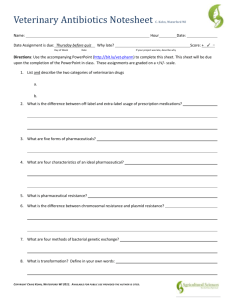
Antibiotics
advertisement

Antimicrobial agents I. Introduction Pharmacognosy IV PHG 423 Dr/ Abdulaziz Saeedan Pharmacy College 1 Antimicrobial agents Antimicrobial agents are compounds that either kills or prevents the growth and multiplication of microorganisms such as bacteria, viruses, fungi or protozoa. They are used to prevent or treat infectious diseases. There are 2 groups of antimicrobial agents used in the treatment of infectious diseases: 1- Antibiotics, which are natural substances produced by certain groups of microorganisms. 2- Chemotherapeutic agents, which are chemical substances that are completely synthesized. NOTES: o Penicillin was the first antibiotic to be discovered by Sir Alexander Fleming in 1928. o Chemotherapeutic agents were originally those employed against infectious microbes, but the term has been broadened to include anticancer drugs. o In the medical and pharmaceutical fields, all these antimicrobial agents used in the treatment of infectious diseases are referred to as antibiotics. 2 Sources of Antibiotics 1- Natural – These are antibiotics that isolated from fungal and bacterial sources. Ex: Benzylpenicillin (from penicillum notatum) and streptomycin (from Actinomycetes sp) 2- Semi-synthetic – These are antibiotics that isolated from fungal or bacterial sources then modified chemically in the Lab. • Semi-synthetic drugs were developed to decrease toxicity and increase effectiveness Ex: Ampicillin and Amikacin 3- Synthetic – These are antibiotics that completely synthesized in the Lab. • They are designed to have greater effectiveness and less toxicity. Ex: Moxifloxacin and Norfloxacin NOTES: Most of the natural antibiotics are isolated from soil microorganisms. Natural antibiotics are often more toxic than synthetic antibiotics. 3 Antibiotic spectrum • It is the field of antibacterial activity of the antibiotic or the range of microorganisms that affected by the antibiotic. So there are 2 types of antibiotic spectrum: 1) Narrow spectrum antibiotics: • These are antibiotics which act against limited range of microorganisms. • Ex: Penicillin G is a narrow spectrum drug as it is only effective against Gram +ve bacteria. 2) Broad (wide) spectrum antibiotics: • These are antibiotics which act on wide range of microorganisms either Gram +ve or Gram –ve bacteria. • Ex: Tetracyclines are broad spectrum drugs as they are effective against Gram +ve and Gram -ve bacteria. NOTES: o No antibiotic is effective against all microbes. o There is no relation between spectrum of an antibiotic and its efficacy or potency (ie. narrow spectrum antibiotics are weak and broad spectrum are strong is a not true thinking) 4 Action of Antibiotics 1) Bacteriostatic antibiotics: • These are antibiotics which prevent the growth and multiplication of bacteria. • Bacteriostatic antibiotics give the chance for natural immunity to deal with the microbes SO they are given to patients with good immune status. • Ex: Sulfonamides, Tetracycline, Chloramphenicol. 2) Bactericidal antibiotics: • These are antibiotics which kill bacteria. • Bactericidial antibiotics may lead to release of toxins and other microbial contents leading to subsequent illness and inflammatory responses. • Ex: Penicillins, Cephalosporins, Streptomycine. NOTES: o Minimal Inhibitory Concentration (MIC) = The lowest concentration of antibiotic that inhibits the growth of the bacterial population. o Minimal Bactericidal Concentration (MBC) = The lowest concentration of antibiotic that kills the bacterial population 5 What is the Ideal Antibiotic? 6 7 Antibiotic Targets • Antibiotic targets can be divided into 5 major sites: 1- Bacterial nucleic acids 2- Bacterial metabolism 3- Bacterial ribosomes or bacterial proteins 4- Bacterial plasma membrane 5- Bacterial cell wall 8 MOA of Antibiotics 1) Inhibition of nucleic acid synthesis: Ex: Quinolones. Topoisomerase enzymes, especially topoisomerase II (DNA gyrase) relaxes the supercoiled DNA molecules of the bacterial cell. Relaxation of the supercoiled DNA molecules allows the DNA strands to be replicated by DNA polymerase enzyme. ► Quinolones acts by inhibition of DNA-gyrase enzyme, so prevent relaxation of the supercoiled DNA molecules of the bacterial cell and consequently inhibit the synthesis or replication of DNA. NOTES: Topoisomerase enzymes are present in both prokaryotic (bacteria) and eukaryotic (human) cells, but the quinolones are specific inhibitors of bacterial topoisomerase II. Inhibitors that are effective against human topoisomerase enzymes, such as etoposide, are used as anticancer drugs to kill cancer cells 9 2) Interfering with the bacterial metabolism: Ex: Sulfonamides Para-aminobenzoic acid (PABA) is utilized by bacteria and converted into dihydrofolic acid by dihydropteroate synthetase enzyme. Dihydrofolic acid converted by dihydrofolate reductase enzyme into tetrahydrofolic acid, then to purines which are essential for synthesis of nucleic acids (DNA) of the bacterial cell. Due to the chemical similarity between sulfonamides and PABA, bacteria utilize sulfonamides instead of PABA, so prevent the synthesis of dihydrofolic acid and block the synthesis of DNA of bacterial cell. 10 3) Inhibition of protein synthesis: Proteins that synthesized by ribosomes are needed for growth, multiplication & other vital activities of bacteria. Antibiotics act at different sites on bacterial ribosomes. o Aminoglycosides (Streptomycin, neomycin, gentamicin) and tetracycline bind to the 30S ribosome causing misreading of mRNA. o Chloramphenicol, Macrolides (Erythromycin) and Lincosamides (Clindamycin) binds to the 50S ribosome so interfere with the process of amino acids polymerization and result in synthesis of non-functional or defective protein. Defective protein fails to function correctly. NOTE: The selective toxicity of these antibiotics is low as bacterial ribosomes are similar to the mitochondrial ribosomes of human cells. 