Paul Hinchey MD, MBA, FACEP
Jose Cabanas MD, MPH, FACEP
Update on important new EMS literature
Therapeutic hypothermia
EMS 12-lead ECG
Discuss medication related events
Understand the extent of medication errors and
their impact on patient care
Discuss common strategies to prevent medical
errors
Update on clinical performance improvement
activities
What is optimal target temperature for
PCAC Therapeutic Hypothermia?
Total 939 patients in randomized
controlled trial
36 International ICUs across Europe
Study endpoint: mortality/neuro outcome
80% VF/VT; 20% Non VF/VT
NEJM (2013)
32-33 vs. 35-36 TH
Unwitnessed asystole cases not included
24% intravascular; 76% surface cooling
28 hours of total cooling
NEJM (2013)
60
55
54
52
53
52
50
45
40
35
Survival
30
Poor Neuro
25
20
15
10
36
33
NEJM (2013)
In unconscious survivors of OHCA of
presumed cardiac cause, TH at a targeted
temperature of 33°C did not confer a benefit
as compared with a targeted temperature of
36°C.
Preventing Hyperthermia appears crucial.
No changes in our current process for PCAC
Does Prehospital TH have benefits?
Randomized clinical trial1,359 patients
Seattle King County Medic 1
583 with VF; 776 non-VF
Almost all patients cooled on ED arrival
JAMA (2013)
EMS cooling: up to 2L of 4C° LR
Mean core temp decrease by 1.20 C° to ED
EMS patients took 1 hr less to get to 34°C
Study endpoints: mortality and neuro status
EMS pts: 7-10mg pavulon + 1-2 mg valium
JAMA (2013)
70
64
63
60
50
VF
40
Non-VF
30
20
16
19
10
No EMS TH
EMS TH
No difference in Neuro Outomes
• EMS TH higher cases of pulmonary
edema. (p<.001)
• Remember Control group did NOT receive
paralytics.
Prehospital TH reduced core temperature
and reduced the time to reach a temperature
of 34°C.
No improvement in survival or neurological
status.
This is one study, no change in our system at
this time.
How often are STEMI patients initial
ECG non-diagnostic?
Do repeat ECGs have real value in
routine evaluation of CP patients?
41,560 STEMI patients in ACTION
Registry (2007-2010)
For patients with an initial non-diagnostic
ECG (11%) , 72.4% (N= 3,305) had an ECG
diagnostic for STEMI within 90 minutes.
No significant differences in the
administration of guidelines-recommended
treatments for STEMI.
Do repeat 12-lead ECGs make a difference?
Do repeat prehospital ECGs make any
difference in STEMI diagnosis?
Canadian Study
Prehosp Emerg Care 2012; 16:109-114
Retrospective Analysis of 325 consecutive
prehospital STEMI’s
EKG on-scene, repeat en-route and pre ED
entry
275 STEMI’s in First EKG (84.6%)
30 STEMI’s in second EKG (93.8%)
20 STEMI’s in third EKG (100%)
Prehosp Emerg Care 2012; 16:109-114
1/10 STEMI cases not apparent in first 12lead ECG.
ACS cases evolve – repeat 12-leads!
Prehospital ECG’s save approx. 20-30
minutes in reperfusion time.
1999 Institute of
Medicine (IOM) report:
3-4% of hospital patients
are harmed by the health
care system
7% of hospital patients
are exposed to a serious
medication error
50,000 – 100,000
deaths/ yr from medical
mistakes
Patient Safety Event
Serious Safety Event
Event that reaches the patient & results in
(death, life-threatening consequences, or serious
physical or psychological injury
Precursor Safety Event
Event that reaches the patient & results
in minimal to no harm
Near Miss “Good Catch”
An event that almost happened,
but error caught by a detection barrier
©2010 Healthcare Performance Improvement, LLC.
ALL RIGHTS RESERVED.
