WOUND CARE 8% Discuss the risks and contributing factors to
advertisement

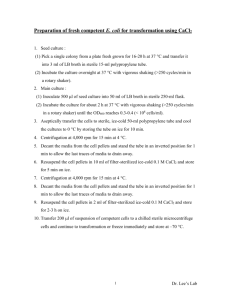
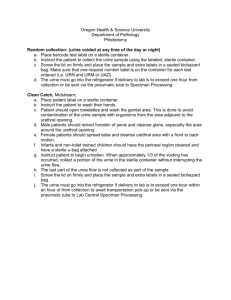
WOUND CARE 8% 1. Discuss the risks and contributing factors to pressure ulcer formation. Risk Factors- decreased mobility, decreased sensory perception, fecal or urinary incontinence, poor nutrition, LOC, shear, friction, moisture. o ** FYI: Unlike shear injuries, friction injuries affect epidermis. Contributing factors- a. pressure intensity 2. Pressure duration 3. Tissue tolerance o Pressure intensity: Pressure applied over a capillary exceeds normal capillary pressure/vessel is occluded tissue ischemia can occur. Blanching hyperemia: when skin turns lighter in color when pressure applied by finger on reddened skin, an attempt to overcome ischemic episode is occurring. Non-blanching erythema: color does not change. Possible deep tissue damage. o Pressure duration: Low pressure over prolonged period and high pressure over short period are two concerns r/t duration of pressure. o Tissue Tolerance: Ability of tissue to endure pressure depends on integrity of tissue. Greater the degree of which the factors of shear, friction, and moisture are present, more susceptible skin will be to damage from pressure. Also ability of underlying structures to assist in redistribution of pressure. 2. Describe complications of wound healing. Hemorrhage (bleeding from wound site) o If occurs after hemostasis (process of clotting) indicates a slipped surgical suture, dislodged clot, infection, or erosion of blood vessel by a FB. o Detect internal bleeding by looking for distention/swelling of affected body part, change in type and amt. of drainage, or signs of hypovolemic shock. o Hematoma: localized collection of blood underneath tissues o Risk of hemorrhage is greatest during 24-48 hours after surgery or injury. o S/S: low BP, high HR and RR, lethargy, bruising, swelling tender. Infection o Considered infected if purulent material drains from it. o Difference btw/ contaminated wounds and infected is amount of bacteria present. o Chances of infection are greater when the wound contains dead tissue, FB around wound, and blood supply and local tissue defenses are reduced. o Can show signs of infection w/in 2-3 days. Surgical wound infection doesn’t usually develop until 4-5th day o S/S: fever, tenderness/pain, elevated WBC, inflammation, drainage is odorous and purulent (can be yellow, green, brown depending on causative organism). Dehiscence (partial/total separation of wound layers) o PT at risk for poor wound healing is at risk for this. o To prevent place folded thin blanket/pillow over abdominal wound when pt is coughing. o 3-11 days post injury Evisceration (total separation of wound layers w/ protrusion of visceral organs) o Surgical emergency o NPO and place sterile wet towels over organs. o S/S: drainage, shock, high HR and RR, low BP 3. Complete an assessment for a patient with impaired skin integrity. Identifying those at risk. Braden scale (6-23 scoring; lower score is higher risk) o Includes areas for: sensory perception, moisture, activity, mobility, nutrition, and friction and shear. o Cut off score for onset of pressure ulcer risk is 18 4. Describe the differences between nursing care of acute and chronic wounds. Acute Care: prevent/manage infection, clean wound, remove nonviable tissue, manage exudate, maintain wound in moist environment, and protect wound. Heals by primary intention, use sterile technique (CANT delegate). o Require close monitoring Q8h o Prevent infection: clean only w/ non-cytotoxic wound cleaners like normal saline or commercial wound cleaners. These ARE NOT used in clean, granulating wounds. o Debridement: Mechanical (wet-to-dry, wound irrigation), autolytic (eschar digested by enzymes via special dressing-transparent film), chemical (topical enzyme prep, Dakin’s sol., sterile maggots), and sharp/surgical. o Maintain hemoglobin to 12g/100 mL Chronic: wound that fails to proceed through an orderly and timely process to produce anatomical and functional integrity. Clean technique (can delegate) o Causes: vascular compromise, chronic inflammation, repetitive insults to tissue. o Continued exposure to insult impedes wound healing. FYI Pressure Ulcer Staging: 1. Non-blanchable erythema (indicative of at-risk personnel). 2. Partialthickness skin loss or blister. (shallow open ulcer w/out slough) 3. Full-thickness skin loss (fat visible; muscle, tendon or bone NOT exposed). 