Document
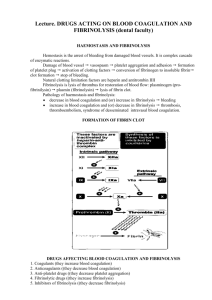
advertisement

HAEMOSTASIS & FIBRINOLYSIS DR B L Mtinangi DEPARTMENT OF PHYSIOLOGY Hubert Kairuki Memorial University December 3, 2015 HEAMOSTASIS & FIBRINOLYSIS 1 A SUMMARY OF PLATELETS FORMATION HEAMOSTASIS & FIBRINOLYSIS 2 SUMMARY OF BLOOD COAGULATION BV Injury Contact/ Tissue Factor Neural Blood Vessel Constriction Platelet Aggregation Coagulation Cascade Primary hemostatic plug Reduced Platelet Activation Blood flow Stable Hemostatic Plug Fibrin formation HEAMOSTASIS & FIBRINOLYSIS 7 HAEMOSTATIS Haemostasis is prevention of blood loss after rupture or injury/trauma of blood vessels It is achieved through: – Vascular spasms – Formation of platelet plug formation – Blood coagulation i.e. Development of insoluble fibrin clot – Clot retraction – Clot dissolution HEAMOSTASIS & FIBRINOLYSIS 8 Vascular spasms (vasoconstriction) Vascular spasms is due to: – Nervious reflex due to pain – Effects of local and humoral mechanism – Thromboxane A2 (prostaglandin) cause vasoconstrition All generate an Action Potential and cause Myogenic spasm (constriction) and REDUCE blood flow The spasm last less than 1 min HEAMOSTASIS & FIBRINOLYSIS 9 FORMATION OF PLATELET PLUG Initiated when the platelet come into contact with damaged vascular surface or collagen fibers Platelets adhere and aggregate to the damaged site Platelets secrete large quantity of ADP and Thromboxane A2 (prostaglandin) Endothetal cells secrete a Von Willebrands factor (a small protein molecule) – Usually attached to factor VIII – Bridges the platelets to exposed collagen HEAMOSTASIS & FIBRINOLYSIS 10 CONT. Aggregated platelets activate coagulation factors Finally convert FIBRINOGEN to FIBRIN – Stabilizing the PLATELET PLUG Platelets normal count 150,000400,000/µl Platelets maintain normal vascular integrity HEAMOSTASIS & FIBRINOLYSIS 11 MECHANISMS OF BLOOD COAGULATION Two mechanisms 1. Procoagulant-promote coagulation Predominate during injury 2. Anti coagulant – inhibit coagulation In normal condition it is predominat HEAMOSTASIS & FIBRINOLYSIS 12 CLOTTING FACTORS AND THEIR ROMANS SYNONYMS Fibrinogen: factor I Prothrombin: factor II Tissue thromboplastin: factor III Calcium: factor IV Proaccelerin: (labile factor V) Prothrombin: factor VII Antihaemophilic: factor (AHF VIII) Plasma thromboplastin component PTC: factor IX HEAMOSTASIS & FIBRINOLYSIS 13 CONT. Stuart: factor X Plasma thromboplastin antecedent PTA: factor XI Hegman factor XII (contact factor) Fibrin stabilizing: factor XIII NB: Factor II, VII, IX & X requires vit K for their synthesis IN THE LIVER, therefore Vit K deficiency & liver diseases leads to bleeding tendencies HEAMOSTASIS & FIBRINOLYSIS 14 Trivial Name(s) Pathway Prekallikrein Fletcher factor Intrinsic High molecular weight kininogen (HMWK) contact activation cofactor; Fitzgerald, Flaujeac Williams factor Intrinsi c I Fibrinogen Both II Prothrombin Both III Tissue Factor Extrins ic IV Calcium Both V Proaccelerin, labile factor, accelerator (Ac-) globulin Both VI (Va) Accelerin VII Proconvertin, serum prothrombin conversion accelerator (SPCA), cothromboplastin Antihemophiliac factor A, antihemophilic globulin (AHG) Factor VIII Characteristic - Contains N-term. gla segment - Protein cofactor This is Va, redundant to Factor V Extrins ic Endopeptidase with gla residues Intrinsi c Protein cofactor IX Christmas Factor, antihemophilic factor B,plasma thromboplastin component (PTC) Intrinsi c Endopeptidase with gla residues X Stuart-Prower Factor Both Endopeptidase with gla residues XI Plasma thromboplastin antecedent (PTA) Intrinsi c Endopeptidase XII Hageman Factor Intrinsi c Endopeptidase XIII Protransglutaminase, fibrin stabilizing factor (FSF), fibrinoligase Both Transpeptidase HEAMOSTASIS & FIBRINOLYSIS 15 INITIATION OF COAGULATION Initiation of coagulation by either: 1. Trauma/injury to the tissue – extrinsic pathway 2. Trauma/injury to the blood – intrinsic pathway 3. Contact of blood with damaged endothelial and collagen HEAMOSTASIS & FIBRINOLYSIS 16 A SUMMARY OF COAGULATION PATHWAY HEAMOSTASIS & FIBRINOLYSIS 19 COAGULATION is also regulated by several natural anticoagulants Antithrombin III inactivate coagulation factors& it neutralizes thrombin Antithrombin III activity is enhanced by heparin Protein C receptor combine thrombomodulin – inhibits thrombin and several coagulation factors Protein S accelerate the action of protein C Deficiency of the above factors leads to HYPERCOAGULOPATHY states leading to increased THROMBOEMBOLISM HEAMOSTASIS & FIBRINOLYSIS 20 CLOT RETRACTION Clot retraction requires large numbers of platelets ie consolidate the clot This contributes to haemostasis by joining the edges of the broken vessels HEAMOSTASIS & FIBRINOLYSIS 21 HEAMOSTASIS & FIBRINOLYSIS 22 SUMMARY OF FIBRINOLYSIS FIBRINOLYSIS (CLOT DISSOLUTION) Dissolution of a blood clot begins shortly after its formation Plasma – contains a globulin PLASMINOGEN incooperated in a large amount in the CLOT PLASMINOGEN is activated by Thrombin, factor XIII, and some lysosomal enzymes to PLASMIN with A PROTEOLYTIC like action HEAMOSTASIS & FIBRINOLYSIS 24 PLASMIN Plasmin digest formed fibrin thread/clot (FIBRINOLYSIS) Plasmin also digest a number of clotting factors like Factor I, II, V & VII alpha2 antiplasmin is always present in blood which Binds with plasmin and inhibit its action Fibrinolysis system is therefore important for removing small clot from tiny peripheral vessels-preventing occlusion or blockage and thromboembolism HEAMOSTASIS & FIBRINOLYSIS 25 Thank you HEAMOSTASIS & FIBRINOLYSIS 26