Community Health Centers - Coastal Resource and Resiliency Center
advertisement

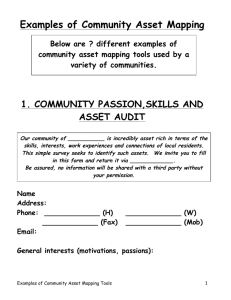
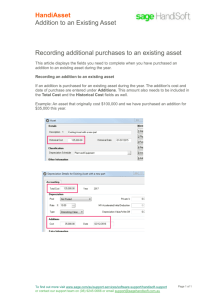
COMMUNITY HEALTH WORKER: HEALTH SERVICES & CARE Earl Nupsius Benjamin, MHA Introduction Public Health Disaster Management Community Organizing/ Planning Mental Health Health System Case Management Barriers to Use/Access to Health Care Cultural Competency Health Interventions: The Health Belief Model Desired Outcomes Understand the role of community health centers Be able to better understand health service coordination Begin to understand the tools of community asset mapping Identify community health resources and existing health services PRIMARY CARE What is Primary Care? 1961: Institute of Medicine Primary care is the activity of a health care provider who acts as an entry point into the health care system for all patients. Primary care is comprehensive, collaborative, coordinated, continuous and inclusive. Challenges in Primary Care Delivering all evidence-based guidelines for preventive and chronic disease care has been estimated to take 18 hours a day for an average sized patient panel. (Yarnall et al 2009; Alexander et al 2005) Most physicians only deliver 55% of recommended care, 42% report not having enough time with their patients. (Center for Studying Health System Change 2008; Bodenheimer & Laing 2007) Providers are spending 13% of their day in care coordination and only using their medical knowledge 50% of the time. (Gottschalk 2005; Margolis & Bodenheimer 2010) Patient care is fragmented and patients are dissatisfied with the level of attention they receive in primary care. (Bodenheimer 2008) More not less primary care is needed especially with more people becoming insured under the Affordable Care Act (ACA) The Primary Care Crisis National shortage of Primary Care Providers In 1998, half of internal medicine residents chose primary care; currently, about 80 percent become subspecialists or hospitalists This is occurring at a time when more, not fewer primary care providers (PCPs) are needed Current State of Primary Care Rushed practitioners who keep being asked to take on more responsibility Patients receiving inconsistent care Lack of care coordination Lack of active follow-up to ensure the best outcomes Patients inadequately trained to manage their condition More patients obtaining access to primary care under ACA What’s Wrong with Primary Care? Not enough time for providers to perform tasks Too much to remember Too many tasks not reimbursed Too many non-provider tasks Poor health outcomes Providers and patients are left dissatisfied… What can be done? Redesign how Primary Care is delivered The Patient Centered Medical Home Enhancing knowledge and skills of all team members Having the right mix of team members Highly organized and appropriately standardized office workflows and processes Providing ongoing training support Using technology Engaging patients and families 10 HEALTH CENTERS Do you know what community health centers are? No. 2. Yes. 3. I think I do. 1. 0% 1 0% 2 0% 3 Have you ever used a community health center’s services? No. 2. Yes. 3. I think I have. 1. 0% 1 0% 2 0% 3 Do you have a community health center[s] in your community? No. 2. Yes. 3. I think I do. 1. 0% 1 0% 2 0% 3 What is a Health Center? Health centers are community-based and patientdirected organizations that serve populations with limited access to health care. Types of Health Centers Grant-Supported Federally Qualified Health Centers (FQHC) are public and private non-profit health care organizations that meet certain criteria under the Medicare and Medicaid Programs Non-grant-supported Health Centers are health centers that have been identified by HRSA and certified by the Centers for Medicare and Medicaid Services as meeting the definition of “health center”. They do not receive grant funding under Section 330. They are referred to as "look-alikes." Outpatient health programs/facilities operated by tribal organizations (under the Indian Self-Determination Act, P.L. 96-638) or urban Indian organizations (under the Indian Health Care Improvement Act, P.L. 94-437). Health Center Program Fundamentals Located in or serve a high need community (designated Medically Underserved Area or Population). Governed by a community board composed of a majority (51% or more) of health center patients who represent the population served. Provide comprehensive primary health care services as well as supportive services (education, translation and transportation, etc.) that promote access to health care. Provide services available to all with fees adjusted based on ability to pay. Meet