4. Full-thickness tissue loss (muscle/bone visible). Granulation: good! Slough: yellow/white tissue must be removed for wound to heal. Eschar: necrotic tissue. Primary Intention: wound that is closed. Surgical incision. Skin edges are approximated. Heals quickly and by epithelializition. Secondary Intention: wound edge not approximated. Pressure ulcer, surgical wounds w/ tissue loss. Heals by granulation tissue, wound contraction and epithelialization. Heals w/ scar tissue. Serous drainage: clear, watery plasma. Purulent (infection): thick, yellow, green, tan. Serosanguineous (dehiscence): pale, pink watery, mix of clear and red fluid. Sanguineous: bright red, indicates active bleeding. Influence wound healing: nutrition (1500 k/cal daily and vitamin A and C), tissue perfusion (DM), age (slower inflamm. response, etc.), infection (prolongs phases). Look for reactive hyperemia (inc. blood flow to ischemic tissue) indicative of pressure ulcer formation; reassess after one hour. When cleaning incontinent pt use nonionic surfactants, and ensure skin is moisturized but not over saturated. Elevating bed to thirty degrees or less decreases chance of pressure ucler dvpt. NEVER MASSAGE REDDENED AREAS. Hydrocolloid dressing: maintains moist healing env. Supports healing in granulating wounds and debrides necrotic wounds. Acts as a preventative dressing. Hydrogel: soothing and don’t adhere to wound bed. Debrides necrotic tissue. STERILE TECHNIQUE 8% 1. Describe 7 principles of surgical sepsis. A sterile obj remains sterile only when touched by another sterile object. Only sterile objects may be placed on a sterile field. A sterile obj or field out of the range of vision or an obj held below a person’s waist is contaminated. Sterile obj or field becomes contaminated by prolonged exposure to air. o Avoid activities that create air currents. When a sterile surface comes in contact w/ a wet, contaminated surface, the sterile obj or field becomes contaminated by capillary action. Fluid flows in the direction of gravity. o Sterile obj becomes contaminated if gravity causes a contaminated liquid to flow over the surface of the object. I.e. hold hands above elbows for surgical hand scrub. The edges of a sterile field or container are considered to be contaminated. (1 inch/2.5 cm) 2. Describe the procedure to open a sterile package with attention to the principles of surgical asepsis. CANT BE DELEGATED TO NAP Open outer most flap away b/c reaching over sterile field contaminates it. 3. Describe the process of open gloving using surgical asepsis. When gloving second hand, slip fingers underneath cuff b/c sterile touching sterile prevents glove contamination. After second glove is on, interlock fingers, hold away from body at waist level. 4. Describe preparation of the sterile field including proper technique for pouring fluids. Verify contents and expiration date. Remove sterile seal and cap in an upward motion to keep inside of cap sterile. Lip 1-2 inches from container when pouring. Pour slowly. Neck of bottle is contaminated. Hold bottle edge outside of sterile field. OXYGENATION (17%) *Oxygen therapy is given at lowest possible O2 sat. to achieve 95-100% SaO2 level w/out complication. 1. SEE OTHER STUDY GUIDE 2. Assess for the physical manifestations that occur with alterations in oxygenation. Inspection: o LOC, general appearance, systemic circulation, breathing patterns, and chest wall movement. o Clubbed nails: chronic hypoxemia. o Retraction: sinking in of soft tissues of the chest btw/ IC spaces. o Kussmaul respiration: metabolic acidosis. Inc. rate and depth of RR r/t dec. oxygen levels. o Cheyne-strokes respiration: dec. blood flow/injury to brainstem. Periods of apnea followed by periods of deep breathing, and then shallow breathing followed by more apnea. o Barrel shaped chest. Palpation: o Peripheral pulses, cap refill, color. o Edema: +1-+4 ABNORMALITIES: o Pursed lip breathing: chronic lung dz o Distention: right-side HF 3. Identify nursing care interventions in the primary care, acute care, and restorative and continuing care settings that promote oxygenation. Primary Care: o Prevention of RI is optimal o Vaccine: flu vaccine recommended for 6 mos and older o Healthy Lifestyle o Env. Pollutants: avoiding secondhand smoke Acute Care: o Dyspnea mngmt o Airway maintenance: adequate hydration and proper coughing tech. o Mobilization of pulmonary secretions o Hydration: keeps secretions thin. 1500 to 2500 mL/day o Humidification: Temp is the MOST important factor affecting amount of water vapor a gas can hold. NECESSARY for pt receiving O2 therapy > 4 L/min o Nebulization o Coughing and deep-breathing tech: Cough ATLEAST Q2h; large amount cough Q2h-Q3h; post-surgery cough Q2h-Q4h Directed coughing: good when random coughing fails o Chest physiotherapy: postural drainage, chest percussion, and vibration. Recommended for those producing >30mL of sputum daily or atelectasis o **Check Annabeth’s study guide for Pos. for postural drainage. Restorative and Cont. Care: o Cardiopulmonary rehab includes: physical exercise, nutrition counseling, relations and stress-mngmt tech, and prescribed meds. o Resp muscle training o Cough techniques 4. 