Brown recluse
advertisement

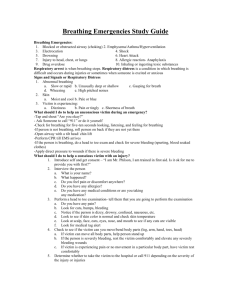
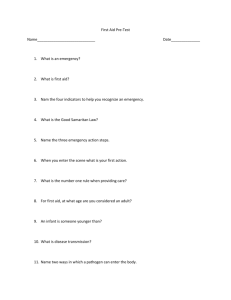
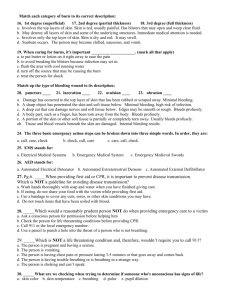
Personalizing your approach to medical emergencies and more minor medical problems Kathie King MD FHYC Fleet Surgeon October 15, 2010 Learn new skills Validate what you already know (this is a sophisticated crowd) (remind you of easily-forgotten facts) (Caveat: this is not a first aid course) What is First Aid? Medical Emergencies First response to situation that requires advanced care Life or Limb-threatening Bleeding Airway Cardiac Arrest Allergic reactions Broken bones Non-emergency First Aid Minor medical needs May need advanced care Minor wounds Minor allergies Common medical problems treated with over-the-counter medications Common injuries “The first thing about First Aid is to be careful, so First Aid can be avoided!” Safety Situational awareness (hazards in environment) Temperature (heat, cold), sun exposure (sunscreen) PFDs, lifelines, bow and stern pulpits, grabrails Appropriate clothing including footwear Boat itself Falling on the boat Caught between boat and another object Falling overboard Where are you cruising? What are you likely to encounter? What will you need? How easily can you obtain supplies? How can you obtain help in an emergency? … from land to a marine environment Your knowledge about your medical conditions Your knowledge about general medical conditions and First Aid Resources: Books Courses/training Subscription medical services Evacuation insurance (Divers Alert Network) Your medication/treatment regimen Supplies for exacerbations/complications Copies of your baseline EKG and other medical records Supplies for expected problems (sunburn, minor cuts, environmental hazards) Supplies for unexpected problems (accidents, illnesses) Are your immunizations up to date, appropriate for your travel? (ex. travel clinic @ Duke for people planning to travel) Other cruisers- VHF or SSB, not your cell phone Coast Guard- channel 16 Leave “how to get help” laminated instructions at the helm, should your guests need to get help for YOU! Common Medical Problems Heart Attack Fractures Stroke Wounds Seizure Bleeding Allergic Reaction Head/neck injury Diabetes Sprain/strain Nausea/Vomiting Burns Heat-related illness Snakebites Cold-related illness Bites and stings Poison oak/ivy/sumac Symptoms: chest pain, shortness of breath, nausea, pain radiating to arms or jaw, sense of impending doom, ashen skin, weak or irregular pulse, sweating, fainting or dizziness, collapse. Symptoms are different in women and in people with diabetes Treatment must be given within 6 hours of onset of symptoms Encourage victim to rest, half-sitting, knees bent, position of comfort Have aspirin available (ask: allergic to ASA or is it contraindicated?) 2 baby-ASA or 1 adult-ASA Does the victim have/use nitroglycerin? If the victim becomes unconscious, get advanced help immediately Be prepared to give rescue breaths and chest compressions Symptoms: Problems with speech or swallowing, weakness or loss of movement in limbs, headache, confusion or loss of consciousness Cincinnati stroke scale Facial droop Arm drift Abnormal speech “Brain attack” Maintain open airway, no food or drink, arrange transport ASAP Treatment must be given within 3 hours CT scan in ER (embolic vs. hemorrhagic) Symptoms: loss of consciousness, rigidity, convulsive movements During the seizure: protect the head, ease the fall, do not restrain After: open the airway, place in “recovery “ position (log-roll victim onto side with upper leg forward, their hand under face to prop open their airway) Post-seizure confusion Medical help if new seizure, unconscious >10 minutes, or recurrent seizures; may need airway management new-onset vs. established pattern; causes: tumor; low blood sugar Causes: bee-stings, drugs, shellfish, peanuts, milk, egg (contact by ingestion, injection, skin, or inhalation) Symptoms: red, blotchy skin; puffy eyes; swelling of throat and tongue, trouble breathing, signs of shock If mild: consider antihistamines, topical anti-itch or steroids If severe: call 911, EMS, or Coast