Low back pain is the fifth most common reason for all
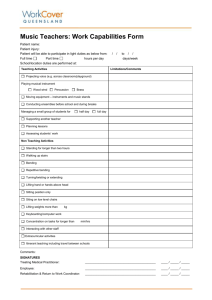
advertisement

بسم هللا الرحمن الرحیم Low back pain By dr HABIBOLLAHI 1 LBP is one of the most common subjective health complaints in Western populations. In Britain, the 1 year prevalence was 49% and in the Nordic countries the 1 month prevalence of LBP was 35%. Low back pain is one of the most frequent medical causes of absence from work, and disability arising from chronic back pain is now a major welfare and economic problem 2 Low back pain is the fifth most common reason for all physician visits in the United State Approximately one quarter of U.S. adults reported having low back pain lasting at least 1 whole day in the past 3 months, and 7.6% reported at least 1 episode of severe acute low back pain within a 1-year period One third of all disability costs in the United States are related to low back pain. 3 Differential - three broad categories: 1. 2. 3. 4 Mechanical (97%) Nonmechanical (~1%) Visceral (~2%) Differential: Mechanical LBP Lumbar Strain or Sprain (70%) Degenerative processes of disc and facets (10%) Herniated disc (4%) Osteoporotic Compression Fracture (4%) Spinal Stenosis (3%) Spondylolisthesis (2%) Traumatic Fractures (<1%) Congenital disease (<1%) Severe Kyphosis or Scoliosis Transitional Vertebrae Spondylolysis Internal Disc Disruption/Discogenic Back Pain Presumed Instability 5 Differential - Nonmechanical LBP: Neoplasia (0.7%) Multiple Myeloma Metastatic Carcinoma Lymphoma and Leukemia Spinal Cord Tumors Retroperitoneal Tumors Primary Vertebral Tumors Infection (0.01%) Osteomyelitis Septic Discitis Paraspinous Abscess Epidural Abscesss Inflammatory Arthritis (0.3%) – note HLA-B27 association. Ankylosing Spondylitis Reiter Syndrome Inflammatory Bowel Disease Scheuermann Disease (osteochondrosis) Paget Disease 6 Differential – Visceral Disease: Pelvic organ involvement: Prostatitis Endometriosis Chronic Pelvic Inflammatory Disease Renal involvement Nephrolithiasis Pyelonephritis Perinephric Abscess Aortic Aneurysm Gastrointestinal involvement 7 Pancreatitis Cholecystitis Penetrating Ulcer Interdisciplinary Team Approach to Chronic Spinal Disorders Complex Problem Interdisciplinary Management • • Physiological factors Social factors • • • • Psychological factors 8 Spine Surgeons Neurosurgeons Pain specialists Psychiatrists/ Psychologists Physiatrists Radiologists TERMINOLOGY 9 Acute low back Low back pain present for fewer than 4 weeks, sometimes grouped with subacute low back pain as symptoms present for fewer than 3 months 10 Chronic low back pain Low back pain present for more than 3 months. 11 Nonspecific low back Pain occurring primarily in the back with no signs of a serious underlying condition (such as cancer, infection, or cauda equina syndrome), spinal stenosis or radiculopathy, or another specific spinal cause (such as vertebral compression fracture or ankylosing spondylitis). Degenerative changes on lumbar imaging are usually considered nonspecific, as they correlate poorly with symptoms. 12 Radiculopathy Dysfunction of a nerve root associated with pain, sensory impairment, weakness, or diminished deep tendon reflexes in a nerve root distribution. 13 Sciatica Pain radiating down the leg below the knee in the distribution of the sciatic nerve, suggesting nerve root compromise due to mechanical pressure or inflammation. Sciatica is the most common symptom of lumbar radiculopathy 14 Spinal stenosis Narrowing of the spinal canal that may result in bony constriction of the cauda equina and the emerging nerve roots 15 Straight-leg-raise test A procedure in which the hip is flexed with the knee extended in order to passively stretch the sciatic nerve and elicit symptoms suggesting nerve root tension. A positive test is usually considered reproduction of the patient’s sciatica when the leg is raised between 30 and 70 degrees. Reproduction of the patient’s sciatica when the unaffected leg is lifted is referred to as a positive “crossed” straight-leg-raise test 16 Spondylosis A degenerative spinal disease that can involve any part of the VERTEBRA, the INTERVERTEBRAL .DISK, and the surrounding soft tissue. 17 Spondylolysis Deficient development or degeneration of a portion of the VERTEBRA, usually in the pars interarticularis (the bone bridge between the superior and inferior facet joints of the LUMBAR VERTEBRAE) leading to SPONDYLOLISTHESIS. 18 Spondylolisthesis Forward displacement of a superior vertebral body over the vertebral body below 19 Spondylarthritis Inflammation of the joints of the SPINE, the intervertebral articulations 20 Osteoarthritis, Spine A degenerative joint disease involving the SPINE. It is characterized by progressive deterioration of the spinal articular cartilage (CARTILAGE, ARTICULAR), usually with hardening of the subchondral bone and outgrowth of bone spurs (OSTEOPHYTE). 