physio lecture 2-4(Cellular transport mechanisms)
advertisement

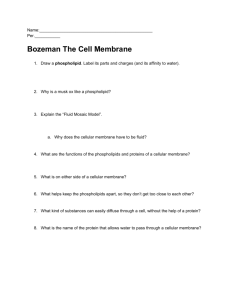
Objectives •Understand how proteins and lipids are assembled to form a selectively permeable barrier known as the plasma membrane. •Explain how the plasma membrane maintains an internal environment that differs significantly from the extracellular fluid. •Explain the importance and characteristics of carrier-mediated transport systems. •Understand how voltage-gated channels and ligand-gated channels are opened. •Explain, using specific examples, the difference between primary and secondary active transport. The Structure of the Plasma Membrane Lipid bilayer – two sheets of lipids (phospholipids)-Polar (water-soluble) heads face out and the non-polar fatty acids hang inside. Polar head non-polar tail • Embedded with proteins and strengthened with cholesterol molecules. -- Integral proteins (or intrinsic proteins) are embedded in the lipid bilayer, Include channels, pumps, carriers and receptors. -- Peripheral proteins (or extrinsic proteins) do not penetrate the lipid bilayer. They are in contact with the outer side of only one of the lipid layers either the layer facing the cytoplasm or the layer facing the extracellular fluid Integral-Membrane Proteins Can Serve as Receptors Integral-Membrane Proteins Can Serve as Adhesion Molecules, ex- integrins, Cadherins. Can Form a Submembranous Cytoskeleton, Ex- spectrin,ankyrin Hereditary Spherocytosis •Hereditary spherocytosis (HS) is a genetic disease that affects proteins in the erythrocyte membrane, and the result is a defective cytoskeleton. •The most common defect is deficiency of spectrin, and the result is that regions of the membrane break off because they are no longer anchored to the cytoskeleton. •cell eventually becomes small and spherical. •Hemolysis (cell bursting) is present because the spherocytes are fragile to osmotic stress. Membrane Transport Cell membrane is permeable to: Non-polar molecules (02& C02). Lipid soluble molecules (steroids). H20 (small size, lack charge). Cell membrane impermeable to: Large polar molecules (glucose). Charged inorganic ions (Na+ , K+ etc.,). Types of Membrane Transport • The movement of large molecules is carried out by endocytosis and exocytosis, the transfer of substances into or out of the cell, respectively, by vesicle formation and vesicle fusion with the plasma membrane. • Cells also have mechanisms for the rapid movement of ions and solute molecules across the plasma membrane. • These mechanisms are of two general types: -- passive movement, which requires no direct expenditure of metabolic energy, and substances move across the membrane down their electrochemical gradient -- and active movement, which uses metabolic energy to drive solute transport against this gradient. Passive transport Processes Includes: A) Diffusion & B) Osmosis Bulk Transport (Endocytosis and Excytosis) Movement of many large molecules, that cannot be transported by carriers. Exocytosis: A process in which some large particles move from inside to outside of the cell by a specialized function of the cell membrane Endocytosis: Exocytosis in reverse. Specific molecules can be taken into the cell because of the interaction of the molecule and protein receptor. 11 Exocytosis Vesicle containing the secretory protein fuses with plasma membrane, to remove contents from cell. 12 Endocytosis Material enters the cell through the plasma membrane within vesicles. 13 Types of Endocytosis Phagocytosis - (“cellular eating”) cell engulfs a particle and packages it with a food vacuole. Pinocytosis – (“cellular drinking”) cell gulps droplets of fluid by forming tiny vesicles. (unspecific) Receptor-Mediated – binding of external molecules to specific receptor proteins in the plasma membrane. (specific) 14 Example of Receptor-Mediated Endocytosis in human cells 15 Diffusion • By which molecules move from areas of high concentration to areas of low concentration and cations move to anions. • Its of 2 types. 1. Simple 2. Facilitated Diffusion • Simple Diffusion: means molecules move through a membrane without binding with carrier proteins. • Facilitated: requires a carrier protein which aids in passage of molecules through the membrane by binding chemically and shuttling them through the membrane. 1. Simple Diffusion Molecules/ions are in constant state of random motion due to their thermal energy. Simple diffusion occurs whenever there is a concentration difference across the membrane the membrane is permeable to the diffusing substance. 17 Membrane Transport particles C1 ● ● C1 ● ● ● ● ● ● ● C2 ● ● ● C2 ● ● ● ● time ●● Another presentation of Fick’s law : J = D A ΔC / ΔX Where , D=Diffusion coefficient factors that influence net flux are: (Fick`s law of diffusion) 1. Electrical gradient. If the molecule is charged then its net flux across a membrane will be increased if the charge on the other side is opposite. 