Guard Epi-Pen (epinephrine) a mild reaction can become severe, within minutes! Epi-Pen information: http://www.epipen.com/~epipen/page/english-cable--how-touse-epipenreg-auto-injector--epinephrine--anaphylaxis Symptoms: polyuria, polydipsia, polyphagia (increased urine, thirst, eating) Problems: High blood sugar: dehydration, electrolyte imbalance warm, dry skin; rapid breathing; drowsy; fruity smell Low blood sugar: confusion, seizures sweaty, cool skin; jittery; rapid loss of consciousness if awake: 4 oz sugary drink or tablets if not awake: get emergency help If the person cannot manage his diabetes, seek medical attention. Mal de mer Causes: Sensory: mal de mer, Meniere’s GI tract: gastritis, obstruction, poisoning Brain: tumor, concussion, migraine Metabolic: kidney, diabetes, other Misc: pregnancy, drugs, infections Problems: dehydration, electrolyte imbalance Care: “supportive” Anti-emetics (patch, pill, suppository), ginger Wrist bands “BRAT “ diet (bananas, rice, applesauce, toast) Cooling mechanism: vasodilation; sweating and evaporation Symptoms of HEAT EXHAUSTION: sweating, rapid pulse and breathing , muscle cramps, headache, nausea, dizziness, weakness, loss of appetite. Cause: excessive sweating, loss of fluids and electrolytes Signs of HEATSTROKE: skin red-hot and dry, shallow breathing with full and bounding pulse, confusion to sudden loss of consciousness, seizures, body temperature >104, vomiting, unable to drink, seizures; may follow heat exhaustion when sweating stops . Cause: failure of temperature regulation, loss of sweating Care: Heat exhaustion: Lie down with legs raised. Sponge with cool water until temperature and behavior return to normal; encourage to drink. Possibly needs medical care, prepare for worsening. Heatstroke: Cool as rapidly as possible with water, not alcohol. Remove outer clothing, wrap in wet sheets until temperature is <100.4 under tongue or <99.5 under armpit. Do not give water or food if victim cannot swallow or respond or has had a seizure. Seek medical help immediately. Be prepared to give rescue breaths and chest compressions. Heat conservation: vasoconstriction, less sweating, hair stands on end, shivering (increases metabolic needs 300%) Hypothermia: when body temp is <95 (can be fatal if <86) Causes: prolonged exposure, “wind-chill” factor, cold water, chronic illness, fatigue, inactivity, alcohol or drugs., extremes of age Symptoms: shivering, cold pale dry skin, apathy or disorientation, lethargy or loss of consciousness, slow shallow breaths, slow pulse. Care: Replace wet clothing; bathe in 100-104 degree bath if victim is fit and can navigate tub, otherwise use warm blankets or forced warm air. Do not use direct sources of heat. Handle gently because in severe cases, rushed movement may cause heart to stop. Seek medical attention for infants, the elderly, or if you have any doubts about victim’s condition. *They’re not dead until they’re warm and dead* Symptoms: pain, limited movement, shortening or deformity of limb, swelling, bruising, coarse grating sound, possibly a wound or shock Care: prevent movement (esp if fracture is unstable) check circulation beyond injury, esp after dressing applied do not move victim until injury is splinted (unless in danger) support injured part with hands until immobilized materials to splint (apart or secured to unaffected body part) don’t straighten any bent body parts if open fracture, clean dressing with gentle pressure if bleeding apply ice to injured area for 20 minutes Cause: partially or completely torn or overstretched ligaments (sprain), muscles or tendons (strain); may be difficult to distinguish from fracture (may need x-ray) Symptoms: pain that worsens with movement or pressure, swelling, bruising Care: RICE x 24 hours rest: try not to move (may need splint or sling) ice: first 24 hours (20 min, 4-8x per day), then ice or heat compression: Ace bandage to reduce swelling and pain elevate: to decrease swelling Plus may need pain meds, an exercise program, or to see MD or PT Cause: direct or indirect blows to head All head injuries are potentially serious Must recognize life-threatening brain