5. 6. 7. 8. 9. Cascade: takes deep breath and holds for 2 secs. while contracting diaphragm. Performs coughs during exhale. Good for large amounts of sputum. Huff: natural cough reflex. Good for clearing central airways. Quad: abdominal muscle issues. Pt breaths out w/ max effort and RN pushes on abdomin. o Pursed-lip breathing o Diaphragmatic breathing: relax intercostal muscles with deep inspiration. Develop a plan of care for a patient with altered need for oxygenation. Differentiate btw/ different oxygen masks. Two types: those delivering low concentrations and those delivering high concentrations. o Simple face mask: short term O2 therapy, FIO2 35-50%, 5L or more (to avoid rebreathing of CO2, needs high O2 level to prevent rebreathing of CO2. Contraindicated in pt w/ CO2 retention o Plastic face mask w/ reservoir bag: higher concentration of O2, Partial rebreather mask (type of simple face mask): resivoir bag should be at least 1/3 to ½ full on inspiration, 40%-70% FIO2, 6 to 10 L/min. Can be used as a non-rebreather mask: prevents exhaled air from returning into reservoir bag, min. of 10 L/min, FIO2 60-80%. ** IF DEFLATED MEANS BREATHING IN EXHALED CO2. High flow systems need to be humidified o Venturi mask: higher oxygen concentrations of 24-60%, 4-12 L/min, doesn’t dry mucous membranes, delivers humidity w/ O2 concentration. Ensure fits properly, if not can deliver decreased FIO2. Identify 3 parts of a tracheostomy tube. Outer Cannula: keeps stoma open, DON’T REMOVE, may be secured w/ trach ties. Inner Cannula: can be removed for cleaning, can be disposable Obturator: used for trach insertion, ALWAYS KEEP AT BEDSIDE in event of accidental trach dislodgement. Identify clinical indications that suggest the need for oral or tracheal suctioning. Based upon physical assessment: inc RR, HR, BP, dyspnea, dec SaO2, pallor/cyanosis, and behavior Assess secretions: nasal, drooling, gastric/vomit in mouth. Auscultate: adventitious breath sounds **Q1-Q2h suctioning is BAD leads to..: cardiac arrhythmias, hypotension, hypoxia, airway trauma. OTHER STUDY GUIDE Explain sterile open tracheal suctioning and tracheostomy care. -Trach Suction CANT BE DELEGATED Best time to insert catheter is upon inspiration. Go down until you meet resistance, or pt coughs. Then pull back 1 cm (1/2 inch). o Pulling back stimulates cough and removes catheter from mucous wall. *App of suction while insertion inc. risk for damage of mucosa, inc. hypoxia r/t removal of O2 in airways. *Intermittent suction and rotation prevent injury to trach mucosa. *Bag-valve expands alveoli. 120-150 mm Hg for suctioning, normal saline instillation is BAD. Open suctioning: new sterile catheter for each suction session. -Trach Care: performed every 8-12 hrs. Indications: soiled/loose trach ties or trach dressing, unstable trach tube, and excessive secretions. CANT BE DELEGATED Cotton-tipped swabs X2, pour NS over one. Open trach kit. Two 4x4 gauze. Pour NS over one. Don’t recap NS Pour NS into sterile basin, and place sterile brush inside Open trach package. Length of twill tape is 60-75 cm (goes around neck 2X). Put on sterile gloves Hyper-oxygenate Remove inner cannula and place in NS basin. Place oxygen source over outer cannula. Clean inner cannula and replace. W/ gauze clean exposed outer cannula and stoma under faceplate extending 5-10 sm in all directions from stoma. Use cotton swab to clean. FWD: tie trach w/ double square knot method Insert clean dressing under faceplate. FYI Tidal volume: amt of air exhaled after normal inspiration Residual volume: amt of air left in alveoli after full expiration. Hypovolemia: reduced circulating blood volume r/t sig fluid loss causing vasoconstriction, inc HR and cardiac output Hypoxia: inadequate tissue oxygenation. Dec Hemoglobin level and lowered oxygen carrying of blood. Diminished concentration of inspired oxygen Inability of tissues to extract oxygen from blood Dec diffusion of oxygen from alveoli to blood (pneumonia) Poor tissue perfusion with oxygenated blood (shock) Impaired ventilation (chest trauma) S/S apprehension, restlessness, inability to concentrate, decreased level of consciousness, dizziness, and behavioral changes. Orthopnea: pt uses pillows when reclining to breath. Hemoptysis: bloody sputum Mobilizing secretions dec. pt hospital stay (: Awake pt at night to cough every 2-3 