DRAFT-Patient-contact-protocol-for-patients-with-high
advertisement

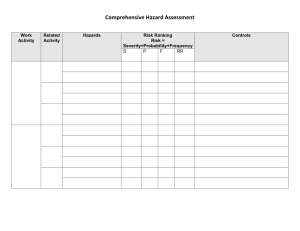
DRAFT National patient contact protocol for patients with Implanted Medical Devices subject to Hazard Alerts Version 0.6 i Contents PART 1 – PRELIMINARY ISSUES ............................................................................................................... 1 A. Introduction ........................................................................................................... 1 B. Hazard Alerts ......................................................................................................... 3 C. Scope of the Protocol ............................................................................................ 5 D. Stages of the Protocol ........................................................................................... 6 E. The role of State/Territory recall co-ordinators .................................................... 7 PART 2 – PREPARATION .......................................................................................................................... 8 F. Adopting a Hazard Alert Management Policy ....................................................... 8 G. Appointing persons responsible ............................................................................ 8 H. Establishing a Hazard Alert Committee ................................................................. 8 I. Managing implanted device data .......................................................................... 9 Collecting implanted device data .......................................................................... 9 Documenting and testing data retrieval processes ............................................. 11 J. Registering with Health Professional Online Services ......................................... 11 K. Identifying Hazard Alerts ..................................................................................... 11 PART 3 – RESPONSE .............................................................................................................................. 12 L. Managing a Hazard Alert ..................................................................................... 12 Initiating the Healthcare Organisation’s response .............................................. 12 Planning for patient contact ................................................................................ 12 Identifying affected patients ............................................................................... 13 Contacting patients ............................................................................................. 14 Following up patients unable to be contacted .................................................... 14 Responding to inquiries ....................................................................................... 15 Maintaining appropriate records ........................................................................ 15 PART 4 – RECOVERY .............................................................................................................................. 16 M. Evaluating and reporting management and outcomes ....................................... 16 N. Supporting system level accountability............................................................... 17 DICTIONARY .......................................................................................................................................... 18 DEVICE DATASET TO BE HELD AT HOSPITAL LEVEL - FORMAT ............................................................. 20 ii COMMISSION SPONSOR Professor Debora Picone AM PROGRAM DIRECTOR Mr Neville Board, Director, Information Strategy and Safety in eHealth AUTHOR Dr Heather Wellington, DLA Piper Version control (Document Revision History) Version Date Comment 0.1 0.2 0.3 0.4 0.5 18 December 2013 20 December 2013 23 December 2013 28 January 2014 9 April 2014 0.6 5 May 2014 Dr Wellington Comments N.Wilcox, T.Snioch Revisions incorporated Revisions incorporated Revised following jurisdictional, Commission Executive and private hospital sector feedback Minor revisions Distribution Date Issued Issued To 0.1 – 18 December 2013 0.3 – 23 December 2013 0.4 – 28 January 2014 0.5 – 10 April 2014 0.6 – 7 May 2014 0.6 – 9 May 2014 Project group DRAFT submitted to Dept of Health ACSQHC Inter-Jurisdictional Committee Commission Executive review Hospitals participating in the Proof of concept phase Jurisdictional Recall Coordinators, ACSQHC Executive, Dept of Health This is a managed document. For identification of amendments each page contains a version number and a page number. Changes will only be issued as complete replacements covered by a release notice. This document has not been released for use until authorised by the last signatory. Authorised for release to the Department of Health: …………………………………………………………………………………………. (___/___/___) Professor Debora Picone, AM iii PART 1 – PRELIMINARY ISSUES A. Introduction The Australian Government, through the Department of Health and in consultation with State and Territory health authorities and the private healthcare sector, has developed this national patient contact protocol (‘Protocol’) for application by Healthcare Organisations when implanted medical devices are subject to Hazard Alerts. The Uniform Recall Procedure for Therapeutic Goods (‘URPTG’), which