging 7-10 mL/hr Nutrition Care Process- Assessment Nutrition-Focused Physical Findings Patient had gained 14 lbs in 2 days. Patient has fluid retention. Skin integrity: minor impairment Appetite: Fine prior to aspiration episode SLP recommended patient to be NPO besides medications are crushed into applesauce. Patient unable to self-feed Nutrition Care Process- Assessment Anthropometric Measurements UBW: Unable to obtain d/t patient’s mental state Height: 4’10” IBW: 95 lbs +/- 10% BMI: 28.5 – overweight *Patient is retaining fluid, weight may not be a good indicator for nutrition status Nutrition Care Process- Assessment Biochemical Data, Medical Tests, and Procedures A swallowing evaluation was performed by the SLP. The SLP noted signs and symptoms of aspiration The patient will have an OJ tube placed for short-term nutrition support. A chest x-ray was done before patient being intubated. Lab Results Component Value Norm Date al Rationale ALBUMIN g/dL GLUCOSE mg/dL GLUCOSE 3.0* 3.5-5 9/25/2013 Malnutrition, acute inflammation 91 9/27/2013 GLUCOSE 116* 9/26/2013 Elevation due to stressed state 9/27/2013 Check for hydration status 9/27/2013 GI loss, malabsorption 94 70110 9/27/2013 SODIUM 139 mEq/L POTASSIUM 3.2* mEq/L PHOSPHORUS 3.1 136145 3.55.5 9/25/2013 Check for re-feeding syndrome risk MAGNESIUM mg/dL CHLORIDE mEq/L CALCIUMSER UM mg/dL BUNUREANR O CREATININE mg/dL 2.0 1.8-3 9/25/2013 Check for re-feeding syndrome risk 106 95105 7.6* 9-11 9/27/2013 Check for fluid/ acid-base imbalances 9/27/2013 Low serum calcium; Corrected Ca: 8.4* 19* 9/27/2013 Malnutrition 9/27/2013 Check for kidney function 1.15 0.61.2 Nutrition Care Process- Assessment Nutrition Need Calories: 1300 kcal (30kcal/kg IBW) Protein: 65-86 gm (1.5-2 gm/kg IBW) Fluids: 1300 mL Nutrition Classification: Severely Compromised, Will follow up every 1-3 days New TF (+4), Low Albumin (+2), Swallowing Problems (+3), Dysphagia (+3) Nutrition Care Process: Nutrition Diagnoses #1 Swallowing difficulty (NC-1.1) related to respiratory status as evidenced by NPO status, need for dysphagia diet, and aspiration history. Nutrition Care Process: Nutrition Intervention #1 Enteral Nutrition (ND-2.1). Recommend initiate enteral nutrition via OJ tube or NJ tube, once placement verified start Isosource 1.5 at rate of 15 mL/hr x 8 hrs; if tolerating advance by 10 mL every 8 hrs to current goal rate of 30 mL/hr x 24 hrs/day. No current free water flushes until IVF addressed. (Table 5) #2 Collaboration and Referral of Nutrition Care: Collaboration with other providers (RC-1.4). No residual checks with Jejunal feeding Nutrition Care Process: Nutrition Intervention Short-term Goal/ Expected Outcome : Maximize nutrient intake: Patient receives more than 75% of recommended nutritional needs via PO or nutrition support. Patient maintains admission weight. Long-term Goal/ Expected Outcome: Patient will be able to meet more than 75% of recommended nutritional needs via PO intake or long-term tube placement in place for feeding. Patient reduces aspiration incidence. Nutrition Care Process: Monitoring and Evaluation Monitor and Evaluation (Nutrition Intervention Performed): #1Enteral nutrition intake (FH). Formula/ solution (1.3.1). Patient was receiving enteral support via OJ tube with Isosource 1.5 formula at 30 mL/hr x 24 hours. Patient tolerated tube feeding at goal rate. The patient is receiving 100% of recommended kcal and protein needs via nutrition support. #2 Micronutrient Intake (1.6) Mineral/ element intake (2) Calcium (1). Patient’s corrected calcium is WNL. Phosphorus (6). Patient is on phosphorus replacement protocol. #3 Biochemical data, medical tests and procedures (BD). Glucose/ endocrine profile (1.5). Glucose, fasting(1). Glucose continues to be high. High glucose possibly due to stress since Hgb A1c is WNL. Electrolyte and renal profile (1.2). Continued to monitor patient’s renal lab. #4 Anthropometric Measurements (AD). Weight change (1.1.4). Patient gained 9 lb since admission. Nutrition Care Process: Monitoring and Evaluation Short-term goal: (Achieved) Short-term goal: Maximize nutrient intake: Patient receives more than 75% of recommended nutritional needs via PO or nutrition support. (Not Achieved) Patient maintain current weight. Long-term goal: (Not Achieved) Patient will be able to meet more than 75% of recommended nutritional needs via PO intake or long-term tube placement in place for feeding. (Not Achieved) Patient reduces aspiration incidence. Nutrition Care Process: Monitoring and Evaluation The patient was admitted to the hospital from 9.27 to 10.14. The patient was followed up everyday by a dietitian. Meanwhile, the patient had developed acute respiratory failure and was at critical condition. Her tube feeding formula was switched from Isosource 1.5 to Impact Peptide 1.5 which is an elemental formula for