Courtesy Dr. Edmond – SETON HRO
Serious
Safety
Event
Precursor
Safety
Event
Near Miss
Safety Event
“Good Catch”
Some holes due
to active failures
Losses
Hazards
Other holes due to
latent conditions
Successive layers of defences, barriers and safeguards
System defences
Wrong medication
Wrong dose / route
Unrecognized clinical deterioration
Wrong procedure
Tunnel vision / decision-making
Treatment delay
Knowledge-based
1.Figuring it Out
30-60 errors/100 acts
15% of
healthcare errors
Rule-based
2.By the Rules
1 error/100 acts
Skill-based
3. Auto-Pilot
3 errors/1,000 acts
60% of
25% of
healthcare errors healthcare errors
“Any preventable event that may cause or lead
to inappropriate medication use or patient
harm while the medication is in the control of
the health care professional, patient, or
consumer”
National Coordinating Committee-Medication Error Reporting and Prevention (NCC MERP); accessed at
http://www.nccmerp.org/aboutMedErrors.html; Jan. 2012.
Figure 2. Commonly studied medication errors as causes of adverse drug events (ADEs): percent of ADEs for each cause: Reducing and
Preventing Adverse Drug Events To Decrease Hospital Costs. March 2001. Agency for Healthcare Research and Quality, Rockville, MD
Emergency situation
No written order
No external crosscheck
No electronic decision support
High‐risk medications
Drug shortage issues and constant
substitutions
EMTPs completed pediatric patient
simulation scenarios
Failure to use Broselow tape: 50%
Incorrect use of Broselow tape: 47%
Incorrect dosing:
Epinephrine: 68-73%
Diazepam: 47%;
Midazolam 60%
70
61
60
49
50
40
30
20
10
0
2012
2013
16
16
16
14
12
12
12
10
10
8
8
6
2012
5
4
4
4
4
3
2
2
3
2
1
2
1
0
0
2013
4
0
1
0
0
0
We continue to see confusion with dosage
calculation
1mcg/kg first dose (max 100mcg)
25mcg every 10 minutes if needed – max total
300mcg
Goal is to reduce confusion
Protocol committee looking at other
potential COG changes
Most providers have memorized the five
rights of medication administration
Right patient, Right route, Right dose, Right
time and Right medication.
These 5 “Rights” focus mostly on
individual performance.
System-wide issues may impact the ability
for providers to perform the 5 “Rights”
Standardization in medication administration
procedure
Use of memory aids and checklists
Risk-reduction strategies to minimize
opportunities for error
Medication storage and packaging
Redundancies and independent backups
Team-work crosscheck
Performance improvement team actively
working in identifying additional ways to
eliminate medication related events in our
system
More information to come with 2015 COG
update.
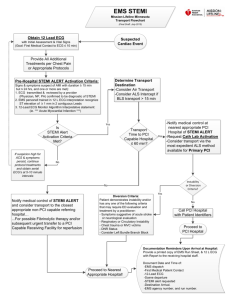
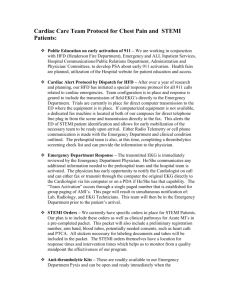
STEMI Update
Cardiac Arrest Update
Clinical Performance Indicators
Clinical Audits (Surveillance)
Performance Improvement
Activities
17,730 PCR’s reviewed (2013)
560+ calls DMO Line
211 clinical events
45% self report rate
Medical Director meetings
CY 2012 = 22
CY 2013 = 33
PCR’s Reviewed: (n=13,495)
Trauma Activations (n=181)
Stroke Activations (n=415)
STEMI Activation/Feedback (n=271)
ACS (n=2260)
Altered Mental Status (n=5550)
Seizure (n=3513)
Stroke (n=635)
Cardiac Arrest (n=670)
High Risk Low Frequency Events (n=4,025)
NTI (n=5)
OTI (n=22)
Surgical Airway (n=1)