is the result of an agreement between the therapeutic goods industry and the Commonwealth and State/Territory health authorities, defines the actions to be taken by health authorities and sponsors when therapeutic goods for use in humans, for reasons relating to their quality, safety or efficacy, are to be removed from supply or use, or subject to corrective action. The URPTG does not, however, specify how patients with Implanted Medical Devices should be contacted when those devices are subject to Hazard Alerts. In its reports: The Regulatory Standards for Approval of Medical Devices in Australia1 and The Role of the Therapeutic Goods Administration Regarding Medical Devices, Particularly Poly Implant Prostheses (‘PIP’) Implants2, the Senate Community Affairs Reference Committee noted significant deficiencies in arrangements for contacting patients in these circumstances. This Protocol defines the procedures that should be implemented by Healthcare Organisations when Implanted Medical Devices are subject to Hazard Alerts. It is based on the following principle: Contacting individuals with Implanted Medical Devices that are subject to a Hazard Alert, and providing them with appropriate information and access to necessary services is: a. b. c. d. a patient and consumer right; a core responsibility of the health care system; a normal part of an episode of care should the unexpected occur; and a critical element of clinical communications. The Protocol: complements the URPTG; will support Healthcare Organisations and clinicians to make reliable, sensitive and timely contact with patients with Implanted Medical Devices that are subject to Hazard Alerts; has a consumer focus; reflects opinions as to ‘best practice’ expressed by stakeholders who participated in a consultation process; and 1 The Senate. Community Affairs Reference Committee. The regulatory standards for the approval of medical devices in Australia. November 2011. 2 The Senate. Community Affairs Reference Committee. The role of the Therapeutic Goods Administration regarding medical devices, particularly Poly Implant Prostheses (PIP) Implants. May 2012. 1 supports good governance at an organisational and system level. The Protocol is accompanied by an implementation guide: Guide to implementing the National Patient Contact Protocol. Important notice This Protocol does not limit, affect or alter the obligations or duties in respect of Implantable Medical Devices imposed on any person by or under any contract, common law or legislation. To the extent that this Protocol is or may be inconsistent with anything in the URPTG or the Australian Regulatory Guidelines for Medical Devices, the URPTG and those Regulatory Guidelines shall take precedence. 2 B. Hazard Alerts Therapeutic goods including Implantable Medical Devices may be recalled when, for reasons relating to their quality3, safety or efficacy, they are to be removed from supply or use, or subject to corrective action. Recalls of therapeutic goods are governed by Section 23 of the Australian Regulatory Guidelines for Medical Devices and are implemented in accordance with the URTPG. A Hazard Alert, which is a type of Recall subject to the URPTG, is the issuing of precautionary information about an implanted medical device. Recalls (including Hazard Alerts) are defined according to the following European classification system: a. b. c. Class I Recalls occur when products are potentially life-threatening or could cause a serious risk to health. Class II Recalls occur when product defects could cause illness or mistreatment, but are not Class I. Class III Recalls occur when product defects may not pose a significant hazard to health, but withdrawal may be initiated for other reasons. The level to which a Recall (including a Hazard Alert) action is undertaken is based on the significance of the risk and the channels through which the goods have been distributed. The Recall levels are: a. b. c. d. Wholesale - includes wholesalers and state/territory purchasing authorities. Hospital - includes nursing homes and institutions, hospital pharmacists, ambulance services, blood and tissue banks and laboratories as well as wholesale as appropriate. Retail - includes retail pharmacists, medical, dental and other health care professionals as well as wholesale and hospital as appropriate. Consumer - includes patients and consumers, as well as wholesale, hospital and retail levels as appropriate. Device Sponsors are primarily responsible for implementing Recalls (including Hazard Alerts). Most Recalls are initiated by Sponsors in consultation with the Therapeutic Goods Administration (‘TGA’). Overall responsibility for coordinating Recalls lies with the Australian (Commonwealth) Recall Coordinator, who is an officer of the TGA. The agreement of the Australian Co-ordinator is required before Sponsors implement any recall strategies. Each State and Territory health authority also nominates an officer, and some also nominate a deputy, through whom information relating to Recalls is channelled and coordinated. Once a Hazard Alert has been initiated, the TGA notifies a number of key stakeholders including State and Territory health authorities. The TGA has a standard operating procedure to alert the Chief Medical Officer (‘CMO’), State and Territory Chief Health Officers (‘CHOs’) and professional organisations (as appropriate) of certain Recall actions. The URPTG requires Sponsors to notify defined individuals and organisations about Hazard Alerts in an agreed written format, but does not define a specific requirement for Sponsors, Healthcare 3 That is, compliance with statutory or agreed standards. 