hrs if have chronic resp dzs. Safety Precautions for O2 therapy Must be prescribed, and adjust w/ provider orders. “oxygen in use” sign. Keep 10 ft from flames Equipment is functioning Store O2 cylinders upright and secured. Check O2 tanks before transporting. Nasal Cannula: precise O2 delivery, up to 6 L/min, must humidify if greater than 4L/min Urinary Elimination, Chapter 45 (17%) 1. Identify factors that commonly influence urinary elimination. Disease conditions- Dec. blood flow to and through the kidney (pre renal), dz cond of renal tissue (renal), and obstruction in lower urinary tract that prevents urine flow from kidneys (post renal). o DM and neuromuscular dz: change in nerve functions leading to loss of bladder tone, reduced sensation of bladder fullness, or inability to inhibit bladder contractions. o Irreversible kidney damage: uremic symptoms (n/v, fluid retention) needing dialysis. Sociocultural: degree of privacy Psychological: anxiety prevents pt from urinating completely. Difficulty relaxing muscles Fluid Balance o Nocturia: sign of renal alteration o Polyuria: excess output o Oliguiria: urine output dec. o Anuria: no output o Diuresis: urine formation o Intake of coffee, tea, cocoa, and soda inc. need to urine. o Febrile causes dec urine production. Surgical procedures o Anesthetics and narcotic analgesics slow glomerular filtration rate, and reduce urine output. Meds & Diagnostic Exam 2. Compare and contrast common alterations in urinary elimination. Most pt unable to store urine/ fully empty the bladder usually r/t impaired bladder function, obstruction to urine outflow, or inability to voluntarily control micturition. Urinary retention: accumulation of urine resulting from inability of bladder to empty properly. As RN watch for volume and freq of voiding to assess for this! o *normally bladder slowly fills w/ urine until distends to certain level, and micturition reflex occurs. Bladder will empty completely o UR bladder is unable to respond to micturition reflex and is unable to empty. Pt can feel need to urinate but cant. o Overflow will occur and sphincter will release small volume of urine. o Small amts q2h-a3h w/out relief o Residual urine occurs if pt has UR or can’t empty bladder all the way. UTI o 80% from indwelling cath. (CAUTI) Each day cath in place 5% inc in bacteria in urine. o CAUTI mostly caused by pt’s own E.Coli o Bacteruria leads to organisms in kidneys and bacteremia (bacteria in bloodstream). o Women are MOST susceptible d/t short urethra and proximity of anus. o Men’s prostatic secretions reduce susceptibility. o S/S dysuria, fever, chills, vomiting. o Dysuria: pain on urination o Cystitis: irritated bladder causing urgent sensation to void o Hematuria: blood in urine. Urinary incontinence: involuntary leakage of urine. o Urge/stress incontinence: incontinence r/t to urinary causes. Urge: involuntary passage of urine after strong sense of urgency to void. S/S: urgency Stress: Involuntary leakage of urine during inc. abdominal pressure in absence of bladder muscle contraction. S/S loss of urine w/ inc. intraabdominal pressure (coughing, laughing, etc). o Functional: loss of urine caused by factors outside urinary tract that interfere w/ ability to respond in a socially appropriate way to the urge to void. S/S urge to void causes loss of urine before reaching appropriate receptacle. o Overflow Incontinence: involuntary loss of urine w/out sensation to void S/S lack of urge to void, unawareness of bladder filling R/T spinal cord dysfunction o Hyperactive/Overactive bladder: urgency associated w/ urinary freq. and nocturia. S/S sudden desire to urinate that is difficult to deter. Urinary diversions: diversion of urine to external source d/t injury to bladder or CA etc. o Continent urinary reservoir: created from distal portion of ileum and proximal portion of colon. Ureters embedded in reservoir. Cath pouch 4-6 X’s daily. o Orthotopic neobladder o Nephrostomy to drain urine directly from kidneys o **refer these pt to osotomy RN (: 3. Obtain a nursing history for a client with urinary elimination problems. Patterns of urination: freq., normal volume, recent changes. NL void 5 X a day Symptoms of urinary alterations Factors affecting urination (i.e. env. Factors, med hx, psychological, muscle tone, fluid balance, surgical/diagnostic procedures, and dzs) 4. Identify nursing diagnoses appropriate for clients with alterations in urinary elimination. (BOOK) 5. Explain how to obtain urine specimens. CAN be delegated Random (routine urinalysis): collect during nl voiding. NOT from indwelling cath bag. Clean-voided/midstream (culture and sensitivity) *Sterile Technique o Female: Spread