other performance and accountability requirements regarding administrative, clinical, and financial operations. Community Health Centers: Their Role & Reach In 2009, they served over 20 million patients at over 8,000 sites, including 941,000 migrant/seasonal farm worker patients and 1 million homeless patients. Their patients typically are without access to other health care settings: low-income people, the uninsured, those with limited English proficiency, migrant and seasonal farm workers, individuals and families experiencing homelessness, and those living in public housing. …Their Role & Reach - Continued Today, approximately 1,200 health centers operate nearly 9,000 service delivery sites that provide care to over 20 million patients This network of health centers has created one of the largest safety net systems of primary and preventive care in the country with a true national impact. The Affordable Care Act: The Essential Role of Community Health Centers The Affordable Care Act established the Community Health Center Fund that provides $11 billion over 5 a year period for the operation, expansion, and construction of health centers throughout the Nation. $9.5 billion is targeted to: support ongoing health center operations, create new health center sites and expand preventive and primary health care services. Health centers will focus more on coordinating primary and preventive services or a “medical home”. Community Health Resources (Activity) PATIENT-CENTERED MEDICAL HOME & COMMUNITYCENTERED HEALTH HOME Coordinated Care Patient-Center Medical Home (PCMH) Community-Centered Health Home (CCHH) Along Comes Patient Centered Medical Home… A model of care where each patient has an ongoing relationship with a personal physician/provider who leads a team that takes collective responsibility for all aspects of the patient’s care Examples of best practices from successful physician office practices combined with theory and vision of how care ought to be delivered Reinforces the importance of all team members 24 Core Concepts for the Patient Centered Medical Home • Each patient assigned a personal physician/physician extender • Whole person orientation • Coordinated , integrated across settings • Quality and safety emphasis • Enhanced access to care • Utilizing performance measures; how well they are fairing with quality measures Team-based care: MD/NP/PA Medical Assistant/RN Office Staff Care Coordinator Nutritionist/Educator Pharmacist Behavioral Health Case Manager Social Worker Community resources CHWs (and others) 25 Along Comes Patient Centered YOUMedical Home… Other Care A model of care where each patient has an ongoing relationship with a personal physician/provider who leads a team that takes collective responsibility for all aspects of the patient’s care Examples of best practices from successful physician office practices combined theory and vision of how YOU with (CHW) care ought to be delivered Reinforces the importance of all team members and supports the value of medical assistants (YAY!) YOU 26 Value of PCMH • Demonstration Projects – Reduced hospitalization rates 6-19% – Reduced ER visits 0-29% – Increased savings per patient $71-$640 Source: Fields, et al. 2010 • Other Benefits – Less staff burnout (10% in PCMH practices compared to 30% in controls) – Reduced cost of care (29% fewer ER visits, 6% fewer hospitalizations, estimated saving of $10.30/patient/month – Improved patient experience – Improved patient outcomes Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C, Soman MP, Trescott CE, Erikson M, Larson EB. The Group Health Medical Home At Year Two: Cost Savings, Higher Patient Satisfaction, And Less Burnout For Provider. Health Affairs 29:5 (2010): 835-843 27 PCMH Essential Skills Essential Skills enable people to perform tasks required by their jobs as well as adapt to change Patient Centered/Whole person care Practice-based learning Communication & Professionalism Teamwork Chronic disease management Practice & Population Management Coordination & Transitions of Care Integration of Care Quality, Performance, & Practice Improvement Information Technology Behavioral Health 28 What is distinctive about CHWs? Community Health Workers: Do not provide clinical care Generally do not hold another professional license Have expertise based on shared culture and life experience with population served Rely on relationships and trust more than on clinical expertise Relate to community members as peers rather than purely as client Can achieve certain results that other professionals can't (or won't) Community Health Workers - Continued CHWs have shown promise in addressing many highpriority concerns in public