3 Organisations or clinicians to ensure patients with Implanted Medical Devices are contacted regarding Hazard Alerts. Nor does it provide for verification of the success of efforts to contact patients. If the depth of a device Recall is to consumer level and consumers cannot be identified, Sponsors are required to insert advertisements in the daily print media of each State/Territory in which distribution has possibly taken place. Following receipt of a Hazard Alert, public hospitals currently assume responsibility for contacting patients with the relevant Implanted Medical Devices, but some report that they have experienced considerable difficulty retrieving the necessary patient identification and contact information. Coordinating and accounting for patient contact has also been challenging in some circumstances. In the private sector practices vary. Some private Healthcare Organisations assume direct responsibility for identifying patients in whom devices subject to a Hazard Alert have been implanted, but many rely on the visiting medical officers who implanted the relevant devices in their private patients to identify and contact those patients. Across both the public and private sectors, governance arrangements and the effectiveness of patient contact efforts vary considerably. This Protocol defines the procedures that should be implemented by Healthcare Organisations to ensure reliable, sensitive and timely patient contact and to establish appropriate organisational governance of Hazard Alerts. 4 C. Scope of the Protocol The Protocol defines ‘best practice’ arrangements for Healthcare Organisations to manage and govern Class I and Class II Hazard Alerts, including arrangements for: collecting and storing information necessary for the future identification of patients who undergo implantation of medical devices; retrieving information necessary to identify and contact patients with Implanted Medical Devices when a Hazard Alert is issued; collaborating with clinicians to contact and advise patients with Implanted Medical Devices that are subject to Hazard Alerts; evaluating the outcomes of patient identification and contact efforts; and reporting to their State/Territory Recall Co-ordinator. The Protocol notes the role of State/Territory Recall Co-ordinators in supporting the management of Hazard Alerts and assumes that State/Territory Recall Coordinators and/or CHOs may provide Healthcare Organisations in their jurisdictions with nationally consistent information about the appropriate timelines for patient contact, together with template information that they can provide to patients. The Protocol does not, however, address the processes for producing such information or communicating it to Healthcare Organisations. The Protocol also does not address: responsibility for provision of and/or payment for health care required by patients with Implanted Medical Devices that are subject to Hazard Alerts; or ownership and/or disposition of Implanted Medical Devices following their Explantation. 5 D. Stages of the Protocol The Protocol complements the URPTG. The URPTG is divided into seven stages and the Protocol is divided into four parts – preliminary issues, preparation, response and recovery (Figure 1). Figure 1: Stages of URTPG and Patient Contact Protocol URTPG recall stage Protocol part / stage Procedure Responsibility Protocol section 1 Notification to the Coordinator Crisis Management Sponsor N/A 2 Information required to assess Recall Sponsor N/A 3 Assessment of Recall Sponsor and Australian Recall Co-ordinator N/A 4 Recall Sponsor N/A Sponsor N/A May include recall letters, paid advertisements in the daily print media and media releases as approved by the TGA 5 Notification to the Federal Minister responsible for Consumer Affairs PART 1 - PRELIMINARY ISSUES 1 Introduction N/A A 2 Hazard Alerts N/A B 3 Scope of the Protocol N/A C 4 Stages of the Protocol N/A D 5 The role of State/Territory Recall Co-ordinators State/Territory health authorities E PART 2 – PREPARATION 6 Adopting a Hazard Alert management policy Healthcare Organisation F 7 Appointing persons responsible Healthcare Organisation G 8 Establishing a Hazard Alert Committee Healthcare Organisation H 9 Managing implanted device data Healthcare Organisation I 10 Identifying Hazard Alerts Healthcare Organisation, clinicians and others J Healthcare Organisation and relevant clinicians K PART 3 – RESPONSE 11 Implementing the Hazard Alert management system PART 4 – RECOVERY 12 Evaluating and reporting outcomes Healthcare Organisation and relevant clinicians L 13 Supporting system level accountability Healthcare Organisation M Sponsor N/A Australian Recall Coordinator N/A 6 Progress of Recall and report 7 Follow-up action 6 E. The role of State/Territory recall co-ordinators Subject to local arrangements, State/Territory Co-ordinators may assume a co-ordinating and/or governance role in relation to Hazard Alerts, which may include: maintaining an up-to-date contact list of Hazard Alert Co-ordinators in their jurisdictions; when a Hazard Alert is issued: o contacting Hazard Alert Co-ordinators in their jurisdictions to determine the number of