Diltiazem (n=42)
Versed (n=605)
Fentanyl (n=3,000)
Tourniquet (n=13)
Pelvic Binder (n=3)
Needle Decompression
(n=13)
CPAP (n=305)
Pacing (n=24)
Cardioversion (n=5)
July-Dec 2013
DMO Activity
140
120
100
Count
80
60
40
20
0
2012
Level 1
41
Level 2
105
Level 3
62
Near Miss
1
Self Reports
92
2013
53
134
23
1
93
43, 801 STEMI PCI patients
Median D2B of 83 min (IQR 6-109 min)
Examined D2B time vs. Mortality
2005-2006; 600 US Centers
Consecutive Patients
No Transfers
No Pre PCI thrombolytic treatments
Analysis repeated excluding patients in shock
Analysis repeated using only D2B < 6 hours
•Limit Scene Time
•Identify STEMI early
•Activating the PCI team makes a
difference
Minimize on scene interventions
Shorten time-to-First 12-lead
Minimize total Scene Time
Remember prehospital STEMI Bundle
▪ ASA, 12-lead (activation), PCI Center (< 90 balloon)
▪ NNT = 15 Harm avoided: Stroke, 2nd MI or Death
84,625 in hospital arrests 2000-2009
79.3% AS or PEA
20.7% VF or VT
Survival to D/C 13% to 22.3%
Asystole and PEA survival about 13-14%
40% significant, 17% severe disability
VF / VT survival 40%
25% Significant, 8% Severe Disability
New Engl J Med 2012; 367:1917-20
AHA Consensus Statement addressing four
key areas:
Metrics of CPR Performance
Monitoring and feedback
Team-level logistics issues
Emphasis on CQI for resuscitation
Chest compression fraction (CCF),
Chest compression rate
Chest compression depth
Chest recoil (residual leaning)
Ventilation.
Goal is to maximize the amount of time chest
compressions generate blood flow
CCF is the proportion of time that chest
compressions are performed during a cardiac
arrest
Data on out-of-hospital cardiac arrest
indicate that lower CCF is associated with
decreased ROSC and survival
Chest
2013 Non-VF patients from ROC Network
64% Asystole, 28% PEA
Median Compression Rate: 110/min
ROSC 24.2%
2% Survival to D/C
Increasing CCF = ROSC
Target a CCF of 80%
89%
2013 CPR Compression Fraction (Median)
95
94
93
92
91
90
89
88
87
86
94
93
92
91
91
90
89
92
92
92
92
91
91 91
91 91
90
90
Manual
W/ Mechanical
90
91
90 90
2013 CPR Compression Fraction
(Average)
94
92
90
88
86
84
82
80
78
76
74
91 91
91 91
92
91
88
87 87 88
90 91 90
90
88
92
91
88
88
85
83
81
Manual
W/ Mechanical
As of January 2014
National
CARES
10.1%
* *Indicates incomplete quarter
The clinical measures presented above have been approved by
the EMS System Medical Director
National
CARES
30.8%
* *Indicates incomplete quarter
The clinical measures presented above have been approved by
the EMS System Medical Director
Clinical Performance Indicators
16:39
09:42
15:32
10:57
19:02
11:52
19 minutes on-scene, 10 minutes to first 12
lead.
NTG OS
23 minutes, 15 minutes to 12 lead,
19 minutes on-scene, 9 minutes to obtain12 lead
19 minutes, 5 minutes to 12 lead.
3 NTG on the scene prior to transport
15:35 on-scene, 10 minutes to 1st 12 lead
16 minutes on the scene, 6 minutes to the first 12 lead.
IV initiated prior to leaving the scene
96%
94%
94%
96%
D2B of ≤ 90 minutes now reads “an ideal of FMC -to-device
time. STEMI System goal of ≤ 90 minutes” (1B)
FMC of 120 minutes or less is new target for patients who
arrive at a non-PCI center (1B)
D2B now officially transitioning to “E2B”
88%
92%
Paul.hinchey@austintexas.gov
Jose.cabanas@austintexas.gov