compression deteriorating consciousness, difficulty breathing, unequal pupils clear fluid or watery blood from the nose or ear control external bleeding and have victim lie down other signs: dizzy, nausea, memory problems, headache Assume that anyone with a head injury also has a neck injury steady and support head, tell victim not to move support victim’s neck (don’t alter neck position if distorted) look for pain, tenderness, loss of movement or sensation Obtain medical attention ASAP, esp if victim is unconscious or has had brief period of unconsciousness with return to consciousness Causes: various; arterial, venous; external, internal (blood that you can and can’t see); type of wound (abrasion, puncture, etc); wound location What to do: Assess the scene (safety), victim (stability, type of wounds, injuries) Comfort, reassure; use protective equipment (gloves, eye protection) Select dressing material (clean, large enough to cover wound) Control blood loss by direct pressure and elevation Reinforce (add more) dressing as needed (do not remove first piece) Assess for shock (rapid pulse, sweating, altered consciousness) Pressure points, tourniquet only if in extremis Obtain help if bleeding does not stop in 15 minutes, bleeding is heavy, or victim has trouble breathing. Causes: various cuts, scrapes, punctures Care: Make sure scene is safe Use protective equipment (gloves, eyes) Wash with soap and water Stop bleeding with pressure (use fingers or palm of hand) Apply dressing to cover wound (consider antibiotic cream) Ask if victim has recent tetanus shot Call for help if excessive bleeding, shock (weak, dizzy, agitated or confused), or large or complex wound Causes: contact with heat, electricity, chemicals Symptoms: pain, difficulty breathing, shock (rapid pulse, shallow breathing, clammy skin, weak, dizzy, nausea, thirst, restless, possibly unconsciousness); may see red, blistered or broken skin Concerns: airway (esp if inhalation injury), dehydration, infection Care: stop the burning process apply cool liquid for 10 minutes (do not overcool) remove rings or constrictive items remove burned clothing if not stuck to skin cover burn with sterile or clean dressing (no lotions, oils) do not break blisters Transport to medical care ASAP if airway injury or large burn! Be familiar with native plants and animal species you’ll encounter along your itinerary, including how to identify them (and possibly capture the culprit for an expert to ID so you can get specific treatment for bites etc). Be able to describe the snake (hard to ID; bring snake in if possible) cottonmouth- “raccoon mask” (white stripe on face) copperhead- splotchy apricot, burgundy, gray or tan rattlesnake- variable colors, patterns (diamond, stripes) & sizes coral snake- “red touches yellow, kill a fellow” stripes Signs of poisonous snakebite: progressive pain and swelling at bite nausea, vomiting, sweating, weakness Seek medical treatment ASAP unless snake positively ID'd as nonvenomous Care: (no cold, ice, suction, or cutting the site of bite) Keep victim calm, do not move body part that was bitten Gently wash bite with soap and water (leave uncovered) If coral snake: apply bandage with mild pressure over wound (no antivenom; this victim is treated with elective intubation and ventilation) Seek medical treatment ASAP unless snake positively ID’d as nonvenomous (need to get antivenom within 4-5 hours of bite) Bees, wasps, hornets, yellow-jackets, fire-ants, mosquitoes, ticks Types of reactions: Immediate: Itching, stinging, swelling Delayed: Fever, hives, joint pain, swollen glands Infections (Lyme disease, Rocky Mtn Spotted Fever) Anaphylaxis: Nausea, facial swelling, difficulty breathing, abdominal pain, low blood pressure Care: Mild (swelling, redness, and pain): scrape off stinger (do not pinch- or even touch), raise affected area if possible, apply ice pack consider hydrocortisone 0.5%, baking soda paste, or antihistamines Severe reaction (anaphylaxis): Epi-Pen, medical attention Stings to mouth and throat: suck on ice or cold water, consider transport to medical facility for airway problems 20,000 spiders in North America 60 bite 4 