11 4) Interfering with the permeability of cell membrane: o Ex: Polymyxin. The cell membrane of bacteria have a certain permeability to control and protect the internal composition of the bacterial cell. Polymyxin attached to the cell membrane and interfere with its permeability, so the bacterial contents can escape causing bacteriolysis. Polymyxin is very toxic as there is little differences between human and bacterial cell membrane. ► So, it used as the last option. NOTE: Antibiotics that interfere with cell membrane function show the least degree of selective toxicity. 12 5) Inhibition of cell wall synthesis: The bacterial cell wall is located outside of the cell membrane. This wall is tough and rigid giving protection to the bacterial cell against the possible osmotic damage. The cell wall is made up of the peptidoglycan molecules: NAG and NAM. o NAG = N-acetylglucosamine o NAM = N-acetyl muramic acid At the final step of cell wall synthesis, cross-linking of NAG and NAM is completed through the activity transpeptidase enzyme. β-Lactam antibiotics (Penicillins and cephalosporins) inhibit the transpeptidase enzyme so interfere with the process of cross-linking between NAG and NAM leading to rupture of the bacterial cell due to osmotic damage. 13 NOTES: o Cell wall is absent in human cells, so antibiotic which destruct the cell wall has high selective toxicity i.e toxic only to the bacteria and is non toxic to human. o Drugs that affect the bacterial cell wall are active only against young, actively growing microbes. 14 Failure of antibiotic therapy Antibiotic treatment is considered a failure if no response is seen within 3 days. Failure may be due to various causes: 1. Wrong diagnosis (a viral infection does not respond to antibiotics). 2. Wrong choice of antibiotic. 3. Wrong dosage . 4. Development of resistance during therapy. 15 Side (adverse) effects of antibiotics Antibacterials are screened for any negative effects on humans before approval for clinical use SO they are usually considered safe. However, some antibacterials have been associated with a range of adverse effects. Side effects of the antibiotics are the unwanted reactions that occur during the medication period. Antibiotic side effects are extremely variable from patient to patient and from antibiotic to antibiotic. Side-effects include: І. Allergic reactions ІІ. Toxic reactions ІІІ. Superinfection 16 I- Allergic reactions Allergic reactions may be mild or serious. 1. Mild allergic reactions: a- Allergic dermatitis: Occurs by using of topical antibiotics. The treated area of skin appears red, swollen and itchy. b- Urticaria: Urticaria is raised itchy rashes that appears on the skin after using of systemic antibiotics. The rashes are often red and can be limited to one part of the body or spread through large areas. In addition, some blisters may appears around the mouth. 17 2. Serious allergic reactions: a- Angioedema: It is the swelling of the body tissues. Lips, tongue, and eyelids may also swell. b- Anaphylaxis: (Anaphylactic shock) It is the most severe form of allergic reactions and is potentially life threatening. Usually occurs within 20 minutes to 2 hours of exposure to the drug due to massive release of histamine. The symptoms include hypotension, bronchial asthma and skin rash. Anaphylaxis is an emergency case so it must be treated immediately. 18 How is an allergic reaction treated? a- Simple rashes are treated with antihistamines and/or corticosteroids to reduce itching and redness. b- Anaphylactic shock is generally treated with injectable epinephrine and/ or antihistaminics. ІІ. Toxic reactions a- Nephrotoxicity • Antibiotics that are metabolized and excreted in the kidney most frequently cause kidney damage. b- CNS toxicity • When drugs can pass through the brain barrier and accumulate in the nervous tissues, they can interfere with neuronal function. 19 III. Superinfection Broad-spectrum antibiotics may change the normal balance of microflora in the GIT and vagina leading to overgrowth of certain pathogens. 1- Antibiotic-associated diarrhea: 5 to 25% of patients may develop diarrhea following antibiotic medication due to destruction of the normal gut flora by the antibiotic and results in overgrowth of Clostridium sp. The most common antibiotics implicated in antibiotic-associated diarrhea are amoxicillin and ampicillin. 2- Vaginal and Oral thrush: (Candidiasis) Candida albicans is a fungus present normally in small populations in the vagina and mouth and does not normally induce disease or symptoms. Using of some broad-spectrum antibiotics kills bacterial species leading to overgrowth of Candida albicans in vagina and oral cavity causing thrush. o The symptoms of vaginal thrush include itching, pain and vaginal discharges. o In oral thrush, some white patches are visible. 20