Substance abuse

Disorders Due to Psychoactive
Substance Use
Department of Psychiatry
1 st Faculty of Medicine
Charles University, Prague
Head: Prof. MUDr. Jiří Raboch, DrSc.
Psychoactive Substance
Psychoactive (psychotropic) substance is any substance which after absorption has influence on mental processes both cognitive and affective.
1.
stimulative
2.
suppressive
3.
hallucinogenic
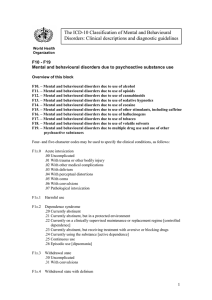
Mental and Behavioural Disorders
Due to Psychoactive Substance Use
Disorders due to use of :
F10.x alcohol
F11.x
opioids
F12.x cannabinoids
F13.x
sedatives or hypnotics
F14.x cocaine
F15.x other stimulants (caffeine)
F16.x hallucinogens
F17.x tobacco
F18.x
volatile solvents
F19.x
multiple drugs and other psychoactive drugs
Mental and Behavioural Disorders
Due to Psychoactive Substance Use
Specific Clinical Conditions:
F1x.0 Acute intoxications
F1x.1 Harmful use
F1x.2 Dependence syndrome
F1x.3 Withdrawal state
F1x.4 Withdrawal state with delirium
F1x.5 Psychotic disorder
F1x.6 Amnesic syndrome
F1x.7 Residual state, late-onset psychotic disorder
F1x.8 Other mental and behavioural disorders
F1x.9 Unspecified mental and behavioural disorder
F1x.0 Acute Intoxication
Df.:
A transient condition following the administration of psychoactive substance resulting in disturbances in level of consciousness, cognition, perception, affect or behaviour, or other psychophysiological functions and responses
Closely related to dose levels
Uncomplicated
With trauma or other medical complications
With delirium
With coma
With convulsions
Pathological intoxication (applies only to alcohol)
F1x.1 Harmful Use
The damage may be physical and/or mental.
Socially negative consequences are not evidence (neither acute intoxication or hangover).
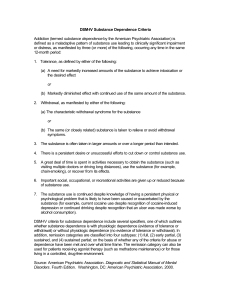
F1x.2 Dependence Syndrome
(Addiction)
a) A strong desire or sense of compulsion to take the substance („craving“) b) Difficulties in controlling substance-taking c) Withdrawal sy characteristic for the substance d) Evidence of tolerance e) Progressive neglect of pleasures and interests f) Persisting with substance use despite clear evidence of overtly harmful consequences
Physical dependence
Psychic (psychological) dependence
F1x.2 The Course of Dependence
Syndrome
F1x.20 currently abstinent (remission)
F1x.21 currently abstinent in a protected environment
F1x.22 currently abstinent on a maintenance regime
F1x.23 currently abstinent - receiving treatment with aversive or blocking drugs (naltrexone, disulfiram)
F1x.24 currently active dependence
F1x.25 continuous (chronic) use
F1x.26 episodic use (dipsomania)
F1x.3 Withdrawal State
Symptoms occurring on absolute or relative withdrawal of a substance after repeated and prolonged use of the substance
• Uncomplicated
• With convulsions
F1x.4 Withdrawal State with
Delirium
Delirium tremens - in severely dependent users with a long history of use of alcohol
Prodromal symptoms : insomnia, tremor, fears followed by illusions, hallucinations, clouding of consciousness and marked tremor
F1x.5 Psychotic Disorder
Psychotic phenomena occurring during or immediately after psychoactive substance use
Schizophrenia-like
Predominantly delusional, hallucinatory, depressive, manic (alcoholic hallucinosis, jealousy)
Persistence for more than 48 hours
F1x.6 Amnesic Syndrome
Impairment of recent memory (learning of new material)
Absence of defect in immediate recall, of impairment of consciousness, and of generalized cognitive impairment
History of chronic use of psychoactive substance (Korsakov’s psychosis or syndrome)
F1x.7
Residual and late-onset psychotic disorder
Onset related to the use of psychoactive substance, the disorder should persist beyond any period of time during which direct effects of the psychoactive substance might be assumed
Flashbacks - duration in seconds or minutes, duplication of previous drug-related experiences
Personality disorder
Dementia
F10.x Mental Disorders Due to
Use of Alcohol
Acute intoxication :
• euphoria, flushed face, ataxia, slowed reaction time, impaired motor performance, slurred speech, poor concentration; in higher doses behavioural changes – disinhibition of sexual and aggressive impulses, increased suicidal and homicidal behaviour
Pathological intoxication :
• sudden change of consciousness with aggressive behaviour and amnesia
Harmful use :
• physical complications – hypertension, arteriosclerosis, heart infarction, cardiomyopathy, brain stroke, liver cirrhosis, fatty liver, gastritis, etc.