labia and clean area Have pt initiate stream, after stream has started pass container into stream collecting 30-60 mL (initial stream flushes microorg.) o Male: Clean in circular motion *same o Remove container before flow of urine stops and before releasing labia/penis (could be contaminated by skin flora) Sterile specimen (C&S): collect from indwelling cath port in drainage tubing (3-5 mL) Timed specimen o First voided discarded o Last void included 6. Discuss nursing measures to promote normal micturition and reduce episodes of incontinence. Micturition: discharge of urine. Age impairs-men prostate enlrgmt-women loss of estrogen. Often occurs from muscle wasting caused by immobility, damage during childbirth, obesity, caffeine, muscle atrophy r/t menopause, trauma. Help pt assume normal pos for voiding! Sensory stimuli o Sound of running water o Stroking inner thigh stimulates sensory nerves o Pour warm water over perineum Kegel exercises (pelvic floor exercises): helps w/ stress/urge urinary incont. Bladder retraining: reduce voiding frequency and bladder capacity. For pt who have dec urge to void (dribbling) o Use urinary diary o 2 or more weeks to learn o Supresses urination and inc. time by increments of 15 mins weekly o Goal to void q3h-q4h in volumes of 240-500 mL o May include toilet schedule Habit training: functional incontinence; improves voluntary control over urination. o Toilet schedule Self-Cath: cleen-versus-sterile tech. o Self-cath 4-6 X’s daily in volumes of 400-500 mL 7. Discuss nursing measures to reduce urinary tract infection. Perineal hygiene that includes cleaning urethral meatus after each void and BM. 3X a day if have a catheter. Minimal daily intake of 1200-1500 mL (flushes urethra of microorg.) if have catheter 2000-2500 mL Voiding after sex Not taking bubble baths Wear cotton underwear Intake of fluids high in acid ash (apple/cranberry juice) Closed drainage system: don’t raise cath bag above bladder. o Don’t allow spigot to touch contaminated surface o Don’t touch ends of cath tubing if dislodged o Drain all urine from tubing into bag before ambulation o Avoid prolonged kinking/clamping o Empty min. Q8h 8. Instruct client directions for proper condom catheter application. For incontinent or comatose men who still have complete and spontaneous bladder emptying. Worn only a night or continuously CAN be delegated Needs a provider’s order Pt supine or sitting pos, clean perineal area. *Shaft must be 2 cm for proper application. Smoothly roll down allowing 2.5-5 cm of space btw/ tip of penis and end of cath. Secure o Elastic adhesive- use spiral tech to wrap around over condom (DON’T USE ADHESIVE TAPE) o Self adhesive- apply pressure for 10-15 secs 9. Discuss proper urinary catheter insertion and care Insertion Requires provider’s orders. CANT be delegated Cath size 14-16 Fr for most pt. Pretesting the balloon by injecting fluid into port is no longer recommended. May distort or stretch balloon causing damage and trauma upon insertion. Read manufacturer’s label to see if it was pre-tested. Proabably will meet resistance on male. Have take slow deep breaths, and continue past prostatic sphincter. Care Female: dorsal recumbent pos., retract labia, clean around (avoid getting soap in urethra) with soap and water Male: supine or fowler’s, retract foreskin, clean in circular motion *Application of antimicrobial products in not effective in reducing UTI, don’t include them Remove anchoring device Clean length of cath tubing in circular motion up to 4 inches. Reanchor FYI Nl output 1200-1500 mL/day. Output less than 30 mL/hr indicates possible circulatory blood volume or renal alterations. Bladder capacity is 600-1000 mL. Adult voids q2h-q4h Reflex incontinence: damage to spinal cord above sacral region results in loss of voluntary control of urination. Hyperreflexia: life threatening prob that affects HR, and BP caused by overly full bladder. Dark Amber urine result of inc. concentrations of bilirubin r/t liver dysfunction. Encouraging pt to wait until urine stops flowing or to attempt to void again (double voiding) can improve bladder emptying. Older men often suffer from inhibit bladder contractions (BPH), makes them prone to urinary retention and incontinence. Though they are PRONE to incontinence, doesn’t mean it is a NORMAL aging process. Restricting fluid intake does NOT dec. urinary incontinence severity or freq. Also need to note high volumes of urine 2000-2500 mL daily How long caths can be remained indwelling Plastic: intermittent r/t inflexibility Latex/rubber: up to 3 weeks Pure silicon/teflon: 2-3 mos. Nutrition, Chapter 44 (8%) 1. Apply the nursing process to a client with dysphagia