patients potentially affected by the Hazard Alert; o supporting Hazard Alert Co-ordinators to access up-to-date information from the TGA, the Supplier, the CMO, the CHO and other relevant sources; o ensuring Hazard Alert Co-ordinators have access to agreed national advice on: the information that should be provided to patients with implanted devices that are subject to the Hazard Alert; the time frames within which patients should be contacted; o monitoring the effectiveness of management of the Hazard Alert; o creating a central point in the jurisdiction for communication about management of the Hazard Alert; o reporting outcomes of management of the Hazard Alert locally and nationally in accordance with agreed protocols; and supporting Healthcare Organisations to take a continuous quality improvement approach to the management of Hazard Alerts. 7 PART 2 – PREPARATION F. Adopting a Hazard Alert Management Policy 1. Healthcare Organisations should issue a policy (‘Hazard Alert Management Policy’) confirming their intent to adopt this Protocol and their approach to its implementation. G. Appointing persons responsible 2. Healthcare Organisations should: a. nominate a position or individual to assume responsibility for coordinating the management of Hazard Alerts (the Hazard Alert Co-ordinator) in each Healthcare Facility, and ensure they have appropriate delegated authority to undertake the responsibilities detailed in this Protocol; b. nominate an alternative position or individual to assume responsibility for coordinating the management of Hazard Alerts in the event the Hazard Alert Co-ordinator is unavailable; c. define and promulgate the role and responsibilities of the Hazard Alert Coordinator; and d. nominate the position or individual who is responsible for generating patient contact lists in the event of a Hazard Alert, and a second position or individual to assume delegated responsibility for list generation in the event that the responsible person is unavailable. The Hazard Alert Co-ordinator and their alternative should be senior medical, nursing or allied health professionals. Healthcare Organisations should notify State/Territory Recall Co-ordinators of the names and contact details of the Hazard Alert Co-ordinator and their alternative. 3. 4. H. Establishing a Hazard Alert Committee 5. Healthcare Organisations should establish a committee (‘Hazard Alert Committee’) to advise the Hazard Alert Co-ordinator on the management of Hazard Alerts. The Hazard Alert Committee should be chaired by a member of the Healthcare Organisation’s senior management team. 6. 8 I. Managing implanted device data Collecting implanted device data 7. 8. 9. 10. Healthcare Organisations, with the support of clinicians, should: a. develop and implement procedures to ensure the data described in Table 1 are collected and accurately recorded in patient medical records for all episodes of care in which a Implantable Medical Device is implanted in or explanted from an patient; b. make all reasonable efforts to: i. record standardised data, as described in Table 1, in searchable electronic systems (e.g. patient administration/ management system, theatre management system or other searchable database); and ii. maintain the currency of those data over time; c. in accordance with their obligations under privacy law: i. inform patients, when the relevant data are collected, that they may be stored, used or disclosed for the purpose of effecting patient contact in the event of a Hazard Alert; ii. advise patients with Implanted Medical Devices that they should always inform the Healthcare Organisation and Medicare Australia, in writing and in a timely manner, of any changes to their permanent contact details; d. include device-identifying data in patient-held discharge summaries and discharge information sent to patients’ general practitioners and, if applicable, other referring clinicians. For additional patient contact options, Healthcare Organisations may also choose to collect the email addresses and mobile telephone numbers, where available, of each patient in whom an Implantable Medical Device has been implanted. Healthcare Organisations should retain the data described in Table 1 in an accessible format and location for all patients with Implanted Medical Devices for the minimum statutory retention period following device explantation or patient death, but should thereafter destroy or permanently de-identify data if no longer required for any purpose. If data referred to in Table 1 are recorded in patients’ medical records and/or other location(s) but are not stored in a searchable format, Healthcare Organisations may establish a systematic process to retrieve those data and record them in a searchable format. 9 Table 1: Data items to be held by Healthcare Organisations Data item Patient identifier information Person Identifier (NHDD4). Identifiers for individual patients that will support patient contact and Recall include: Name (full name including middle names) Medicare number (including individual reference number) Healthcare Facility medical or unit record number Patient date of birth and gender Patient address at the date and time of implant, updated as relevant during subsequent contacts with the health care facility Where the patient is a child or an incompetent adult, the name and address of the patient’s substitute decision-maker. Device identifier information5 Device identifier (DI) Production identifier (PI) These elements respectively identify the device and provide production information such as batch or serial number information that combine to form a Unique Device Identifier (UDI): UDI = DI + PI Provider identifier Clinician identifier Date of admission for implantation, revision or explantation procedure 4 NHDD: National Health Data Dictionary, version 16 see http://www.aihw.gov.au/publicationdetail/?id=10737422826. 