21 Spondylarthropathies Heterogeneous group of arthritic diseases sharing clinical and radiologic features. They are associated with the HLA-B27 ANTIGEN and some with a triggering infection. Most involve the axial joints in the SPINE, particularly the SACROILIAC JOINT, but can also involve asymmetric peripheral joints. Subsets include ANKYLOSING SPONDYLITIS; REACTIVE ARTHRITIS; PSORIATIC ARTHRITIS; and others 22 23 Occupational factors for low back pain Job related • • • • • • • • • Manual handling tasks Lifting Twisting Bending Falling Reaching Excessive Weights Prolonged Sitting Vibration 24 Related to Individual Prior Episode Job Dissatisfaction Smoking Obesity Genetic factors Back Safety & Lifting Common Causes of Back Injuries Heavy Lifting Twisting Reaching & Lifting Carrying & Lifting Awkward Postures Sitting or Standing 25 Slips,Trips & Falls Back Safety & Lifting Heavy Lifting Job requires heavy lifting: Use equipment when possible or ask for help. Try to avoid repetitive lifting over a long period of time. Twisting • Twisting at the waist while lifting or holding a heavy load. Reaching & Lifting • Injury usually occurs when reaching over the head, across a table or out the back of a truck. 26 Back Safety & Lifting Carrying & Lifting Awkward Positions • Inappropriate postures that can contribute to back pain are caused by poor workstation layout and/or equipment design. Slips,Trips & Falls • It is very easy to injure your back, neck or legs while slipping, tripping or falling. 27 Injury usually occurs when carrying or lifting objects with awkward or odd shapes. Back Safety & Lifting Sitting or Standing 28 Sitting or standing too long in one position. Sitting can be very hard on the lower back. For every one to two hours sitting, stand up and take a stretch. For every one to two hours standing, sit down or move around and stretch. Back Safety & Lifting Back Injury Prevention 29 Avoid lifting and bending whenever you can. Place objects up off the floor. That way you won’t have to reach down to pick them up again. Raise / lower shelves. The best zone for lifting is between your shoulders and your waist. Put heavier objects on shelves at waist level, lighter objects on lower or higher shelves. Back Safety & Lifting Back Injury Prevention Reducing exposure to known risk factors Repetition Awkward Position Force 30 Object weight Load Distribution Object friction Duration Back Safety & Lifting Back Injury Prevention Cont.: Avoid Hyper extension movements of the back. – Avoid Hyper flexion movements of the back. 31 Back Safety & Lifting Back Injury Prevention cont.: Maintain good posture Lift objects holding them close to your body Never “twist” when carrying, handling, or transferring a heavy object – Avoid “locking out” the knees – Use proper lifting techniques 32 Back Safety & Lifting 4 1 2 Assess 33 3 Plan Prepare Perform Back Safety & Lifting Assess Assess the task: Assess Your Own Capabilities: 34 Posture Pacing, rate of work, breaks Requirements for team handling Strength, height, etc. Health problems Gender, age, fitness Back Safety & Lifting Assess Cont.: Assess the Load: Assess the environment: 35 Weight, shape, size Handles, packaging Stability Contents: hot, cold, hazardous Space constraints Flooring condition, levels Temperature, humidity, ventilation Tidiness, general housekeeping Back Safety & Lifting Plan Task Route Consider start and end points 36 What is the most appropriate posture? Is there mechanical aid available? Is there anyone else to help? Can any obstructions be cleared Back Safety & Lifting Prepare Prepare the load: Prepare yourself and the area: 37 Can the load be split? Can the load be made more stable? Make sure contents are evenly distributed? Move the load’s center of gravity close to yours Cover sharp / abrasive edges Check space constraints Move obstacles Check final destination Check housekeeping Get a good grip on the load Use PPE where appropriate Back Safety & Lifting Perform Apply principles of biomechanics to reduce the load on the spine 38 Keep a wide base of support. Maintain the lumbar curve (low back) as much as possible. Get a good grip. Position feet in direction of travel. Use smooth controlled movements. Use friction to minimize force. Try to avoid twisting and stooping. Use team lifting where appropriate. Back Safety & Lifting Get close to the load Slowly Lift Proper Lifting Techniques Hug the Load Squat Down Grip the Load 39 Back Safety & Lifting Get close to the load Proper Lifting Techniques – Get as close to the load as possible with your feet wide apart about shoulder width, with one foot slightly in front of the other for balance. • Test the object’s weight before lifting it. • Ask for assistance from a co-worker when appropriate. • Have the object close to the body and put less force on the low back. • Avoid rapid, jerky movements. 