and risk for aspiration. S/S: cough during eating, change in voice tone or quality after swallowing, abnormal movements of the mouth, tongue, or lips; and slow, weak, imprecise, or uncoordinated speech. Silent aspiration: occurs in pt w/ neurological probs that lead to dec. sensation. Occurs w/out cough. Precautions: o Dysphagia screening: there are diff tools o Perform oral hygiene before meals: risk of aspiration pneumonia is associated w poor oral hygiene o Inspect mouth for pockets of food. o Position: 90 degree angle, head is flexed slightly forward. o Observe w/ diff. consistencies of food. o Place 1/2 to 1 teaspoon on unaffected side of mouth. o Place hand on throat to gently palpate swallowing to evaluate swallowing effort o Provide verbal coaching: open mouth, feel for food in your mouth, chew and taste the food, etc. o Provide periods of rest o Pt remain sitting upright for 30-60 mins after meal: allows food in pharynx to clear Dysphagia Diet Levels: o Dysphagia puree o Dysphagia mechanically altered o Dysphagia advanced o Regular Levels of liquids: o Thin liquids (low viscosity) o Nectar-like liquids (medium viscosity) o Honey-like (viscosity of honey) o Spoon-thick (viscosity of pudding) 2. Discuss EBP to determine NG tube feeding tube placement. Injection of air is ineffective in detecting tubes placed in lungs. Addition of blue food coloring to assist w/ detection of formula aspirated into lungs is no longer used. Glucose method no longer used. Measurement of pH of secretions withdrawn from feeding tube helps to differentiate the location of the tube. (CANT be delegated) o Intermittently fed: test immediately before feeding and after 4 hrs of past feeding. o Inject 30 mL of air. Flush w/ 30 mL o Cont. tube fed: test placement q4h-q6h. If pt is tolerating feedings and correct location on tube exit site it has remained in original pos. it is reasonable to cont. feedings. o Wait an hr. after med. admin. o Obtain 5-10 mL of gastric aspirate. o pH should be less than 4 if greater than 5.5 it is associated w/ respiratory excretions Nasointestinal: >6 Cont. feeding: >5 **<7 Acidic Most reliable is x-ray film. 3. Describe the methods to avoid complications of enteral feedings *Typically starts at full strength at slow rates. Inc hourly rate q8h-q12h per provider’s order if no signs of intolerance appear. S/S of intolerance: high gastric residuals, nausea, cramping, vomiting Serious compmlication is aspiration of formula ito tracheobronchial tree resulting in necrotizing infection, pneumonia, and potention absess formation. To reduce complications: o Keep bed elevated to 30 degrees (45 preferrable) o Measure gastric volume q4h-q6h reciving cont. feeding and before feeding in intermittent feedings. o Delayed gastric emptying (risk for aspiration): if 250 mL or more remains in stomach on two consecutive assessments each 1 hr aart or if a single measurement exceeds 500 mL. NAS on Aspiration recommends: o Stop feeding if aspiration occurs o w/hold feedings and reassess pt tolerance to feeding if GRV is over 500 mL o reevaluate for aspiration periodically o Use RN measures to reduce risk of aspiration if btw/ 250-500 mL Complications: o Pulmonary aspiration: verify tube placement, high fowlers during feeding and 2 hrs after. o Diarrhea: Change formula rate/dilute, don’t hang formula longer than 4-8 hrs in bag and change tubing/bag q24h. o Constipation: from lack of fiber/free water or inactivity o Tube Occlusion: Irrigate w/ 30 mL, use liquid meds when available o Tube displacement: Replace tube and confirm placement. o Abdominal cramping, N/V: Suggest isotonic formula, lower rate of delivery to inc. tolerance, HOB 30 degrees. From lactose intolerance, intestinal obstruction (stop feeding), high-fat formula, cold formula used. o Delayed gastric emptying o Serum electrolyte imbalance o Fluid overload o Hyperosmolar dehydration. 4. Discuss the administration of enteral feedings via nasoenteric, gastrostomy or jejunostomy tubes (Skill 44-3) Enteral tube feedings: administered into stomach or intestines via tube inserted through nose or a percutaneous access. Supplement pt oral nutritional intake when they cannot meet their nutritional needs by mouth. **Parenteral nutrition: pt who cannot tolerate nutrition via GI tract. Solutions consist of glucose, amino acids, lipids, minerals, via indwelling peripheral or central venous catheter. Pt w/ low risk of GERD receive gastric feedings; however, if risk of GERD (which leads to aspiration) receive jejunal feeding. Flush line w/ small amount of water to ensure tube patency Admin of EN feedings: o CAN be delegated o Auscultate o for BS before starting b/c could indicated decreased