5 International Medical Device Regulators Forum (IMDRF), UDI Guidance: Unique Device Identification (UDI) of Medical Devices, see: http://www.imdrf.org/docs/imdrf/final/technical/imdrf-tech-131209-udi-guidance.pdf 10 Documenting and testing data retrieval processes 11. Healthcare Organisations should: a. document a procedure for data retrieval that will enable timely and reliable retrieval of patient-, device- and provider-identifying data for all Implanted Medical Devices; and b. undertake a practical test, and periodically review the effectiveness, of the data retrieval procedure. Note: Notwithstanding clause 7.b7.b.i, arrangements to store, search and retrieve data necessary to identify patients with specific Implanted Medical Devices will vary between Healthcare Organisations and Facilities. For example, some Healthcare Organisations may collect relevant data in searchable electronic patient records, while others may rely on extracting inventory and/or procedure data from searchable electronic systems supported by manual searches of patient records. Procedures for generating patient contact lists will vary, therefore, between Healthcare Organisations and Facilities, but should be documented in accordance with local arrangements and tested periodically. J. Registering with Health Professional Online Services 12. Healthcare Organisations should register with Medicare’s Health Professional Online Services (‘HPOS’) to enable future access patient contact information held by Medicare6. K. Identifying Hazard Alerts 13. The Hazard Alert Co-ordinator should regularly monitor the TGA website for new Hazard Alerts. Healthcare Organisations should establish a policy requiring staff and visiting medical officers to inform the Hazard Alert Co-ordinator if they are notified of a relevant Hazard Alert. 14. 6 More information about HPOS is provided in the Guide to implementing the National Patient Contact Protocol. 11 PART 3 – RESPONSE L. Managing a Hazard Alert Initiating the Healthcare Organisation’s response 15. When a Hazard Alert is received, the Hazard Alert Co-ordinator should: a. immediately ensure all Implantable Medical Devices subject to the Hazard Alert that remain in stock are quarantined; b. report the receipt of the Hazard Alert to the relevant Healthcare Organisation or Facility quality, clinical governance and/or risk management committee(s); and c. convene the Hazard Alert Committee; d. establish a log of key tasks; and e. assign responsibilities and preliminary timeframes for completion of all tasks. Planning for patient contact 16. The Hazard Alert Co-ordinator, in collaboration with relevant clinicians and with advice from the Hazard Alert Committee, and taking into account the technical and clinical advice available about the hazard, its urgency and management (including advice from the CMO and/or the jurisdictional Recall Co-ordinator, if available), should: a. document a patient contact protocol that includes: i. the preferred mode(s) of patient contact (e.g. telephone, letter or a combination of contact modalities) and the order in which they will be effected; ii. who will contact patients; iii. the target timeframe for contacting patients; iv. key messages to be provided to patients, including: A. factual advice about the nature and significance of the hazard and its recommended management, consistent with the advice provided to the Healthcare Organisation or Facility by the Sponsor, the TGA, the Commonwealth CMO, the relevant professional college(s), the State/Territory CHO and/or the State/Territory Recall Co-ordinator; B. details of specific actions the patient is advised to take to protect their health and wellbeing (for example, initiate an immediate consultation with their general practitioner or specialist); C. details of a contact telephone number for patient to make inquiries; and D. a request for the patient or their family/carer to contact the Healthcare Organisation or Facility within a specified 12 17. timeframe to confirm they have received the advice about the Hazard Alert; b. draft template patient contact letters, where required; c. prepare tools (e.g. standard forms) to record the outcome of each patient contact; d. ensure adequate resources are available to provide appropriate clinical support to patients including, where necessary: i. specialist consulting services; ii. theatre time and/or resources; and/or iii. a telephone inquiry line staffed by trained health care professionals; and e. identify and train the staff who will be responsible for interacting with patients; f. consider whether inquiries from the public are likely and if so, implement appropriate training and provide appropriate resources for Healthcare Organisation and/or Facility personnel who may receive those inquiries. Arrangements for clinical interventions are outside the scope of this protocol. In collaboration with clinicians the Hazard Alert Co-ordinator should, however, commence