40 Back Safety & Lifting Squat Down Proper Lifting Techniques Cont.: Keep yourself in an upright position while squatting to pick up. Squat by bending the knees and hips. Keep the three Curves of the Back properly aligned: 41 Ears, Shoulders, and Hips are in a straight line. Back Safety & Lifting Grip the Proper Lifting Techniques Cont.: Load Tightening the stomach helps support the spine. Do not hold your breath while tightening the muscles. Get a firm grasp of the object before beginning the lift. 42 Use both hands. Use whole hand, not just fingers. Use gloves as needed to prevent “pinched” grips or to protect the hands during lift. Back Safety & Lifting Hug the Load Proper Lifting Techniques Cont.: 43 Legs are the strongest muscles in the body – so use them. Avoid back flexion. Hold objects close to body. Slide the object from the knee on the ground to midthigh. Keep the head forward. Hug the object to your stomach & chest. Back Safety & Lifting Slowly Lift Proper Lifting Techniques Cont.: 44 Lift with the legs to allow the body’s powerful leg muscles to do the work. Flex the knees and hips, not the back. Avoid bending & twisting at the waist. Try to keep the back “straight” during the lift. Do not look down at the object during lift. Look up to help “straighten” the position of the back for a safer lift. Never Bend, Lift, and Twist at the same time. Back Safety & Lifting Torque = Load x Distance Box = 30 lbs. Body wgt = 170 lbs. L5/S1 Disk 12 in. L5/S1 Disk 36 in. 16 in. 0 in. 30 lbs. 30 lbs. 85 lbs. (30 lbs. x 36 in.) + (85 lbs. x 12 in.) = 2,100 in-lbs. (Box) 45 (Employee) 85 lbs. (30 lbs. x 16 in.) + (85 lbs. x 0 in.) = 480 in-lbs. (Box) (Employee) Back Safety & Lifting Exercises 46 Exercises that work your back, hips, thighs, and abdominal muscles can minimize back problems. Stand behind chair, hands on chair. Lift one leg back and up, keeping the knee straight. Warm up slowly and exercise regularly. Back Safety & Lifting Exercises Cont.: Starting Position: Standing tall, feet shoulder width apart, chin tucked in 47 Place your palms on the small of your back, fingers pointing down. Keep your head up as you lean back slowly as far as possible. Hold for at least 10 seconds. Return to starting position and relax. Back Safety & Lifting Exercises Cont.: Wall Squats 48 Stand with back leaning against wall Walk feet 12 inches in front of body. Keep abdominal muscles tight while slowly bending both knees 45 degrees. Hold 5 seconds. Slowly return to upright position. Repeat at least 5 to 10 times. Back Safety & Lifting Exercises Cont.: 49 Lie on the floor on back. Keeping arms folded across chest, tilt pelvis to flatten back, chin tuck into chest. Tighten abdominal muscles while raising head and shoulders from floor. Hold at least 10 seconds and release. Repeat at least 5 to 10 times. Back Safety & Lifting • Summary – Common Causes Of Back Injuries Heavy Lifting Twisting Reaching & Lifting Carrying & Lifting Awkward Positions Sitting or Standing Slips, trips, and falls – Back Injury Prevention • Reduce exposures to known risk factors 50 Back Safety & Lifting • Summary Cont.: – Principles of Safe Handling Assess Plan Prepare Perform – Proper Lifting Techniques • Close • Squat • Grip • Hug • Slowly – Exercise-Should You?---of course!!! 51 Imaging 52 Plain Radiography: Most common spinal imaging test. Low cost and ready availability. AP and Lateral views demonstrate alignment, disc and vertebral body height, and gross assessment of bone density and architecture. Sacroiliitis occurs early in Ankylosing spondylitis and is readily detected by plain films. Agency for Health Care Policy and Research Guidelines currently do not recommend routine oblique and spot lateral views. Get oblique if you suspect spondylolysis; good for pars interarticularis. Get flexion and extension films if you suspect lumbosacral instability. Get angled sacral views if you suspect ankylosing spondylitis. Caution using lumbar radiography repeatedly, may damage the gonads, particularly in reproductive age females. 53 Plain Films - Weaknesses: Neoplasm - ~50% trabecular bone loss prior to becoming visible Infection – similar, relatively late appearance of change Inability to distinguish acute from chronic compression fractures Disc herniation Spinal Stenosis 54 CT + MRI: CT Strengths: MRI Strengths: Axial bony anatomy Cortical bony destruction Facet degenerative changes Disk herniation Soft tissue evaluation in patients who cannot undergo MRI secondary to claustrophopia or implanted metal. CT Myelography good for bony causes of spinal stenosis CT Weaknesses: Discogenic disease (nucleus pulposis rupture, annulus fibrosis tears) Spinal canal contents Discitis MRI Weaknesses: 55 Better soft tissue contrast than CT Visualization of disc Ligamentous pathology Vertebral marrow and spinal canal Neoplasm Infection (may be the best modality with gadolinium enhancement) Disc Herniation