• psychic complications - depression
F10.x Mental Disorders Due to
Use of Alcohol
Dependence syndrome:
• increased tolerance to alcohol, morning drinking, alcohol bouts, blackouts, deterioration in occupational and marital life, behavioural changes, withdrawal symptoms
Withdrawal state:
• tremor, anxiety, easy getting startled, agitation, insomnia, nausea, sweating, epileptic seizures and delirium tremens
Delirium tremens:
• usually starts in evening hours – growing tremulousness, severe agitation, anxiety and perceptual distortion
• a state seriously endangering patient's life
• recovery after several days, retrograde amnesia
F10.x Mental Disorders Due to
Use of Alcohol
Other psychotic disorders:
• alcoholic hallucinosis
• pathological jealousy
• Korsakov's psychosis
• Wernicke encephalopathy
• alcoholic dementia
Treatment of alcoholism
• Withdrawal from alcohol, benzodiazepines, clomethiazol
• Aversion therapy
• Alcohol-Antabuse (disulfiram) Reaction (AAR)
• Psychotherapy
F11.x Mental Disorders Due to
Use of Opioids
Morphine, heroin (diacetylmorphine), codeine, pethidine, methadone
Heroin :
• dependence develops within two weeks of daily use
• overdose may lead to death
• withdrawal symptoms are extremely unpleasant
• needle-sharing represents a serious risk of transmission of HIV and hepatitis B + C viruses
• treatment of the withdrawal state – buprenorphine, benzodiazepines, spasmolytics; in serious cases of dependence heroin is replaced by methadone
F12.x Mental Disorders Due to
Use of Cannabinoids
Marijuana (marihuana) is a colloquial term for dried leaves and flowers of cannabis plant (Cannabis sativa L.)
Δ 9 -tetrahydrocannabinol (Δ 9 -THC) is responsible for the psychoactive properties of the cannabis plant
Complex physiological functions of the cannabinoid system: motor coordination, memory procession, control of appetite, pain modulation and neuroprotection
Summary of adverse effects:
• acute : anxiety, panic, impaired attention, memory, reaction time and psychomotor performance and coordination, increased risk of road accident, and increased risk of psychotic symptoms among vulnerable persons
• chronic : chronic bronchitidis, a cannabis dependence syndrome, subtle impairments of attention, short-term memory and ability to organize and integrate complex information
F12.x Mental Disorders Due to
Use of Cannabinoids
Effect of cannabinoids on central nervous system:
Euphoria, enhancement of sensory perception, tachycardia, antinociception, difficulties in concentration, impairment of memory
Cannabis use may exacerbate symptoms of schizophrenia and may precipitate disorders in persons who are vulnerable to developing psychosis; heavy cannabis use may increase depressive symptoms among some users
Tolerance develops; the relatively long half-life and complex metabolism of cannabis may result in a low intense withdrawal syndrome
Marijuana use tends to impair executive function in the brain, e.g. higher risk for all types of injuries is associated with cannabis use
Cannabis abuse and dependence were highly associated with increasing risks of other substance dependence
F13.x Mental Disorders Due to
Use of Sedatives and Hypnotics
benzodiazepines – potentiate the action of
GABA risk of dependence short-acting benzodiazepines: alprazolam, flunitrazepam, oxazepam, lorazepam, temazepam long-lasting benzodiazepines: diazepam, clorazepate, chlordiazepoxide, etc.
withdrawal state can be accomplished with epileptic seizures interaction with alcohol may induce qualitative changes of consciousness
F14.x,15.x Mental Disorders
Due to Use of Stimulants
Cocaine, amphetamine, metamphetamine
(pervitine), phenmetrazine, methyphenidate,
MDMA (ecstasy, methylenedioxymetamphetamine)
Positive mood, activity, planning, diminished need of sleep
Tachycardia, arrhythmia, hypertension, hyperthermia, intracerebral haemorrhage
Withdrawal symptoms: severe craving, depression, decreased energy, fatigue, sleep disturbance
Prolonged use can trigger paranoid psychoses, impulsivity, aggressivity, irritability, suspiciousness and anxiety states
F16.x Mental Disorders Due to
Use of Hallucinogens
Lysergid acid diethylamide (LSD), psilocybin, mescaline, phencyclidine
Acute intoxication: distorted perception
(optic hallucinations and illusions); unpredictable and dangerous behaviour
Withdrawal syndrome has not been described
F18.x Mental Disorders Due to
Use of Volatile Solvents
Toluene, acetone, adhesives, petrol, cleaning fluids, etc.
Acute intoxication: euphoria, disorientation, incoordination, slurred speech; optic hallucinations
The way of use is very dangerous
Drug Addiction Treatment
HEALTH SERVICE:
acute states (detox program, tox. psychosis) weaning treatment
after-treatment care substitution (maintainance) treatment
OUT OF HEALTH SERVICE:
contact centers
daily static centers therapeutic communities after-treatment centers protected workshops and habitations mutual help groups – Alcoholics Anonymous,
Narcotics Anonymous
Links
Czech National Focal Point for Drugs and Drug Addiction: www.drogy-info.cz
European Monitoring Centre for
Drugs and Drug Addiction: http://www.emcdda.eu.int/