Title of Presentation - Collaborative Family Healthcare Association
advertisement

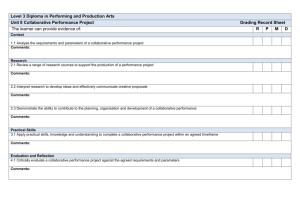
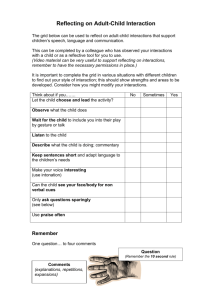
Session #A1b Friday, October 11, 2013 Collaborative Reflecting Teams in Healthcare Education Lana Kim, PhD, Assistant Professor, Marriage & Family Therapy, Valdosta State University Barbara Couden Hernandez, PhD, Professor, School of Medicine, Director of Physician Vitality, Loma Linda University Collaborative Family Healthcare Association 15th Annual Conference October 10-12, 2013 Broomfield, Colorado U.S.A. Faculty Disclosure Please include ONE of the following statements: I/We have not had any relevant financial relationships during the past 12 months. Objectives • Explain how reflecting teams function according to Tom Andersen • Identify common issues in medical or healthcare provider education that require emotional intelligence and experiential learning to perform well • Engage as a reflecting team member in a Collaborative Reflective Team Training • Describe outcome data from Collaborative Reflective Team Trainings Learning Assessment 1. Identify one common issue in healthcare provider education for which collaborative reflecting teams (CRT) would be beneficial? 2. Name the three reflection categories 3. What are some common healthcare education goals for which CRT would not be recommended? Simulation Learning I hear and I forget I see and I remember I do and I understand -Chinese Proverb Self-Reflection “Personal security facilitates self-disclosure, openness to feedback, & the risk-taking behaviors necessary to learning and professional growth.” –Lee & Everett, 2004 Reflection Categories Curiosity • Describe strengths observed • Be specific Validation • State what you wondered about …the process …the people • How were you impacted by what you observed? • Reactions, ideas, hypotheses Speculation PROTECTED LISTENING SPACE SPATIAL SEPARATION & SEQUENCED DIALOGUE Primary Learners Reflecting Team Variations • • • • Fishbowl Intermittent reflection Bug-in-the-ear Adaptable for teaching, treatment, and supervision. Contraindications • Not recommended for: – Testing (i.e. OSCE) – Assessment/evaluation – Skills training – Knowledge acquisition Summary • Protected communication increases psychological/emotional safety: Increases buy-in and engagement of learners by decreasing defensiveness. • Collaborative learning, expand perspectives, learner competency, and growth. • Facilitates deeper levels of group learning with focus away from checklist evaluation. • Clear need for guidelines given popular appeal of the format and likelihood that it may be used without sufficient training (Hoffman, 1993). • Reflecting processes are useful for situations in which strong feelings such as anger, fear, and anxiety are experienced. (Kjellberg, E., Edwardsson, M., Niemela, & Oberg. T., 1995) References • • • • • • • • • Andersen, T. (1991). The reflecting team: Dialogue and dialogues about the dialogues. New York: WW Norton. Fanning, R.M., & Gaba, D.M. (2007). The role of debriefing in simulation-based learning. The Journal of the Society for Simulation in Healthcare, 2(2), 115-125. Hernandez, B., & Kim, L. (Accepted book chapter). Collaborative reflective trainings (CRT) for mental health clinicians and physicians. In R.A. Bean, S. Davis, & M.P. Davey (Eds.), Clinical Supervision Activities for Increasing Competence and Self-Awareness. Hertel, J.P., & Millis, B.J. (2002). Using simulations to promote learning in higher education: An introduction. Sterling, VA: Stylus Publishing. Hoffman, L. (1993). Exchanging voices: A collaborative approach to family therapy. London: H. Karnac Books. Kjellberg, E., Edwardsson, M., Niemela, & Oberg. T. (1995). Using the reflecting process with families stuck in violence and child abuse. In: S. Friedman (Ed.), The Reflecting Team in Action. New York: Guilford Press. Lederman, L.C. (1984). Debriefing: A critical reexamination of the post-experience analystic process with implications for its effective use. Simul Games, 15, 415-431. Savoldelli, G.L., Naik, V.N., & Hamstra, S.J. (2005). Barriers to the use of simulation-based education. Canadian Journal of Anesthesiology, 52, 944-950. Stafford, F. (2005). The significance of de-roling and debriefing in training medical students using simulation to train medical students. Medical Education, 39, 1083-1085. Session Evaluation Please complete and return the evaluation form to the classroom monitor before leaving this session. Thank you!