health and health care for the underserved. They have proven impact in important areas such as: Access to care Prenatal/perinatal care Chronic disease management Long term care (in support of home- and community-based care) Utilization of services, especially reducing inappropriate use of the ER CHW roles in the PCMH In partnership with medical professionals, a CHW can serve as the team member with expertise in cultural factors and social determinants. Facilitate patient-provider communication Spend more time with patient and family, including home visits Facilitate more complete patient-provider communication (candor), potentially making diagnosis and treatment more efficient and effective Communicate more frequently and continuously with patients Reduce numbers of patients “lost to follow-up” Improve care transitions and help reduce hospital readmissions Why Health Centers should care about CHWs Effective PCMHs will have to maintain a higher level of patient-provider communication in terms of openness/candor and also continuity. CHWs are key to this happening. Community-Centered Health Homes The community-centered health home provides high quality health care services while also applying diagnostic and critical thinking skills to the underlying factors that shape patterns of injury and illness. By strategically engaging in efforts to improve community environments, CCHHs seek to improve the health and safety of their patient population, improve health equity, and reduce the need for medical treatment. Community-Centered Health Homes – Continued The Importance of Community Prevention Community prevention is integral to effective health reform. It reduces the burden placed on the health system by reducing rates of preventable injury and illness and better aligning resources to address the factors that shape health and safety outcomes. Prevention can substantially diminish health inequities by focusing attention on unhealthy policies and inequitable resource distribution and improving community environments. Inquiry Assessment Action Elements of the CCHH: Possible Roles for the CHW Inquiry elements – Collect data on social, economic, and community conditions Analysis elements - Identify priorities and strategies with community partners Action elements – 1.) Coordinate activity with community partners 2.) Advocate for community health 3.) Mobilize patient populations A HEALTH CARE FACILITY IN YOUR COMMUNITY SAW THAT MANY OF ITS PATIENTS WERE DIABETIC. THE FACILITY IS NOW INVOLVED IN COMMUNITY PLANNING PROCESSES THAT ARE FOCUSED ON REDUCING THE NUMBER OF PEOPLE SUFFERING FROM DIABETES AND OTHER CHRONIC ILLNESSES. IS THIS SCENARIO AN EXAMPLE OF A COMMUNITY-CENTERED HEALTH HOME? 1. 2. 3. No. Yes. I do not know 0% 1 0% 2 0% 3 YOU COMMUNITY ASSET MAPPING Community Asset Mapping Asset mapping is an inventory of the businesses, organizations, and institutions that help create a community. A community asset is a quality, person, or thing that is an advantage, a resource, or an item of value to an organization or community. There are three levels of assets: Level 1 – Gifts, skills, and capacities of the individuals living in the community. Level 2 – Citizens’ organizations/networks through which local people pursue common goals. Level 3 – Institutions present in the community, such as local government, hospitals, education, and human service agencies. Community Asset Mapping – Continued Community Asset Chart Individual Skills Talents Experiences Professional Personal Resources Leadership Networks Institutional Churches Colleges and universities Elderly care facilities Police/Fire department Hospitals and clinics Mental health facilities Libraries Schools Transportation Governmental State/City/Local government Federal government agencies Bureau of Land Management Economic development Military facilities Small Business Administration State education agency Telecommunications Organizational Small and large businesses Citizen groups/Clubs Community centers Home-based enterprises Radio/TV stations Nonprofit organizations Physical/Land Utility companies Parks and recreational facilities Real estate agencies Waste management facilities Chamber of Commerce Culture Historic/Arts council groups Council for cultural affairs Tourism City council Museums Community Asset Mapping – Continued The Asset Mapping Process Phase One: Determining healthcare consumers’ needs and current resources Phase Two: Searching the healthcare consumers’ community Phase Three: Identifying potential resources Phase Four: Verifying asset mapping results Phase Five: Share asset mapping results with the community Community Asset Mapping (Activity) Reflection Summary