Communication - Cheshire & Merseyside Strategic Clinical Networks
advertisement

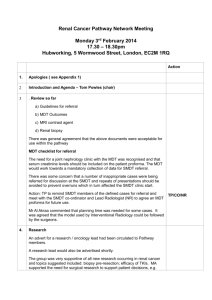
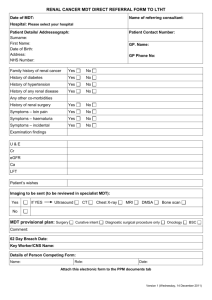
Local MDT Reports on Communication Between Local and Specialist MDTs CNSs & MDT Co-ordinators South Mersey SMDT Graeme Totty, Urology SMDT Co-ordinator Jeni Nixon, Local Urology Co-ordinator, WUTH Karen Beckett, Local Urology Co-ordinator, CoCH Linda Mallanaphy, Local Urology Co-ordinator, NCH Referrals to SMDT • • • • > from local co-ordinator via MDT/verbal > from Uro-Oncology Nurse by phone > Clinic letters from Consultants > for NCH & CoCH, patients are referred by local MDT co-ordinators by e-mail • > proformas not currently used Liaison between SMDT & local MDT co-ordinators • > Wirral MDT co-ordinator works in same office • > Visit CoCH co-ordinator at least once a week & regular e-mails & phone calls in between • > Visit NCH co-ordinator each Wednesday & in contact by phone or e-mail Collection of case notes & slides • Case Notes & slides collected from CoCH MDT co-ordinator each Wednesday • Slides collected from NCH Pathology Lab each Wednesday (case notes needed at local Hospital for video-conferencing to SMDT) Pathology review • All slides from CoCH & NCH (along with WUTH cases) are reviewed prior to SMDT by Consultant Histopathologists • Histology from CoCH & NCH is displayed & discussed only if there is disagreement with the original report Role of Co-ordinator @ SMDT meeting in relation to chair • Changed from start of 2010 • Meeting chaired on rotational basis by Consultant Urologists + Oncologists • Cases discussed in order on agenda Timeline for referrals • > Most CoCH & NCH referrals are made on Wednesday following discussion at local MDT & discussed @ SMDT on the Friday of the same week • > Majority of Wirral cases go straight to SMDT without previous discussion. SMDT Outcomes • > Outcomes are e-mailed to all members each Monday • > The completed SMDT pro-forma is faxed to patients G.P. on Monday after the meeting • > Pro-forma faxed to Consultant @ NCH & CoCH at same time • > Patients are contacted by Specialist Nurse if applicable Other responsibilities • Track patients journey in relation to cancer Waiting Time Targets (now on SCR). • Co-ordinate cases for discussion @ weekly Penile SnMDT • Provide data for Audits/Peer Review etc Challanges • Adapting to Somerset Cancer Registry for use in SMDT • Obtaining feedback on patients discussed @ SMDT & followed up at local hospital. • Dealing with increasing number of patients discussed North Merseyside Urology Specialist MDT Group Will Maitland Interaction and co-ordination with Local MDT groups North Merseyside Urology SMDT Group Royal Liverpool and Broadgreen NHS Trust Southport and Ormskirk NHS Trust University Hospital Aintree NHS Trust Whiston Hospital NHS Trust Nobles Hospital NHS Trust Referrals also accepted from South Liverpool NHS Trusts SMDT Referrals Referral deadline = midday Wednesday. Sent via facsimile or secure email links. Referrals consist of completed patient proforma accompanied by all relevant radiology and histopathology reports. Majority of patients discussed at SMDT have been discussed at the Local MDT groups the previous week. SMDT outcomes are sent back to referring Trust by midday the following Monday and official letters are dictated by SMDT Chair. ISSUE – Illegible hand-writing makes data entry difficult, leading to data errors on SMDT discussion lists. SMDT Histopathology Review Reviews are undertaken by either Dr Paul Mansour, Dr Vijay Aachi or Prof. Chris Foster. Pathology review takes place for specified patients at the SMDT, not every patient at present. Slides are either sent by Local Trust teams ahead of SMDT referral or facsimile requested by the SMDT co-ordinator after initial discussion. Target turn-around for pathology review is 14 days after initial discussion. Pathology review reports are sent back to original pathologist at the referring Trust. SMDT Radiology Review Reviews undertaken by either Dr Jane Belfield, Dr Peter Rowlands, Dr Gabby Lamb or Dr Kirsty Slaven. Radiology reports sent by facsimile with the individual SMDT referral proformas and passed to the core radiologists. SMDT co-ordinator completes individual ‘Image Request’ proformas for each individual patient. ‘Image Request’ proformas are emailed to the Trust PACS Team who arrange for the notes to be transferred electronically from the referring Trust. ISSUE – Original radiology reports cannot be sent electronically with the images? SMDT Patient Casenotes Notes sent to and from the centre Trust from Aintree and Whiston hospitals only. Notes are addressed to the recipient and sent by registered taxi courier. ISSUE – Reconstituted notes from Whiston Hosp makes locating and presenting patient info during SMDT difficult. Conclusion and Future Challenges An efficient and robust service however there are areas which need to be addressed…. Hand-written referral proformas. Sending of electronic radiology reports with requested images. Reconstituted Whiston notes. Pathology review of all patients discussed at Urology SMDT. Communication/ Issues from local MDT’s Michelle Thomas UHA North SMDT Duplication of information sent to SMDT. Patients are contacted before outcomes are given. Organisation of patients to be discussed. Access to MDT co-ordinator. Renal service appears to be fragmented. Video link. Outcomes of patient attending joint clinic. Reliant on CNS giving outcome. South SMDT Video link not reliable. Patients wait one week for oncology appt. Patients require separate appointment to discuss surgery. Patients prefer to be seen at local hospital. Completely reliant on CNS giving outcome over telephone. No Issues with outcomes/proformas etc. Key worker Transfer Beverley Rogers/Gill Riley Urology MacMillan Nurse Specialists Mersey South Urology Cancer Centre POLITICAL AGENDA • Manual for Cancer Service Standards 2004 • NICE Improving Supportive and Palliative Care for Adults with Cancer 2004 • Cancer Reform Strategy 