Spinal stenosis Nerve root impingement Cannot detect cortical bone Common degenerative disk disease and disease of facet joints – too nonspecific Fractures seen best in the axial plane Subtle annular tears Bone Scans: While plain films, CT, and MRI detect bony morphology, bone scintigraphy detects biochemical changes in bone. Most useful in detecting the age of compression fractures. Old fractures will appear “cold” while new fractures will appear “hot”. Very useful for determining primary bony tumors (usually benign, i.e. osteoid osteoma, osteoblastoma, aneurysmal bone cyst, and osteochondroma) degree of metastasis and certain infections (infectious spondylitis in particular – gallium67 when compared with MRI had better specificity and sensitivity). Useful for subtle fractures and infarction. Useful for metabolic bone disease such as Paget Disease. 56 Discography: Controversial method for diagnosing discogenic pain. Used to delineate whether suspicious discs found on MRI were the true cause of the patients’ pain. However, the use of discography as an indicator of general disk disease has been found to be suspect. One study by Holt, et al., found 38% positive rate when they tested healthy subjects. Can we utilize a test with that degree of inaccuracy? Recent studies have shown a lower degree of specificity but the jury is still out. Good for posterolateral annulus fibrosis tears when CT is used to visualize the tears with contrast enhancement. 57 Cases: 58 Lateral radiograph showing decreased disk space between L5 and S1. Consistent with Osteoarthritis and Degenerative Disk Disease. 59 Lateral radiograph showing grade 1 spondylolishthesis. (Grades correspond to how far forward the posterior border of the spinous process slides along the sacral platform. Grade 1 = 1-25%, 2 = 2650%, 3 = 51-75%, 4 = 76-100%.) 60 Saggital MRI showing central disk herniation at L5-S1. 61 Severe lumbar degenerative disk disease and osteoarthritis. What are the four cardinal features of OA? 62 1. Joint Space Narrowing 2. Osteophytic Spurring 3. Subchondral Sclerosis 4. Subchondral Cysts Frontal and lateral radiograph showing L2 compression fracture. How old is this fracture? Can you tell? No – get a bone scan. 63 Multiple acute compression fractures in an elderly female. Image on right is status-post multiple serial vertebroplasties. 64 What kind of patient presents with spondylolysis? Image on right is oblique view of lumbar spine. Adolescent athletes. Males>Females 2-3:1. Caucasions>African Americans 3:1. Gymnasts and Football Players are the two most frequent types of athletes affected. 65 66 Saggital T1 weighted MRI of the spine showing bony metastases to the distal thoracic spine. Breast cancer primary. 67 Osteomyelitis. Image is a saggital T1 weighted image showing osteomyelitis of the lumbar spine at L2-L3. Enterococcus was isolated. 68 69 Frontal radiograph showing syndesmophytes bridging the intervetebral spaces. Ankylosing Spondylitis: Sacroiliac joints and axial spine undergo progressive ossification. Ensethoopathy (ossification of ligamentous attachments) is also characteristic. Onset is typically in young people, usually teens or twenties. Presents as a persistent bachache which is not relieved by rest and improves with exercise. If you suspect AS, an angled plain film of the pelvis is the best modality along with AP and lateral films of the lumbar spine. 70 A technetium 99m-bisphosphonate bone scan of a patient with polyostotic Paget's disease. 71 Young patient with progressive kyphosis. Diagnosis is? Scheuermann Disease! Because I knew you were all dying to know what that is. Scheuermann disease (juvenile kyphosis) is a deformity in the thoracic or thoracolumbar spine in children secondary to osteochondrosis of the secondary ossification centers of the vertebral bodies. 72 73 74 75 76 77 Disc Degeneration: chemical changes associated with aging causes discs to weaken, but without a herniation. Prolapse: the form or position of the disc changes with some slight impingement into the spinal canal. Also called a bulge or protrusion. Extrusion: the gel-like nucleus pulposus breaks through the tire-like wall (annulus fibrosus) but remains within the disc. Sequestration or Sequestered Disc: the nucleus pulposus breaks through the annulus fibrosus and lies outside the disc in the spinal canal Disc Degeneration 78 Summary: Plain Radiography remains the mainstay as the initial test of choice. CT can help delineate axial pathology, particularly bony fractures impinging on nerve roots. Discography has limited utility due to unacceptably high false positive rates. Bone scans are good for determining the age of fractures, the extent of neoplastic spread, and metabolic bone disease. MRI is good for everything else, particularly infections (most), disc herniations, and ellucidation of spinal and neural root pathology. 79 80 81 82 83 84 85 86 87