patients who are in stressed condition. The patient then became more stable, and had a PEG placement for long-term nutrition support. The patient was discharged with nocturnal feeds Isosource 1.5 65 mL/hr x 12 hours/day. The reason why she was discharged with Isosource 1.5 instead of Impact Peptide 1.5 was because her insurance company would not cover Impact Peptide 1.5 since it is an elemental formula and is more expensive. Patient’s Progress after Discharge The patient was re-admitted to the hospital 4 days after being discharged. The patient was re-admitted for aspiration because she was having PO intake. The patient is on DNR status. The RD recommended modifying the PEG tube to a PEG-J tube, however, IR stated that PEG needed to be in place for 3-4 weeks prior to adjust tube. During her second admission, the tube feeding was either running at a low rate or on hold for a few times due to reoccurring emesis. Finally, the patient was able to tolerate tube feeding with bolus feeds. The patient was discharged on 10/26/2013 with the same recommendation of tube feeding regimen as previous time. Evidence-based recommendation implemented on this case 30-45 degrees head of bed position Enteral nutrition support to decrease risk of aspiration Jejunal feeds rather than gastric feeds Elemental formula was used Conclusion The current recommendation for Aspiration Pneumonia care is to feed patients who are receiving tube feeding in a 30-45 degree elevation of head of bed position. Promotility agents are also encouraged to use. There are controversial in whether or not jejunal feeding is more beneficial over gastric feeding; More research need to be done to confirm this finding. Further more, research suggest that elemental formula may be a better choice than standard formula, however, elemental formulas are more expensive and many insurance do not cover it. References 1. 2. 3. 4. 5. 6. 7. Horiuchi A, Nakayama Y, Sakai R, Suzuki M, Kajiyama M, Tanaka N. Elemental diets may reduce the risk of aspiration pneumonia in bedridden gastrostomy-fed patients. Am J Gastroenterol. 2013; 108: 804-810. Jiyong J, Tiancha H, Huiqin W, Jingfen J. Effect of gastric versus post-pyloric feeding on the incidence of pneumonia in critically ill patients: observations from traditional and Bayesian randomeffects meta-analysis. Clin Nutr. 2013; 32: 8-15. Echevarria IM, Schwoebel A. Development of an intervention model for the prevention of aspiration pneumonia in high-risk patients on a medical-surgical unit. Medsurg Nurs.2012; 21 (5): 303-308. Marik P. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001; 344(9): 665-671. Komiya K, Ishii H, Umeji K, et al. Impact of aspiration pneumonia in patients with communityacquired pneumonia and healthcare-associated pneumonia: A multicenter retrospective cohort study. Respirology.2013; 18 :514-521. Garcia J, CCC, Chambers E. Managing dysphagia through diet modifications. Am J Nurs. 2010; 110(11): 26-33 Recommendations Summary CIU: Optimizing Enteral Nutrition Delivery. Academy of Nutrition and Dietetics Evidence Analysis Library Web site. http://andevidencelibrary.com/template.cfm?key=3256.Accessed December 14, 2013 Reference 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Bankhead R, Boullata J, Brantlet S, et al. Enteral nutrition practice recommendations. J Parenter Enteral Nutr. 2009; 33(2): 123-167. Ho KM, Dobb GJ, Webb SA. A comparison of early gastric and post-pyloric feeding in critically ill patients: a meta-analysis. Intens Care Med. 2006; 32: 630-649 Marik PE, Zaloga GP. Gastric versus post-pyloric feeding: a systematic review. Crit Care. 2003; 7: R46-R51. Heyland DK, Drover JW, Dhaliwal R, Greenwood K. Optimizing the benefits and minimizing the risks of enteral nutrition in the critically ill: role of small bowel feeding. Jpen-Parenter Enter. 2002; 25: S51-S55 American Dietetic Association. International Dietetics & Nutrition Terminology Reference Manual. 2nd ed. Chicago, Il: American Dietetic Association; 2009. Pronsky ZM, Crowe SR. Food Medication Interactions. 17th ed. Birchrunville, PA: Food-Medication Interactions; 2012. Nutrition Care Manual Web site. https://www.nutritioncaremanual.org/to pic.cfm?ncm_category_id=1&lv1=5538&lv2=255469&ncm_toc_id=255469&ncm_heading=Nutrition%20Car e. Accessed Dec 15, 2013. ARAMARK Healthcare. Assessment and education policy #2: Nutrition status classification worksheet. Patient Food Services: Policies and Procedures, Volume IV; 2007. White JV, Guenter P, Jensen G, et al. Consensus statement: academy of nutrition and dietetics and American society for parenteral and enteral nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Parenter Enteral Nutr. 2012; 36: 278-279 American Dietetic Association. International Dietetics & Nutrition Terminology Reference Manual. 2nd ed. Chicago, Il: American Dietetic Association; 2009.