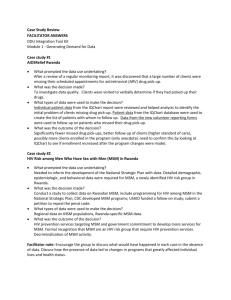
Countdown to 2015 for Maternal, Newborn & Child Survival
advertisement

Caring for the Whole Person: Comprehensive Health Services for MSM Kenneth H Mayer, Linda-Gail Bekker, Andrew Grulich, Ron Stall, Grant Colfax, Javier R Lama Fenway Health/Beth Israel Deaconess Medical Center, USA Desmond Tutu AIDS Foundation, S Africa Kirby Institute, UNSW, Australia University of Pittsburgh, USA San Francisco Dept of Health, USA IMPACTA, Peru 2012 Structure of the Article • Reviewed medical work published in English between Jan, 1977 and Jan, 2012 related to MSM • Searched PubMed and Google Scholar with the key terms related to MSM and specific clinical issues • Reviewed more than 1000 articles, preferentially choosing systematic reviews, papers with new data, or recently published work • Life course perspective, focused on factors that can be changed to decrease HIV risk • Assessed structural issues influencing health disparities Introduction • Although MSM existed in societies throughout history, AIDS created awareness of health concerns • Programs that dealt with emergencies transitioned to the provision of chronic care post-HAART • Increased recognition of MSM and other LGBT health disparities • Recent research has increased recognition that homophobia has health consequences • Recent research has documented enhanced health disparities for MSM living in LDCs (Mayer, AJPH, 2008; Stall, AJPH, 2003; Safren, J Consult Clin Psych, 1999; Almeida, J Youth Adolesc, 2009; Beyrer, STI, 2008) MSM are heterogeneous Growing Up and Coming Out • Same sex behavior and gender non-comformity remains stigmatized in most societies • Societal messages remind MSM Youth they are not accepted (e.g. marriage pressure, exclusion from military) • MSM Youth may encounter loss of friends, non-support from families, religious abandonment, and verbal or physical abuse, resulting in adverse health outcomes • External stigma may → internalized homophobia → depression, substance use • Sexual expression is happening earlier (Harrison, J Sch Health, 2003; Drasin, J Homosex, 2008; D’Augelli, Clin Child Pysch, 2002; Grov, J Sex Res, 2006) Growing Up and Coming Out • Self-acceptance can lead to early identity integration, disclosure and adaptation of safer practices; adverse experiences impair identity formation and behavior • In the U.S. Black and Latino Youth were less comfortable with disclosing their MSM identity; Role of dual stigma? • Youth experiencing homophobic bullying may withdraw from school • In some countries, homophobic laws may impede successful development • Having supportive conversations with adults and role models may lead to successful maturation (Merighi, Jour Contemp Human Serv, 2000; Butler, J Homosex, 2008; Rosario, Cult Divers Ethnic Minor Psych, 2004; Murdock, Psych in the School, 2005; Beyrer, Epidemiol Rev, 2010) Life Course Development • Some MSM experience syndemics, i.e. increased risk for depression, substance use, sexual risk and HIV • Internalization of homophobic and domestic violence plays a role in syndemic formation • Despite the stressors MSM experience, the majority are not depressed and are not using substances • Factors that enhance resilience need to be better understood (Stall, Addiction, 2001; Mills, Am J Psych, 2004; Greenwood, AJPH, 2002; Mustanski, Ann Behav Med, 2007; Friedman, AIDS and Behavior, 2008) Resilience in the Face of Stressors: Majority of MSM are not infected or risk taking No. of Psychosocial Health Problems* 0 (n = 1,392) 1 (n = 812) 2 (n = 341) 3 or 4 (n = 129) Recent high risk sex 7% 11% 16% 23% HIV prevalence 13% 21% 27% 22% All associations have p’s < 0.001. All p values are two-tailed. From Stall et al., 2003 * Childhood sexual abuse, depression, substance use, intimate partner violence Sexual Health • Not just absence of disease, but also safe and pleasurable experiences • Specific practices put MSM at risk for diverse STDs • Anal sex: HIV, rectal GC/CT, HBV, HPV, HSV Anal trauma may →HCV Oral sex: Syphilis; Penile sex: HPV, HSV Saliva: CMV, EBV, HBV, HHV-8 Oral-anal: enteric pathogens, HAV,HBV Abraded skin: MRSA • Some MSM may not be individually risky, but select partners from high prevalence pools (e.g. Black MSM in the US) (Wolitski, AIDS Behav, 2011; Hart, Current Op Infect Dis, 2009; Grulich, Austral NZ J Public Health, 2003; Jin, AIDS, 2010; Abdolrasouli, Sex Health, 2009; Cohen, STI, 2004; Tohme, Hepatology, 2010; Jin, STI, 2007) Infectious Diseases • Syphilis: ↑ associated with HIV+ serosorting and SU • GC and CT: Need to test with NAAT in order to detect frequently asymptomatic rectal infections • Increasing MDR GC, including quinolone resistance • HSV2: More common among MSM and facilitates