2007 • MCCN Key Worker Guideline WHAT IS A KEY WORKER? The key worker is defined in the NICE guidance (2004) as: “A person who with the patient’s consent and agreement takes a key role in coordinating the patient’s care and promoting continuity, ensuring the patient knows who to access for information and advice.” WHY DO PATIENTS NEED A KEY WORKER? There is a need to ensure integration and co-ordination of care, throughout the patients cancer journey The aim should be to provide continuity of care throughout the patient pathway. DESIGNATING THE KEY WORKER Each patient should have a named key worker who will be identified at the MDT where the initial cancer diagnosis is made and treatment planning decisions discussed. The key worker will ideally be a Clinical Nurse Specialist. • • • • • • The named key workers should be reviewed at key points in the patient’s cancer journey: Around the time of diagnosis Commencement of treatment Completion of the primary treatment plan Disease recurrence The point of recognition of incurability The point at which dying is diagnosed RECORD KEEPING The name, designation and contact details of the key worker should be recorded within the patient notes. Multi-disciplinary teams must agree a method of documentation, for example, the MDT proforma, which is signed and dated. The patient should be provided with written information detailing the name of the key worker, designation and contact details. The key worker’s details should be included in all correspondence. What happens South of the Mersey…. • Uro oncology nurses both attend SMDT • Pick up patients who will need appointments/investigations at cancer centre • Ensure appropriate appointments made • Ensure available at clinic appointment (transfer of key worker) Tools Used • “business card” and information leaflet with specialist nurse contact names and direct dial number • Patient access to permanent record of consultation • Letter link • Diaries!! Liaison with Key Worker at Referring Hospital • Not on a routine basis • No formal handover • Contact on an individual basis following patient assessment of understanding Does it work ? • Three patient experience surveys undertaken; • > penile cancer • > cystectomy • > nephrectomy PENILE CANCER • 63% RETURN • 95% knew who specialist nurse/key worker was • 84% Knew how to contact specialist nurse/ key worker Cystectomy • 61% return rate • 100% patients knew who their specialist nurse/key worker was • 100% of patients knew how to contact their specialist nurse/key worker Nephrectomy • 85% return rate • 100% of patients knew who their specialist nurse/key worker was • 100% of patients knew how to contact their specialist nurse/key worker Issues • Lack of uro oncology cns at CCO • Major impact on workload WUTH (from a local perspective) • Can not transfer key worker CONCLUSIONS • Appears to work well • Patient satisfaction • No need for another form of paperwork • ??? The Role Of Radiotherapy Liaison & Support Practitioner. Martin Woods Radiotherapy Liaison & Support Practitioner Clatterbridge Centre for Oncology 0151-334-1155 Ext 4727 Bleep 4195 martin.woods@ccotrust.nhs.uk Key Skills Communication Patient centred approach Liaison & Teamwork Signposting Documentation & Accuracy Enthusiasm & Motivation I provide holistic assessment & care to patients’ receiving radiotherapy& chemo-radiotherapy who are not linked with a site specific CNS. This includes:- • Bladder Cancer • Prostate Cancer • Upper G.I. Cancers (oesophagus, stomach, • • • • gall bladder, liver). Brain Tumours Lymphomas Melanomas/Sarcomas Testicular Cancers Communication NICE Guidance states: Interpersonal communication is the process through which patients & carers can explore issues & arrive at decisions in discussions with health & social care professionals. It is most effective when there is mutual understanding, respect & awareness of individuals’ roles & functions. • Important to establish an excellent rapport with patients’ & carers – vital to enable me to assess their immediate & future needs. Communication •Establishing that initial rapport can pay dividends for the future relationship with the patient – common ground •I have a patient centred approach & provide an empathetic & sympathetic ear to patients’ & their carers’. •Discussions with patients and carers at key stages aids holistic assessment and identifies existing and potential needs. •I monitor patients’ progress throughout the course of treatment & make further referrals if necessary. Liaison & Teamwork I have an excellent working relationship Radiotherapy colleagues, with members of the CReST team & Doctors. Developed good working relationship with Specialist Nurses. Signposting The Radiotherapy Support Practitioner is a link to the other professionals & services the patient/carer may need • CReST Team • Cancer Nurse Specialist (CNS) • District nurse • Macmillan Nurse • Occupational therapist • Social workers • Psychologist • Chaplain Signposting I am aware of my limitations & can recognise when the solution to the patient’s needs are outside of my competencies – referring to the appropriate professional. What makes this post special? The difference between involvement and commitment is like egg and bacon. The chicken is involved; the pig is committed! I am committed to giving the best care & support to patients’ & their carers Local MDT’s – common problems ◦ Reliance on CNSs to give feedback on outcomes ◦ Difficulties with video link SMDT co-ordinators – ◦ Issues variable Lack of a forum between the CNSs and the MDT co-ordinators within the Network to discuss issues and share good practice Need to identify how there can be a seamless transition in the role of key worker from centre to centre ◦ CNSs from local centres attend joint clinics – i.e. the key worker stays with the patient where possible ◦ Improved transfer of information between key workers if different at each centre – how?? ◦ Leaflets to be given to patients at diagnosis / transfer of care explaining how the key worker changes