2. Temperature. Higher temperature ⇒ greater net flux 3. Surface area of membrane. Greater the surface area greater the net flux. 4. Molecule mass. Higher mass molecules move slower so the net flux would be less 5. Membrane permeability. The greater the membrane permeability for the molecule the greater the net flux Diffusion Rate Jx ↑Px Flux ↓Px [X] Concentration Simple Diffusion • Most molecules partition poorly – i.e. soluble in water but not lipid – therefore cannot cross lipid bilayer • Need – pores, channels and transporters The major property of biological membranes which makes them impermeable to most ions and polar molecules is A The presence of cholesterol B The absence of all proteins from the membrane C The structure of the lipid bilayer D The absence of charged groups on the membrane surface E The hydrophilic core of the membrane Pores, Channels and Transporters • Pore – transmembrane protein that is open, ex-aquaporins • Channel – transmembrane protein with a pore that can open and close(gated) • Transporter – transmembrane protein that undergoes a conformational change and facilitates the transport of a ‘packet’ of substrate across the membrane Ion Channels. •The cell membrane has ion channels that increase the permeability of the membrane for that ion species and allows the movement of those ions down their electrochemical gradient, channels can be opened or closed by gates •These channels can show a high degree of specificity for a particular ion species, e.g. the epithelial sodium channel is 30 times more permeable to Na+ than K+. Regulation of ion channels Ion channels gates may be open or closed and the time and frequency of opening may be regulated. There are three major factors that are involved in the regulation of the frequency and duration of channel opening. 1.Ligand-gated channels 2.Voltage-gated channels 3.Mechanosensitive channels Ligand gated Ion Channel • The channel is a channel/receptor complex • Upon ligand binding there is a conformational change that opens the channel • Selectivity is conferred by charged amino acids and size (selects for cations or anions and then selects for size e.g. K+ ion much larger than Na+ ion – hydrated form) Ligand-Operated ACh Channels Ion channel runs through receptor. • Receptor has 5 polypeptide subunits that enclose ion channel. • 2 subunits contain ACh binding sites. 26 Voltage Gated Ion Channel • change in membrane potential(Vm) moves charged molecules within the channel changing channel conformation either opening or closing the channel. • Charged amino acids inside the channel - pore detect the electric field across the membrane – and conformational change can occur in response to a change in electric field Organ of Corti When sound waves move the basilar membrane it moves the hair cells that are connected to it, but the tips of the hair cells are connected to the tectorial membrane the hair cell get bent . There are little mechanical gates on each hair cell that open when they are bent. K+ goes into the cell and Depolarizes the hair cell. (concentration of 29 K+ in the endolymph is very high) Facilitated Diffusion via carrier • Ex- glucose, amino acid transport. – Down concentration Gradient – Chemical Specificity: Carrier interact with specific molecule only, cysteinurea. – Competitive inhibition: Molecules with similar chemical structures compete for carrier site. – Saturation: Vmax (transport maximum): Carrier sites have become saturated. glucose transporter 4 (GLUT4) activated by insulin Graph showing the relationship between net flux and concentration gradient of a substance moved across the membrane via facilitated diffusion. If the concentration gradient (and hence concentration) increases enough the transporters will become saturated and the net flux cannot be increased, this net flux value is called the transport maximum. Active transport When the cell membrane moves molecules or ions uphill against a concentration gradient (or uphill against an electrical gradient), the process is called active transport Primary active transport Secondary active transport: Active transport 1 Primary active transport: the energy used to cause the transport is derived directly from the breakdown of ATP or some other high-energy phosphate compound 2 Secondary active transport: The energy is derived secondarily from energy That has been stored in the form of ionic concentration differences between the two sides of the membrane created by primarily active transport Intracellular vs extracellular ion concentrations Ion Intracellular Extracellular Na+ K+ Mg2+ Ca2+ H+ 5-15 mM 140 mM 0.5 mM 10-7 mM 10-7.2 M (pH 7.2) 145 mM 5 mM 1-2 mM 1-2 mM 10-7.4 M (pH 7.4) Cl- 5-15 mM 110 mM 3.1 Primary Active Transport Hydrolysis of ATP directly required for the function of the carriers. Molecule or ion binds to “recognition site” on one side of carrier protein. 