HIV transmission. Acyclovir prophylaxis was not effective • Hepatitis A/B, HPV vaccination should be standard of care, Hepatitis C screening also indicated • HPV: Vaccine preventable neoplasia; Frequency of anal cytology screening needs further clarification (Heffelfinger, AJPH, 2007; Kalichman, STI, 2011; Buchacz, AIDS, 2004; Kent, Clin Inf Dis, 2003; Annan, STI, 2009; Gunn, STD, 2007; Taylor, Clin Inf Dis, 2011; Szumowski, Clin Inf Dis, 2009; Chin-Hong, J National Cancer Inst, 2005; Workowski, MMWR, 2010; Moreira, Hum Vaccin, 2011; Cranston, STI, 2008; Kaplan, MMWR, 2009) Mental Health Issues • 40% of MSM become depressed, 2X the lifetime rate of heterosexual men • Predictors of major depression are: not having a partner, experiencing anti-gay threats or violence, non-identification as gay • Panic disorder, social phobia, generalized anxiety disorder are more common among MSM (20% lifetime incidence) • Culturally-tailored treatment may involve groups that enhance community identification (Sandfort, Arch Gen Psych, 2001; Gilman, AJPH, 2001; Lewis, Health Place, 2010; Safren, Health Psychology, 2012) Substance Use • Many studies suggest that substance use is common among MSM • Reasons for SU include: coping with homophobia, depression/anxiety • Among SU MSM, poly-drug use is common • Rates of MSM cigarette smoking range from 27 to 66%, higher than matched controls • Heavy alcohol use (14-39%) tends to be lower than general population • Episodic recreational use is common; drug addiction is uncommon (Stall, AJPH, 1999; Ryan, Am J Prev Med, 2001; Greenwood, Drug Alcohol Dep, 2001; Ostrow, JAIDS, 2010; Mimiaga, AIDS Pt Care STDs, 2008) Substance Use • Substance use during sex is associated with HIV SC • SU may ↑ libido, sense of invulnerability; impair negotiation skills, select high risk network partners • For HIV+ MSM, SU may decrease medication adherence • For HIV- MSM, SU facilitates transmission by lowering pain thresholds, allowing for more traumatic sex, and possibly impairing host immunity • Culturally-tailored programs that include groups and/or support MSM identity, have been successful in decreasing cigarette and crystal methamphetamine use (Colfax, Lancet, 2010; van Griensven, J Int AIDS Soc, 2010; Johnston, Int J Drug Pol, 2010; Bautista, STI, 2004; Parry, Drug Alcohol Dep, 2008; Koblin, AIDS, 2006; Cochran, Sub Use Misuse, 2007; Shoptaw, J Sub Abuse Treat, 2008; Mausbach, Drug Alcohol Depend, 2007; Mansergh, PL0S Med, 2010) Non-Communicable Medical Conditions • Body image and weight: some MSM may attempt to conform to cultural ideals by increased exercise, others may “self-medicate” depression by over-eating • Medical complications of substance use: Cardiovascular and pulmonary complications of cigarettes, inhaled stimulants; alcohol potentiating liver disease • Aging issues: Many MSM age alone, partially due to social rejection of non-traditional families (Sandfort, Arch Gen Psych, 2001; Greenwood, AJPH, 2005; Mansergh, STI, 2008) Structural Changes and MSM Health • Will ↑ civil rights improve health outcomes? • ↑LGBT teen suicide in non-supportive Oregon counties compared to those with Gay-Straight student alliances • MSM at Fenway Health had ↓ medical and mental health costs after marriage equality • But HIV and STD rates are not down in Europe/U.S. Could lag be due to ↑ prevalence antedating changes in social norms? Or therapeutic optimism, or…… More data are needed (Hatzenbuehler, Pediatrics, 2011; Hatzenbuehler, AJPH, 2012) Culturally Competent Care • MSM have often received suboptimal care and have been reticent to disclose to providers because of fears of stigmatization • Many health care providers are unaware of the diversity of MSM and their different health conditions • Ironically, health care providers may be uniquely able to assist MSM in their coming out process because of their social role • Culturally-competent care is a basic human right, and is essential for optimal clinical management (Gonser, J Cult Divers, 2000; Meyer, AJPH, 2001; Mayer, AJPH, 2008; Bettancourt, Cultural Competence in Health Care, 2002) Caring for the Whole Person • MSM and other LGBT people have similar health concerns as others, as well as some additional concerns • Important to engage the whole person, not a collection of risk factors • Important to understand that LGBT life issues are similar to others, but also unique: – Families, Coming Out – Long Term Relationships – Reproduction, Parenting – Mental Health – Chronic Diseases – Communicable Diseases Thank You Steven A. Safren Conall O’Cleirigh Matthew Mimiaga Rodney Vanderwarker Harvey Makadon Judy Bradford Steve Boswell Sean Cahill Tom Mills Amy Herrick Chris Beyrer NIAID, NIMH, NIDA, NICHD, CDC, HRSA, Mass DPH