ability of GI tract to digest/absorb nutrients o Set up set via aseptic technique. o Shake formula and cleanse top w/ alcohol swab, and pour into bag and hang on pole. o Place pt in high-folwers pos. o Verify tube placement Nasoenteric: x-ray or pH Gastrostomy tube: aspirate gastric secretions, check pH (1-4) Jejunostomy tube: intestinal secretions and check pH (not acidic) o Check GRV Intermittent: before feeding and q4h Continuous: q4h-q6h Draw up 10-30 mL, inject into tube, aspirate all contents. Return contents unless exceeds 250 mL o Flush w/ 30 mL of water o Initiate feeding: o Syringe for intermittent: Pinch proximal end of tube to prevent air from entering Remove plunger from syringe Fill syringe w/ formula, release tube, and elevate syringe no more than 45 cm above insertion site and allow gravity to take over to reduced abdominal discomfort. o Bag for intermittent: Attach feeding bag tubing to end of feeding tub. Set rate via roller clamp to reduce air intro. into stomach. Bag empty over 30-45 mins via gravity to reduce abdominal discomfort. Change bag q24h o Cont. drip method: Attach admin set tubing to end of feeding tube. Insert tubing through infusion pump and set rate. o Advance rate as ordered to prevent diarrhea and gastric intolerance. o Flush w/ 30 mL q4h for cont. feeding, and before and after intermittent feeding. o When feeding not being admin, clamp proximal end of feeding tube. FYI Vitamins are organic substances. Fat-soluble: A D E K; Water-soluble: C and B complex Minerals are inorganic. Intestine is primary area of absorption. Longer material stays in large intestine, the firmer the feces. Small intestine primary site for absorption of nutrients. Enzymes work at specific pH; starch digestion occurs in mouth *If EN therapy is less than 4 weeks, nasogastric or nasojejunal feedings may be used. *If more than 4 wks surgical or endoscopically placed tubes are preferred to reduce discomfort of nasal tube. Bowel Elimination, Chapter 45 (8%) 1. List nursing measures that promote normal elimination. Almost impossible to contract muscles in supine pos. for defecation, raise HOB Teach pt and family about proper diet, adequate fluid intake, and factors that stimulate or slow peristalsis (i.e. emotional stress). Most imp habit is to TAKE TIME for defecation Raise HOB when pt using a bedpan because supine will result in hyperextension of hips Offer bedpan often Offer elevated seat for toilet to minimize risk of falls. Small fracture pan: lower extremity fractures; shallow fits under buttocks and deeper w/ handle goes under upper thighs 2. List nursing measures included in bowel training. Involves setting up a daily routine by attempting to defecate at the same time each day. Includes: o Choosing time for defecation o Giving stool softeners o Offering hot drinks or fruit juices o Helping pt to toilet o Avoiding opioids that increase constipation o Providing privacy and setting a time limit (15-20 mins) o Have pt lean forward at hips, apply manual pressure w/ hands over abdomen, and bear down but not strain. o Exercise in general and of weak abdominal and pelvic floor muscles: Lie supine, tighten abdomen for three seconds. Repeat 5-10 X’s Flex and contract thigh muscle by raising knee to chest. Repeat w/ each leg at least 5 X’s o Diet: Const. inc. high-fiber foods and fluids. Diarrhea inc. low-fiber foods and avoid foods that cause gastric upset. o Management of hemorrhoid pain via sitz bath or ice pack. 3. Discuss nursing care measures required for clients with a bowel diversion. Ostomies: location determines consistency o RN teaches coping w/ and r/t self-esteem and body image issues. o RN freq assess of fecal drainage, character of feces, appearance and cond. Of stoma, type of fecal collection device used, and methods to maintain function of ostomy. o Care of: irrigation of left-sided ostomies to regulate colon emptying Only colostomies can be irrigated Never use enema, use special cone-tipped irrigator to prevent bowel penetration and backglow. Have pt sit on toilet and place irrigating sleave over stoma and end into commode Provider’s orders state amount and tpe of irrigation. Pt waits 30-45 mins after irrigation for feces to drain. o Watch for skin breakdown. o Assess stoma and ensure it is bright pink or brick red. o Nutritional Considerations: Low fiber: bread, noodles, rice, cream cheese, eggs, straigned fruit juices, lean meats, fish and poultry. Eat slow and drink 10-12 glasses of water daily to prevent blockage. 4. Instruct nursing assistant proper method of administering a cleansing enema Cleansing enemas promote complete evacuation of feces from colon through infusion of a large volume of solution or through local irritation of the mucosa of the colon. High and low refer to height and pressure the fluid is delivered o High enemas cleanse entire colon. 