3.1 Primary Active Transport Binding stimulates phosphorylation (breakdown of ATP) of carrier protein. Carrier protein undergoes conformational change. Hinge-like motion releases transported molecules to opposite side of membrane. Mechanism of Acid Secretion •The key player in acid secretion is a H+/K+ ATPase or "proton pump" located in the parietal cell membrane. •Hydrogen ion is pumped out of the cell, into the lumen, in exchange for potassium through the action of the proton pump. Na+/K+ Pump A Model of the Pumping Cycle of the Na+/K+ ATPase 39 Importance of the + + Na -K Pump Control cell volume Develop and Maintain Na+ and K+ concentration gradients across the membrane Electrogenic action influences membrane potential Provides energy for secondary active transport 2 Secondary Active Transport Energy needed for “uphill” movement obtained from “downhill” transport of Na+. Hydrolysis of ATP by Na+/K+ pump required indirectly to maintain [Na+] gradient. 41 Secondary active transport co-transport (symport) out in Na+ glucose Co-transporters will move one moiety, e.g. glucose, in the same direction as the Na+. counter-transport (antiport) out in Na+ ca2+ Counter-transporters will move one moiety, e.g.ca2+, in the opposite direction to the Na+42. Insulin Secretion and Membrane Transport Processes (b) 1 Beta cell secreting insulin. Closure of the KATP channel depolarizes the cell, triggering exocytosis of insulin. 2 High glucose levels in blood 3 4 KATP channels Metabolism ATP increases. increases. close. 5 Cell depolarizes and calcium channels open. 6 Ca2+ entry acts as an intracellular signal. Ca2+ Glucose GLUT transporter Glycolysis and citric acid cycle ATP Ca2+ 7 Ca2+ signal triggers exocytosis, and insulin is secreted. Epithelial Transport A 7-year-old boy is brought to the pediatrician because of a chronic cough, fatty diarrhea, and failure to thrive. Pseudomonas aeruginosa is cultured from his respiratory tract. The physician informs the patient’s parents that their son has a disease that is caused by a mutation in a specific ion transporter. This patient has a mutation in the ion transporter of which of the following electrolytes? (A) Bicarbonate (B) Calcium (C) Chloride (D) Potassium (E) Sodium factors that influence net flux are: (Fick`s law of diffusion) 1. Electrical gradient. If the molecule is charged then its net flux across a membrane will be increased if the charge on the other side is opposite. 2. Temperature. Higher temperature ⇒ greater net flux 3. Surface area of membrane. Greater the surface area greater the net flux. 4. Molecule mass. Higher mass molecules move slower so the net flux would be less 5. Membrane permeability. The greater the membrane permeability for the molecule the greater the net flux The Movement of Water Across the Plasma Membrane The Movement of Water Across the Plasma Membrane •Water can move in and out of cells. •But the partition coefficient of water into lipids is low meaning the permeability of the membrane lipid bilayer for water is low. •Specific membrane proteins that function as water channels explain the rapid movement of water across the plasma membrane •These water channels are small integral membrane proteins known as aquaporins Water Movement NaCl 0 mOsm NaCl 100 mOsm [water] HIGH [water] LOW Aquaporin If membrane impermeable to NaCl CLINICAL CORRELATION•In the kidney, aquaporin-2 (AQP2) is abundant in the collecting duct and is the target of the hormone vasopressin, also known as antidiuretic hormone. This hormone increases water transport in the collecting duct by stimulating the insertion of AQP2 proteins into the apical plasma membrane. Several studies have shown that AQP2 has a critical role in inherited and acquired disorders of water reabsorption by the kidney. • For example, diabetes insipidus is a condition in which the kidney loses its ability to reabsorb water properly, resulting in excessive loss of water and excretion of a large volume of very dilute urine (polyuria). Although inherited forms of diabetes insipidus are relatively rare, it can develop in patients receiving chronic lithium therapy for psychiatric disorders, giving rise to the term lithium-induced polyuria. • Both of these conditions are associated with a decrease in the number of AQP2 proteins in the collecting ducts of the kidney. Osmosis - Osmosis is the flow of water across a semipermeable membrane from a solution with low solute concentration to a solution with high solute concentration. The Movement of Water Across the Plasma Membrane Is Driven by Differences in Osmotic Pressure •Osmotic pressure of a solution is defined as the pressure necessary to stop the net movement of water across a selectively permeable membrane •When a membrane separates two solutions of different osmotic pressure, water will move from – the solution with low osmotic pressure (high water and low solute concentrations) to the solution of high osmotic pressure (low water and high solute concentrations). Osmolarity refers to osmotic pressure generated by the dissolved solute molecules in 1L of solvent. It depends strictly on the number of particles in solution (not the number of molecules, since some molecules (e.g. NaCl) dissociate into ions when in solution). Osmolarity is therefore, the number of particles per liter of solution and is expressed in osmol/L or OsM or in the case of dilute solutions as milliosmol/L. Ex- A solution of 1 M CaC12 has a higher osmotic pressure than a solution of 1 M KCl because the concentration of particles is higher. The higher the osmotic pressure of a solution, the greater the water flow into it. Osmolarity The osmotic pressure of a solution can be calculated by - Van't Hoffs law, which states that osmotic pressure depends on the concentration of osmotically active particles. The concentration of particles is converted to pressure according to the following equation: where: osmotic pressure (mm Hg or atm) g = number of particles in solution(osm/mol) 7T = R = gas constant (0.082 L-atm/mol-K) σ = Reflection coefficient (varies from 0 to 1) T = absolute temperature (K) C = concentration (mol/L) The Concept of Tonicity •Tonicity describes a solution, and how that solution affects cell volume. • The tonicity of a solution depends not just on the osmolarity of the solution but also on whether the solutes (particles) in the solution are penetrating or not. • Two solutions having the same effective osmotic pressure are isotonic because no water flows across a semipermeable membrane separating them. • If two solutions separated by a semipermeable membrane have different effective osmotic pressures, the solution with the higher effective osmotic pressure is hypertonic and the solution with the lower effective osmotic pressure is hypotonic. • Water flows from the hypotonic to the hypertonic solution. RBC hypotonic solution Rules for predicting tonicity If the cell has a higher concentration of non-penetrating solutes than the solution, there will be net movement of water into the cell. The cell swells, and by definition that solution is hypotonic. SWELL RBC isotonic solution NO VOLUME CHANGE RBC hypertonic solution SHRINK Tonicity Tonicity describes the volume change of a cell placed in a solution SHIFTS OF WATER BETWEEN BODY FLUID COMPARTMENTS - Types Examples Iso-osmotic volume contraction Diarrhea,Burns Hyperosmotic volume contraction Severe dehydration (sweating, fever, diabetes insipidus - ↓ ADH) Hypo-osmotic volume contraction Adrenal insufficiency (↓ aldosterone) Iso-osmotic volume expansion Infusion of isotonic saline Hyperosmotic volume expansion High NaCl intake Hypo-osmotic volume expansion Syndrome of inappropriate ADH secretion (SIADH) ISO-OSMOTIC VOLUME CONTRACTION 1. ECF Fluid change ? 2. ECF Osmolarity ? 3. ICF Osmolarity ? 4. Hematocrit ? HYPEROSMOTIC VOLUME CONTRACTION 1. ECF Fluid change ? 2. ECF Osmolarity ? 3. ICF Osmolarity ? 4. Hematocrit ? Hypo-osmotic volume contraction 1. ECF Fluid change ? 2. ECF Osmolarity ? 3. ICF Osmolarity ? 4. Hematocrit ? ISO-OSMOTIC VOLUME EXPANSION 1. ECF Fluid change ? 2. ECF Osmolarity ? 3. ICF Osmolarity ? 4. Hematocrit ? HYPEROSMOTIC VOLUME EXPANSION 1. ECF Fluid change ? 2. ECF Osmolarity ? 3. ICF Osmolarity ? 4. Hematocrit ? HYPO-OSMOTIC VOLUME EXPANSION 1. ECF Fluid change ? 2. ECF Osmolarity ? 3. ICF Osmolarity ? 4. Hematocrit ? A 23-year-old man is brought to the Emergency Department after collapsing during basketball practice. On admission he is lethargic and appears confused. His coach reports that it was hot in the gym and he was drinking a lot of water during practice. An increase in which of the following is the most likely cause of his symptoms? a. Intracellular tonicity b. Extracellular tonicity c. Intracellular volume d. Extracellular volume e. Plasma volume A 70kg man is given a treatment intravenously. The diagram shows the intracellular(ICF) volume And extracellular fluid(ECF)volume before and after treatment. Which of the following treatments was likely administered to this man? A. Hypertonic saline B. Hypotonic saline. C. Isotonic saline D. Isotonic glucose. 