developing procedures addressing: a. any special elements of consent procedures needed to support the subsequent clinical management of patients affected by the Hazard Alert; b. the need for comprehensive documentation in patient clinical records of: i. the clinical interventions undertaken in response to the Hazard Alert; ii. where explantation occurs, the observed state of the Implanted Medical Device; c. any testing, photography or other procedures proposed to be conducted on explanted devices; and d. the disposition of devices that are explanted as a result of a Hazard Alert, noting that: i. the safety of individuals potentially exposed to explanted devices must be a priority; and ii. legal ownership of explanted devices may vary depending on contractual arrangements. Identifying affected patients 18. The Hazard Alert Co-ordinator should: a. in collaboration with relevant personnel (e.g. procurement, supply and clinical personnel): i. determine how many of the Implantable Medical Devices that are subject to the Hazard Alert have been purchased by the Healthcare Organisation; ii. consider whether any of the Implantable Medical Devices that are subject to the Hazard Alert have, or may have, been supplied by visiting medical officers directly for patient use, and therefore will not appear on usual hospital supply/inventory records; 13 iii. b. determine the number of patients in whom the Implantable Medical Device that is subject to the Hazard Alert has been implanted; and activate the documented procedure referred to in clause 11 to generate a patient contact list. Contacting patients 19. 20. 21. 22. The Hazard Alert Co-ordinator should provide to the Healthcare Organisational staff members and/or clinicians who have been allocated responsibility for effecting patient contact: a. the patient contact list(s) generated in accordance with the documented procedure referred to in clause 11; b. where contact will be made by telephone, written advice of the information to be conveyed to patients; c. where contact will be made by letter, template patient contact letters; d. tools to record the outcomes of patient contact efforts; and e. the agreed method and timelines for reporting the results of patient contact efforts to the State/Territory Recall Co-ordinator. Written communications with patients should always be signed by a senior manager or clinician, whose identity is clear. Unless exceptional circumstances apply, all verbal communications with patients about Hazard Alerts should be by senior healthcare professionals with specific knowledge of both the implant that is subject to the Hazard Alert and the hazard that has been identified. The person(s) responsible for effecting patient contact should, in accordance with the parameters defined in clause 15.d15.d: a. make patient contact as expeditiously as possible; b. maintain accurate records in the agreed format of the outcomes of both successful and unsuccessful patient contact efforts; and c. submit those records to the Hazard Alert Co-ordinator in a timely manner. Following up patients unable to be contacted 23. 24. 25. Where the agreed patient contact procedures are followed but the Hazard Alert Coordinator is unable to reliably verify that an affected patient has been contacted, the Hazard Alert Co-ordinator should: a. if the urgency of the situation permits, make further patient contact efforts; b. if the patient cannot be contacted, utilise HPOS to identity the patient’s current contact details as recorded in the Medicare customer database. Following receipt from Medicare Australia of the patient’s current contact details as recorded in the Medicare customer database, the Hazard Alert Co-ordinator should repeat the step defined in clause 22 above. Healthcare Organisations or Facilities should add an alert to the medical record of each patient with an Implanted Medical Device that has been subject to a Hazard Alert if the patient has not been contacted, to ensure that if the patient contacts the Healthcare Organisation or Facility in the future the relevant information will be provided to them. 14 Responding to inquiries 26. Subject to privacy and confidentiality obligations: a. the Healthcare Organisation should: i. provide accurate and timely responses to members of the public and/or patients who initiate inquiries about the Hazard Alert; ii. consider establishing a ‘fast track’ process to provide specific device information in writing to patients who have received an implant of a similar type but are unsure whether their particular device is subject to a Hazard Alert, which: A. minimises time delays and inconvenience for patients; B. is appropriately recorded; and C. does not incur any cost for patients. iii. maintain accurate records of all relevant inquiries and responses; b. the Hazard Alert Co-ordinator should respond to all relevant inquiries by the State/Territory Recall Co-ordinator, the TGA/Australian Recall Coordinator and/or the CHO about the progress and/or effectiveness of the Hazard Alert management process. Maintaining appropriate records 27. The Hazard Alert Co-ordinator should ensure accurate records of the processes and outcomes of the Hazard Alert management process are maintained, including a. the number of affected patients; b. records of all committee meetings and correspondence (email and other) about the Hazard Alert and its management; c. a log of all telephone calls relating to the Hazard Alert and its management, including a summary of issues discussed; d. date(s) letters are sent and/or telephone calls are made to patients; e. date(s) patient contact is confirmed; f. date(s) patients are reviewed by a clinician (if applicable); g. date(s) of receipt of returned written communications to patients; h. date of accessing the HPOS system to ascertain further contact details from the Medicare customer service database; i. identified adverse events associated with the Hazard Alert and/or the device that is the subject of the Hazard Alert; j. a log of complaints and other consumer feedback about the process; and k. outcomes of patient contact efforts. 