You want us to do WHAT? - Maryland Patient Safety Center
advertisement
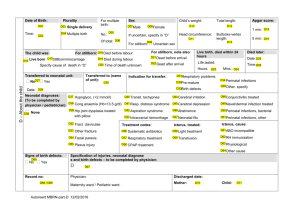
You want us to do WHAT? Perinatal & Neonatal Learning Network December 3, 2013 Jennifer Ustianov MS RN IBCLC Perinatal Content Lead NICHQ Objectives • Outline the case for widespread use of maternal and neonatal risk assessment tools • Describe how the use of Improvement Science can assist implementation within an existing system of care • Plan the tasks and first test of change for implementing the widespread use/adoption of risk assessment tools Why me? Leadership Introspection Why now? Maternal and Neonatal risks What was learned in 2012? • Over 30% of maternal and infant discharges had identifiable risk • Member hospitals have very good processes for getting patients out of the hospital • Significant numbers of patients with risks were not identified for the specific intervention of early post-discharge evaluation Why not now? Creating the Case • Insert updated MD stats on neonatal and maternal outcomes Key Elements of Breakthrough Improvement Will to do what it takes to change to a new system Ideas on which to base the design of the new system Execution of the ideas Factors which effect the Will to change • • • • • Need and urgency for change Life experiences Positive and negative experience Personality Resources and Support Ideas: bases for design of new system Ideas come from: • Strong evidence • Good knowledge (our own or others) • Hunches • Open, supportive and agile team-based environments Execution of the ideas • • • • • • • • • Tap on expertise Multidisciplinary planning team Use tools and methods tested by others. Test, Study; Test, Study; Test, Study. Leadership support. Identify and remove barriers and old way. Illicit involvement and feedback. Embrace grumbling as an opportunity. Remember: with true change comes learning Model for Improvement Three Fundamental Questions for Improvement 1. What are we trying to accomplish? 2. How will we know that a change is an improvement? 3. What changes can we make that will result in improvement? PNN and the Model for Improvement (MFI) What are we trying to accomplish? Project Aim How will you know change is an improvement? Measurement Strategy What change can we make that will result in improvement? Workplan Test and Implement Perinatal & Neonatal Risk Assessment Aim Statement Our aim is to improve communication between hospitalbased and community –based providers and between hospital staff and families through standardization of the discharge process for mothers and babies, including the late pre-term infant. Success will be measured through both process and outcome measures Aim Model for Improvement By June 2014 the Neonatal Risk Assessment Tool will be implemented What are we trying to accomplish? How will we know that a change is an improvement? What change can we make that will result in improvement? TESTING Tasks: •Data collection: How, who, when to collect data •Design flags in EHR •Identify community referral network •Create audit tool •Education of ALL staff •Celebrate wins MEASURES Outcome: 95% of neonates with identified risks will have documented appropriate referrals Process: 80% of new admission will have a completed neonatal risk assessment within 24 hours Tests: P: Patti RN will use the Risk Assessment Tool for the first admission D: Patti was too busy to implement –critical ca S: No assessment done in first 24 hours Edit/Act: Next test will include communication to next shift re whether assessment was completely Making it Happen for Improved Outcomes Team Planning • Draft Aim statement • Draft one Outcome Measure • Draft one Process Measures P-D-S-A Cycles • A way to turn Ideas into Action (P D) • A way to connect Action to Learning (S A) Using PDSA cycles to learn our way through improvement A P S D A P S D A P S D 4. Implementation testing A few providers, varied shift/time of day 3. More wide-spread tests A few providers, one shift/time of day 2. Then do f/u test over a variety of conditions to understand scalability and identify weaknesses One provider, different shift/time of day 1. Early tests are simple and designed to learn then One provider, one succeed shift/time of day AIM Concept D Concept A Concept C Concept B Change Concepts, Theories, Ideas PDSAs Why Testing • Increase belief that the change will result in improvement – dealing with uncertainty – dealing with skeptics/ minimize resistance upon implementation • Opportunity for “failures” without impacting performance • Get idea of how much improvement can be expected from the change • Learn how to adapt the change to conditions in the local environment • Evaluate costs and side-effects of the change Risk Assessment Tool • Started at admission to capture pre-existing risk factors • Continued through admission to capture new onset risks • Framework for education, counseling, consultations, and discharge referrals • 1 tool to capture risk and coordinate care Eight Step To Change Overview of Kotter’s Points, 1995 1. Establish a sense of urgency RISK: Based on market, competitive, social, performance (etc.) realities, the change must be seen as critical to organizational survival/success Not Sufficiently Compelling !!! 2. Form a powerful guiding coalition Not A Credible/ Cohesive Team !!! Assemble a leadership group with enough commitment, credibility, influence, and authority to lead, model, and sustain the change effort 3. Create a Vision A clearly stated “higher” vision that speaks powerfully to participants and personally spurs them to “go the extra mile” RISK: RISK: Vague, Insufficient Motivation !!! RISK: 4. Communicating the Vision Use multiple vehicles and venues to communicate the new vision/strategies Teach new behaviors by the example. Less than Over-Comm by Factor of 10 !!! Overview of Kotter’s Points, 1995 5. Empower others to act on the vision Get rid of obstacles; Change systems /structures that seriously undermine the vision; Encourage risk taking 6. Plan for and create short-term wins Plan for and create visible performance improvements ; Recognize and reward employees involved in the improvements 7. Consolidate improvements and produce still more change Use increased credibility to amplify change in systems, structures, and policies; Hire, promote, and develop employees who can implement the vision; Reinvigorate process with new projects, themes, and change agents RISK: Not Neutralizing Resistance !!! RISK: Leaving Successes to Chance !!! RISK: Declaring Victory Too Soon !!! RISK: 8. Institutionalize new approaches Articulate and reward the connections between the new behaviors and corporate success; plan leadership succession consistent with the vision Declaring Victory Too Soon !!! Implementing Change Strategies to Consider 1. The path of least resistance 2. 3. 4. 5. - best use of the people willing to change Impact - biggest improvements early in implementation Learning - the most learning happens as the change is implemented Resources - best scheduling and use of available resources Interdependence - will the change work without all its components? Implementing Change – Foolproof the New Process/Procedure Reduce likelihood of mistake/error – Decrease the likelihood that a needed item is left off the surgery cart by prepackaging kits of instruments and other surgical items – Make it impossible to attach the vacuum line to an oxygen outlet by installing different sizes or shapes for vacuum and oxygen connectors – Get rid of old versions of forms! Change the Culture – Holding the Gains • Make reversal as difficult as possible • Establish a standard process • Use measurement and audits • Pay attention to maintenance processes, especially orientation and training Partnering with Patients • When does this begin • How do we individualize our education • Who make it happen? Engaging Partners and Community Stakeholders • Who are our partners in mitigating risk – How do we engage them – How can we partner in this work • Who are your community resources – Do you KNOW what they offer – Do you TRUST what they provide – Do you BELIEVE they can make a difference Kotter’s 8 Reasons Why Attempts at Change Fail 1. 2. 3. 4. 5. 6. 7. 8. Not establishing a great enough sense of urgency. Not creating a powerful enough guiding coalition. Lacking a clear vision. Under-communicating the vision by a factor of ten. Not removing obstacles to the new vision. Not systematically planning for and creating short-term wins. Declaring victory too soon. Not anchoring changes in the corporate culture. Team Planning • Reflect on you Aim and Measures • Use the worksheet provided to plan: – Your tasks – Your first PDSA (who, what, where, when) – Report on aspect of this work to another team