12-18 inches o Low enema cleanses only rectum and sigmoid 12 inches o After enema is infused, pt turn from left lateral to dorsal recumbent, to right lateral position. Include: o Tap water: hypotonic and exerts osmotic pressure lower than fluid in interstitial spaces. Stimulates defecation. Watch for water toxicity o Normal saline: Safest b/c exerts same osmotic pressure. Stimulates peristalsis. No danger of excess fluid absorption. ** infants and children receive only NS b/c at risk for fluid imbalance. o Hypertonic (Fleet enema): hypertonic and exerts pressure pulling fluids out of interstitial spaces resulting in distention promoting defecation. Low volume. Contraindicated in infants and those who are dehydrated. o Soapsuds: Intestinal irritation to stimulate peristalsis. Only pure castile soap. Administration: o Can delegate but CANT if there is medication o Sterile technique is unnecessary. o No more than three enemas. o Don’t give w/ pt on toilet can scrape rectal wall. o Order is required o Put pt in left side-ling w/ right knee flexed. Allows sol to flow downward via gravity b/c of natural cure of sigmoid and rectum. o Enema bag Add warmed solution to bag. Raise container and release clamp to remove air from tubing; then reclamp Lubricate 2.5-3 inches. Insert about 3-4 inches. Hold tubing in rectum until end of fluid instillation. Open clamp and allow sol. To enter. Raise height of enema slowly Clamp once instilled. o Prepackaged disposable: Already lubricated, insert. Squeeze bottle until all solution has enetered rectum. Retain sol. Until defecation occurs (2-5 mins). o –Assist pt to bedpan/toilet. 5. Insert and maintain a nasogastric tube for gastric decompression Small bore is for feeding Large bore is for decompression (removal of gastric secretions). Include Levin and Salem sump tubes. o Salem sump: preferred. Has two lumina; one for removal of gastric contents and one to provide an air vent. NEVER clamp, connect, suction, irrigate air clamp. o Levin tube: single lumen w/ holes near tip. Purpose of decompression is to keep GI tract free of secretions, reduce nausea and gas, and dec risks of vomiting and aspiration. INSERTION: o CANT be delegated o Prepare equip. and cut tape 4 inches long and cut one end in shape of V o Pos. pt in high-fowlers pos. o Instruct pt to relax while occluding one nares. Determines which is more patent for insertion. o Measure distance Tip of nose to earlobe to xiphoid process OR mark 20 inch point on tube and measure traditionally. Tube insertion is at midway point btw/ 20 inches and traditional mark. o Mark measured distance o Curve 4-6 inches of end of tube tightly around index finger to decrease tube stiffness o Lubricate 3-4 inches o Pt extend neck against pillow and instruct slowly through naris aiming downward. o Do not force against continued resistance. o Stop tube advancement above oropharynx and allow pt to relax. o Ask pt to flex head forward, swallow, advance tube 1-2 more inches with each swallow. o Ensure placement o After inserted connect to drainage bag or suction o Tape tube to nose by wrapping V end around tubing. o Fasten to gown by looping rubber band in slipknot and pin rubber band to gown. o Elevate HOB to 30 degrees to prevent esophageal reflux o When placement is confirmed place red mark to indicate where exits nose. o Tube irrigation: 30 mL of NS Disconnect NG tube from suction, etc. and clamp Insert syringe and unclamp and inject slowly to avoid gastric trauma. Turn pt onto left side. After instilling, immediately aspirate to w/draw fluid. Amount greater than instilled- difference is output Amount less than instilled-difference is intake **irrigating solutions count as intake FYI Observable peristalsis is often a sign of intestinal obstruction. Esophagus-cardiac sphincter-stomach-duodenum-jejunum-ileum-ileocecal valve-large intestine (ascending, transverse, descending, sigmoid / cecum, colon, rectum). Pt w/ CVD, ICP, and surgical wounds risk for cardiac dysrhythmias and elevated BP r/t Valsalva maneuver and need to avoid. Stress increases digestive process, whereas depression slows down resulting in constipation. Common Problems: Constipation: S/S BM less than every 3 days, excessive straining, hard feces. Impaction: unrelieved constipation. Feces wedged in rectum. Suspected if cont. oozing of diarrhea stool occurs. Diarrhea: dvpt of fluid and electrolyte imbalance. Hemorrhoids: dilated, engorged veins in rectum. Fecal Incontinence: mentally alert but physically unable to avoid defecation.