15 PART 4 – RECOVERY M. Evaluating and reporting management and outcomes 28. When implementation of the Hazard Alert management plan is completed, the Hazard Alert Co-ordinator should: a. collate data and other information relevant to the organisation’s performance in managing the Hazard Alert; b. lead a local review of the timeliness, efficiency and effectiveness of management of the Hazard Alert incorporating: i. engagement of relevant local personnel including the organisational risk and quality assurance managers and participating clinicians; ii. review of data and other information relevant to the organisation’s performance in managing the Hazard Alert; and iii. identification of potential improvements; c. lead implementation of improvements identified in step b above; d. prepare a final report including: i. a reconciliation of the patient contact list with the patients contacted; ii. an assessment of the effectiveness of management of the Hazard Alert; and iii. specific recommendations for improvement; e. submit the final report, as appropriate, to: i. relevant clinicians; ii. the Healthcare Organisation or Facility quality manager and/or risk manager; iii. relevant Healthcare Organisation and/or Facility quality, clinical governance and/or risk management committees; and f. subject to relevant Healthcare Organisational protocols and privacy and confidentiality obligations, submit the final report, as appropriate, to State and Territory Recall Co-ordinators. 16 N. Supporting system level accountability 29. Subject to relevant healthcare organisational protocols and privacy and confidentiality obligations, the Hazard Alert Co-ordinator should respond in a timely manner to requests for information about the effectiveness of implementation of this Protocol from: a. the State/Territory Recall Co-ordinator; b. the CHO; c. the Sponsor; d. the TGA and/or e. any other relevant authority. END OF PROTOCOL 17 DICTIONARY Active Implantable Medical Device means an active medical device, other than an Implantable Medical Device, that is intended by the manufacturer: (a) (b) either: (i) to be, by surgical or medical intervention, introduced wholly, or partially, into the body of a human being; or (ii) to be, by medical intervention, introduced into a natural orifice in the body of a human being; and to remain in place after the procedure. Active Medical Device means Hazard Alert means the issuing of precautionary information about an implanted device. Hazard Alert Co-ordinator means the person appointed from time to time to assume the responsibilities of coordinating the management of Hazard Alerts in a Healthcare Organisation or Facility. Healthcare Facility means any facility in which an implantable device is implanted in a human being. It includes hospitals, day procedure centres and professional consulting suites. Healthcare Organisation means any organisation that operates one or more facilities in which implantable devices are implanted in human beings. Explantation means the removal of an Implanted Medical Device from a patient’s body. Implantable Medical Device means a medical device (other than an Active Implantable Medical Device) that is intended by the manufacturer: a. b. c. to be, by surgical intervention, wholly introduced into the body of a human being, and to remain in place after the procedure; or to replace, by surgical intervention, an epithelial surface, or the surface of an eye, of a human being, and to remain in place after the procedure; or to be, by surgical intervention, partially introduced in to the body of a human being, and to remain in place for at least 30 days after the procedure. Implanted Medical Device means an Implantable Medical Device or an Active Implantable Medical Device that has been implanted in a patient. Recall means the permanent removal of therapeutic goods from supply or use for reasons relating to deficiencies in the quality, safety or efficacy of the goods. It includes: a. b. requests to pharmacists, hospitals, pathology laboratories, fractionators, operating and research facilities, biomedical engineers or others to check and return goods found to be defective; and removal from supply or use of goods with inherent design or manufacturing defects. 18 Sponsor means the person, business or company that has the primary responsibility for the supply, including for clinical investigational use, of the product in Australia. The Sponsor may also be the manufacturer of goods. State/Territory Recall Co-ordinator means the person(s) appointed from time to time by each State and Territory to coordinate recalls of therapeutic goods in their jurisdictions. 19 DEVICE DATASET TO BE HELD AT HOSPITAL LEVEL - FORMAT [Pending] 20