venomous Black widow spider Brown recluse spider “Hobo” (aggressive) house spider Yellow sac spider Non-venomous spiders can bite (and be painful), too! The 2 worst actors: Black widow: red hourglass or spots, occ yellow marks; prefers crevices; early symptoms: pain at bite, abdominal pain, muscle cramps, weakness, tremor (neurotoxic); mimics other illnesses; antivenom available. Brown recluse: violin pattern on upper body; prefers barns, basements, old tires; early symptoms: itching, nausea, vomiting; later skin necrosis (tissue death), abnormal clotting and bleeding, kidney damage; no antivenom. *hard to ID; bring spider if possible; get treated early “Hobo” spider: brown, mistaken for brown recluse; prefers; soil and debris, under rocks, in crawlspaces; pain, scabs, blisters, scars (often confused with brown recluse , less severe course). Yellow sac spider: pale yellow or white; prefers ceilings and foliage, often co-exists with people; symptoms mild redness, swelling, itching, heals in 2 weeks (mistaken for brown recluse). *hard to ID; bring spider if possible Non-venomous species: Raise body part if possible, apply ice packs or cool compresses Watch for signs of allergic reaction (wheezing) or anaphylaxis (collapse); seek medical attention as needed *hard to ID; bring spider if possible 2,000 species Cousin of the spider, usually only attacks if feels threatened More problem in developing countries (and Arizona) Check bedclothes, etc! Care: Wash with soap and water Cool compresses- on 10 minutes, off 10 minutes If possible, elevate bite area above heart Seek medical attention if blurred vision, wandering eye movements, muscle twitching, or numbness/tingling of extremities Jellyfish, corals, anemones, Portuguese men-of-war, urchins, barracudas, eels, catfish Symptoms: Pain, bleeding, swelling, numbness, burning, redness More serious: cramps, diarrhea, difficulty breathing, fever, nausea/vomiting, paralysis, sweating, weak, faint dizzy; occasionally, anaphylaxis. May need help- removing stinger, or advanced medical care. Care: Wipe off stingers with towel; wear gloves. Wash with salt water, then soak in hot water 30-90 minutes if instructed by trained personnel. Possibly vinegar or meat tenderizer may neutralize toxins? Possibly compress limb above sting, immobilize limb? SEEK HELP- removing stinger, advanced medical care. Most common allergic contact dermatitis in the US 60-80% of people react to this allergen ( is both irritant and allergen) Urushiol (an oil) found in poison oak/ivy/sumac in roots/stem/fruit Exposure by direct contact, smoke, your clothes (for years!) IvyBlock can be applied before plant contact TechNu removes urushiol, then alcohol dissolves unabsorbed poison Dry clean your clothes or wash separately and clean machine or leave clothes in sun (UV breaks down urushiol) Symptoms: Itching, then redness, then rash (4 hours to 10 days later; can last 3 weeks), then fluid-filled blisters (non-contagious) 15% severely allergic, some with respiratory problems (esp if plants burned and inhaled urushiol) Care: cleanse yourself with alcohol, magnesium sulfate, or TechNu avoid soaps (may move the urushiol to other areas!) clean your clothes and equipment with alcohol cool compresses or over-the-counter soothing gels topical steroid or non-steroidal anti-inflammatory creams oral anti-histamines or steroids Understand your plans and potential circumstances Know your skills and bring supplies for what you can treat Ask your physician about necessary medications and supplies Consider First Aid/CPR courses (Red Cross, Heart Association) Consider First Aid books (American College of Emergency Physicians) Consider evacuation insurance (Divers’ Alert Network) Consider subscription medical advice service (see Internet Resources, next slide) HAVE FUN! Medical kits, subscription medical services http://www.riparia.org/cruising_medical_kit.html http://www.marmed.com/marmed.htm http://www.seasidemarineintldrug.com/home.html https://www.tripprep.com/scripts/main/default.asp http://www.worldclinic.com/ Evacuation insurance http://www.diversalertnetwork.org/insurance/ http://www.diversalertnetwork.org/