7.A 14-year-old boy has a craniotomy performed under general endotracheal anesthesia for removal of a craniopharyngioma. The anesthetic agent used is halothane, and when he is fully awake in the recovery room, he is extubated and sent to the floor. Five percent dextrose in one-third normal saline was dripping in his intra-venous line at a rate of 125 mL/h. Four hours later, the nurses report that he cannot be roused from a deep sleep. They also point out that his urinary output in each of those 4 hours was 1059, 1100, 980, and 1250 mL, respectively. Laboratory studies show: Sodium 156 mEq/L Osmolarity 312 mOsm/L pH 7.55 pco2 28 mm Hg Bicarbonate 24 mEq/L Which of the following best explains these findings? (A) Brain edema (B) Nephrogenic diabetes insipidus (C) Respiratory depression induced by unmetabolized anesthetic (D) Surgical trauma to the posterior pituitary (E) Water retention Oral Rehydration Therapy Is Driven by Solute Transport Oral administration of rehydration solutions has dramatically reduced the mortality resulting from cholera and other diseases that involve excessive losses of water and solutes from the gastrointestinal tract. The main ingredients of rehydration solutions are glucose, NaCl, and water. The glucose and Na+ ions are reabsorbed by SGLT1 and other transporters in the epithelial cells lining the lumen of the small intestine . Deposition of these solutes on the basolateral side of the epithelial cells increases the osmolarity in that region compared with the intestinal lumen and drives the osmotic absorption of water. Absorption of glucose, and the obligatory increases in absorption of NaCl and water, helps to compensate for excessive diarrheal losses of salt and water. The Clinical Relevance of Understanding Tonicity The importance of understanding this well is to make sure that you understand the basis and rationale for intravenous fluid therapy. Several IV fluids exist e.g. 0.9% saline(normal saline) 5% dextrose in normal saline 5% dextrose in water half normal saline 5% dextrose in half normal saline. (Dextrose is glucose). How does the clinician decide which fluid to use? Well, it depends on what the objectives are – replacement of blood volume or rehydration of cells in dehydrated individuals. Discussion on IV solutions First thing to do is to look at the relative osmolarity and tonicity of the solution to the extracellular (and intracellular) fluid. Then take into account what effect this will have on the volumes of the two fluid compartments. 1. 0.9% saline. This has the same osmolarity as the intracellular fluid. The saline is NaCl so the two particles Na and Cl are considered to be non-penetrating. Therefore this solution is isoosmotic and isotonic. Because it is isotonic it will not change the tonicity of the extracellular fluid and so the extracellular fluid will remain isotonic to the intracellular fluid. Therefore NO FLUID MOVEMENT INTO THE CELLS. This solution would be suitable for replacing blood (extracellular fluid). 2. 5% Dextrose in normal saline. 5% dextrose is iso-osmotic to the intracellular fluid, so is normal saline. Therefore you must take into account both of these when working out the overall osmolarity. This solution has twice the osmolarity of the intracellular fluid. Therefore it is HYPEROSMOTIC. Dextrose is penetrating , so makes no contribution to the tonicity of the solution. Saline is non-penetrating it does make a contribution. Therefore the solution is ISOTONIC. Infusion of this solution into the veins would not change the tonicity of the extracellular fluid so NO NET FLUID MOVEMENT INTO THE CELLS. Notice the NET. Rapid infusion of this solution will lead initially to some water movement out of the cells which will be reversed as the dextrose moves into the cells. This solution would be suitable for replacing blood. 3. 5% Dextrose in water. 5% dextrose is iso-osmotic to the intracellular fluid. Water is, of course, hypo-osmotic (it has no particles). This solution therefore is iso-osmotic to the intracellular fluid. Water has no tonicity and dextrose is penetrating . This solution has no tonicity so is HYPOTONIC to the intracellular fluid. Infusion of this solution will make the extracellular fluid hypotonic to the intracellular fluid so some of the infused fluid will enter the cell. THERE IS THEREFORE FLUID MOVEMENT INTO THE CELLS. This solution would be suitable for rehydrating cells. 4. Half normal saline. This is 0.45% saline, so has half the number of particles as normal saline so it is hypo-osmotic to the intracellular fluid. The particles are non-penetrating but again you have half the number of particles. This solution is therefore HYPOTONIC to the intracellular fluid. Infusion of this solution will make the extracellular fluid hypotonic to the intracellular fluid so some of the infused fluid will enter the cell. THERE IS THEREFORE FLUID MOVEMENT INTO THE CELLS. This solution would be suitable for rehydrating cells. 5. 5% Dextrose in half normal saline. 5% dextrose is iso-osmotic to the intracellular fluid, half normal saline is hypo-osmotic. However if you have them together in a solution the result is hyperosmotic to the intracellular fluid. Only the saline is nonpenetrating , therefore the solution is HYPOTONIC to the intracellular fluid. Infusion of this fluid will decrease the tonicity of the extracellular fluid. THERE IS THEREFORE FLUID MOVEMENT INTO THE CELLS. This solution would be suitable for rehydrating cells.